2-Year Results of Phase 2 Trial for Talimogene Laherparepvec in Melanoma
This study reports on the primary analysis of recurrence-free survival at 2 years for patients with resectable stage IIIB IVM1a melanoma treated with Talimogene Laherparepvec (T-VEC) neoadjuvant therapy followed by surgery compared to surgery alone. The trial evaluates the efficacy and safety of T-VEC in the neoadjuvant setting and its impact on systemic antitumor immune response. The results provide insights into the potential benefits of T-VEC in high-risk melanoma patients.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
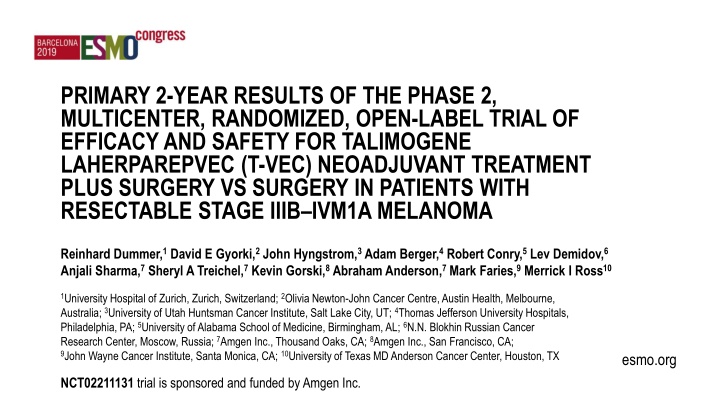
PRIMARY 2-YEAR RESULTS OF THE PHASE 2, MULTICENTER, RANDOMIZED, OPEN-LABEL TRIAL OF EFFICACY AND SAFETY FOR TALIMOGENE LAHERPAREPVEC (T-VEC) NEOADJUVANT TREATMENT PLUS SURGERY VS SURGERY IN PATIENTS WITH RESECTABLE STAGE IIIB IVM1A MELANOMA Reinhard Dummer,1David E Gyorki,2John Hyngstrom,3Adam Berger,4Robert Conry,5Lev Demidov,6 Anjali Sharma,7Sheryl A Treichel,7Kevin Gorski,8Abraham Anderson,7Mark Faries,9Merrick I Ross10 1University Hospital of Zurich, Zurich, Switzerland; 2Olivia Newton-John Cancer Centre, Austin Health, Melbourne, Australia; 3University of Utah Huntsman Cancer Institute, Salt Lake City, UT; 4Thomas Jefferson University Hospitals, Philadelphia, PA; 5University of Alabama School of Medicine, Birmingham, AL; 6N.N. Blokhin Russian Cancer Research Center, Moscow, Russia; 7Amgen Inc., Thousand Oaks, CA; 8Amgen Inc., San Francisco, CA; 9John Wayne Cancer Institute, Santa Monica, CA; 10University of Texas MD Anderson Cancer Center, Houston, TX esmo.org NCT02211131 trial is sponsored and funded by Amgen Inc.
Conflict of Interest Disclosures R Dummer has intermittent, project-focused consulting and/or advisory relationships with Novartis, Merck Sharp & Dohme (MSD), Bristol-Myers Squibb (BMS), Roche, Amgen, Takeda, Pierre Fabre, Sun Pharma, Sanofi, and Catalym outside the submitted work. DE Gyorki received travel and honorarium from Amgen Inc. J Hyngstrom is contracted by Ebix to provide written and audio reviews of general surgery research articles every 2 months for Practical Reviews of General Surgery (the author does not deem this to be relevant to content of the current publication). A Berger served on speaker s bureaus for Cardinal Health and Castle Biosciences, and advisory boards for Castle Biosciences. R Conry served on speakers bureaus for Merck, BMS, Amgen Inc., Novartis, Array, and Regeneron-Sanofi. L Demidov received research grants from Novartis, consulting fees from MSD, BMS, Novartis, Roche; served on the advisory board for Novartis; and received honorarium from MSD, BMS, Novartis, and Roche. A Sharma, SA Treichel, A Anderson, and K Gorski are employees of and stockholders in Amgen Inc. M Faries received consulting fees from Delcath Systems Inc. and served on advisory boards for Pulse Biosciences and Novartis Inc. MI Ross received honoraria from Merck and Amgen Inc.; advisory fees from Merck and Amgen Inc.; research funding from Amgen Inc. and Provectus; and travel from Merck, Amgen Inc., Provectus, Novartis, and Castle Biosciences.
Introduction Despite recent advances, the risks of recurrence and death remain high for patients with advanced stage IIIB IVM1a melanoma even after resection1,2 Talimogene laherparepvec (T-VEC) is a genetically modified herpes simplex virus-1 based immunotherapy designed to selectively replicate in tumors, produce granulocyte-macrophage colony-stimulating factor (GM-CSF), and stimulate systemic antitumor immune response3,4 T-VEC may be suitable for use in the neoadjuvant setting given the following attributes: Mechanism of action invokes systemic immune surveillance Administration requires intralesional injection into tumors This phase 2, multicenter, randomized, open-label trial evaluates neoadjuvant administration of T-VEC + surgery compared with surgery alone in high-risk patients with resectable stage IIIB IVM1a melanoma (NCT02211131)5,6 Here, we report the primary analysis of recurrence-free survival (RFS) at 2 years 1. Whitman ED, et al. Future Oncol. 2019;15:459-471. 2. McKean MA, et al. Cancer Treat Rev. 2018;70:144-153. 3. Liu BL, et al. Gene Ther. 2003;10:292-303. 4. Hu JCC, et al. Clin Cancer Res. 2006;12:6737-6747. 5. Dummer R, et al. Presented at: ASCO 2019; Chicago, IL. Abstract 9520. 6. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02211131. Accessed Sept 3, 2019.
Methods: NCT02211131 Trial Schema5 Arm 1 T-VEC Intralesional 4 mL x 106 PFU/mL; then after 3 weeks, 4 mL x 108 PFU/mL Q2W n = 75 Resectable Stage IIIB IVM1a6 Melanoma Injectable and measurable LDH 1.5 x ULN for IIIB/C and 1 x ULN for IVM1a ECOG PS 0 or 1 Prior treatment completed 3 months prior Surgical Resection Follow-up ~5 Years 1 N = 150 R : Week 13 Week 18 1 Follow-up ~5 Years Stratification: Disease stage Planned adjuvant therapy Week 1 Week 6 n = 75 Arm 2 Surgical Resection Primary Endpoint: Key Secondary Endpoints: RFS,* overall survival (OS),* overall tumor response (in Arm 1 only), pathological complete response (in Arm 1 only), rates of histopathological tumor-free (R0) surgical resection, local RFS, regional RFS, distant metastases-free survival, safety Exploratory Endpoints: Analyses of tumor tissue biomarkers and correlations with clinical outcomes for T-VEC RFS *RFS and OS at 2 years, 3 years, and 5 years. LDH, lactate dehydrogenase; ULN, upper limit of normal; PFU, plaque forming units. 5. Dummer R, et al. Presented at: ASCO 2019; Chicago, IL. Abstract 9520. 7. AJCC Cancer Staging Manual, 7th Edition. 2015.
Methods: Trial Endpoints Primary Endpoint: RFS (per protocol): RFS events were defined as local, regional, or distant recurrence (whichever occurred first) or death due to any cause after surgery in the intention-to-treat (ITT) set Patients who withdrew prior to surgery or had a non-R0 resection were counted as an RFS event at randomization RFS (sensitivity): An additional sensitivity analysis of RFS was also conducted RFS regardless of surgical margin, eg, not counting non-R0 resections as events at baseline Additional key efficacy endpoints: objective response rate (ORR) in Arm 1, R0 resection rate, and pCR rate 7. AJCC Cancer Staging Manual, 7th Edition. 2015.
Baseline Patient Characteristics Arm 1: T-VEC + Surgery (n = 76) 63.5 (34, 85) 49 (64.5) Arm 2: Surgery Alone (n = 74) 59.0 (21, 85) 47 (63.5) Age median (min, max), years Male n (%) ECOG PS n (%) 0 1 Disease stage (per current CRF)a n (%) Stage IIIB Stage IIIC Stage IVM1a BRAF mutation status n (%) Mutation Mutation not present Missing Received prior surgery n (%) Received prior radiotherapy n (%) Received prior systemic therapy for current disease n (%) Chemotherapy Immunotherapy No plans for adjuvant therapy (per IVRS) n (%) 67 (88.2) 9 (11.8) 63 (85.1) 11 (14.9) 28 (36.8) 30 (39.5) 17 (22.4) 26 (35.1) 35 (47.3) 13 (17.6) 35 (46.1) 40 (52.6) 1 (1.3) 71 (93.4) 4 (5.3) 4 (5.3) 1 (1.3) 3 (3.9) 64 (84.2) 34 (45.9) 39 (52.7) 1 (1.4) 66 (89.2) 5 (6.8) 3 (4.1) - 3 (4.1) 62 (83.8) ITT Analysis Set: 150 patients enrolled and randomized. Patients enrolled from February 2015 to April 2017 aOne patient in Arm 1 was discovered to have stage IVM1c disease after randomization. CRF, case report form.
pCR Rate With Neoadjuvant T-VEC Arm 1: T-VEC + Surgery Efficacy Analysis Set (n = 57) ITT Analysis Set (n = 76) pCRa n(%) 13 (17.1) 13 (22.8) 9 out of 13 patients with Pathological CR have not relapsed at the time of this analysis Efficacy Analysis Set: patients who received at least 1 dose of T-VEC followed by surgical resection in Arm 1, or who received surgical resection in Arm 2 ITT Analysis Set: 150 patients enrolled and randomized apCR is defined as no evidence of viable tumor cells on complete pathological evaluation of the surgical specimen per institutional standards.
2-Year RFS (Per Protocol) Arm 1 (T-VEC + Surgery, N = 76): 29.5% Arm 2 (Surgery Alone, N = 74): 16.5% Median Follow-up = 31.2 months Overall P = 0.070 Overall HR (80% CI) = 0.75 (0.58, 0.96) 100% Kaplan-Meier (KM %) 75% 50% | | ||| 25% 0% 0 3 6 9 12 15 18 21 24 27 30 33 36 39 42 45 Study Month Number of Patients at Risk: Surgery Alone T-VEC + Surgery 74 76 18 32 14 32 14 26 12 24 11 22 10 22 9 21 8 20 8 19 6 16 4 11 2 5 1 2 0 1 0 Type of RFS Event at Baseline Arm 1: T-VEC + Surgery (n = 76) Arm 2: Surgery Alone (n = 74) No surgery n (%) 18 (23.7) 4 (5.4) R1 or R2 (lack of R0) resection following surgery n (%) 25 (32.9) 41 (55.4) Total events at baseline n (%) ITT Analysis Set: 150 patients enrolled and randomized 43 (56.6) 45 (60.8)
2-Year RFS (Sensitivity Analysis) Arm 1 (T-VEC + Surgery, N = 76): 50.5% Arm 2 (Surgery Alone, N = 74): 30.2% Median Follow-up = 31.2 months Overall P= 0.038 Overall HR (80% CI) = 0.66 (0.50, 0.87) 100% Kaplan-Meier (KM %) 75% 50% 25% 0% 0 3 6 9 12 15 18 21 24 27 30 33 36 39 42 45 48 51 Study Month 19 16 37 36 Number of Patients at Risk: Surgery Alone T-VEC + Surgery 74 76 56 56 34 56 28 44 26 41 23 38 22 38 15 34 13 28 9 20 6 9 4 6 3 2 0 1 1 0 Type of RFS Event at Baseline Arm 1: T-VEC + Surgery (n = 76) Arm 2: Surgery Alone (n = 74) No surgery n (%) 18 (23.7) 4 (5.4) ITT Analysis Set: 150 patients enrolled and randomized
Improved 2-Year OS With Neoadjuvant T-VEC 100% Kaplan-Meier (KM %) 75% 50% Arm 1 (T-VEC + Surgery, N = 76): 88.9% Arm 2 (Surgery Alone, N = 74): 77.4% Median Follow-up = 31.2 months Overall P = 0.050 Overall HR (80% CI) = 0.49 (0.30, 0.79) 25% 0% 0 3 6 9 12 15 18 21 24 27 30 33 36 39 42 45 48 51 Study Month Number of Patients at Risk: Surgery Alone T-VEC + Surgery 74 76 71 73 70 71 66 70 61 69 59 69 59 68 56 65 49 60 44 53 40 44 29 36 20 22 8 16 5 4 1 3 1 1 0 0 ITT Analysis Set: 150 patients enrolled and randomized
Subsequent Anti-cancer Treatment at 2 Years Adjuvant Setting Arm 1 T-VEC + Surgery (n = 73) 65 (89.0) 8 (11.0) 6 (8.2) 6 (8.2) 2 (2.7) 2 (2.7) - 4 (5.5) - - - - - - - 1 (1.4) 1 (1.4) Metastatic Setting Arm 1 T-VEC + Surgery (n = 73) 48 (65.8) 25 (34.2) - 17 (23.3) 15 (20.5) 4 (5.5) 15 (20.5) - 2 (2.7) - 1 (1.4) - 3 (4.1) 7 (9.6) - 8 (11.0) 2 (2.7) Arm 2 Arm 2 Surgery Alone (n = 69) 48 (69.6) 21 (30.4) 14 (20.3) 14 (20.3) 8 (11.6) 4 (5.8) 5 (7.2) 7 (10.1) 1 (1.4) - - - 1 (1.4) 1 (1.4) - 8 (11.6) 1 (1.4) Surgery Alone (n = 69) 32 (46.4) 37 (53.6) - 27 (39.1) 23 (33.3) 6 (8.7) 21 (30.4) 1 (1.4) 4 (5.8) 1 (1.4) - 1 (1.4) 6 (8.7) 11 (15.9) 1 (1.4) 7 (10.1) 2 (2.9) Patients not receiving subsequent anti-cancer treatment n (%) Patients receiving subsequent anti-cancer treatment n (%) Systemic without radiotherapy Immunotherapy Checkpoint inhibitors CTLA-4 inhibitors PD-1 / PD-L1 inhibitors Cytokines Oncolytic virus Intratumoral Intravesicular Other Chemotherapy Targeted small-molecule therapy Chemo-embolization Radiotherapy only Other In patients receiving at least one dose of T-VEC or surgery. n represents the number of patients that received therapy for each category; patients may have received more than 1 category of subsequent adjuvant therapy.
Increased CD8+ Cell Density After T-VEC Treatment Is Correlated With Clinical Outcomes Arm 1: OS Stratified by Change in CD8+ Cell Density Arm 1: RFS (Sensitivity) Stratified by Change in CD8+ Cell Density 1 1 Increased CD8+ Cell Density No Change or Decreased CD8+ Cell Density 0.9 0.9 0.8 0.8 Kaplan-Meier (KM %) Kaplan-Meier (KM %) 0.7 0.7 0.6 0.6 0.5 0.5 0.4 0.4 Increased CD8+ Cell Density No Change or Decreased CD8+ Cell Density 0.3 0.3 0.2 0.2 HR = 0.21 (0.05, 0.89) P = 0.034 HR = 0.35 (0.16, 0.73) P = 0.01 0.1 0.1 0 0 0 5 10 15 20 25 30 35 40 45 50 5 10 15 20 25 30 35 40 45 50 Study Month Study Month Number of Patients at Risk: 37 16 35 16 30 7 28 5 27 3 26 3 19 3 9 0 3 2 0 37 16 37 16 37 15 37 14 36 12 35 9 27 7 20 5 4 3 3 1 0 0 In an exploratory analysis, T-VEC treatment resulted in a 3-fold increase in intratumoral CD8+ cell density (P < 0.001) and a 17-unit increase in PD-L1 expression H-score (P = 0.038) in Arm 1 CD8+ density and PD-L1 H-score were also higher in Arm 1 after T-VEC treatment compared with Arm 2 (both P < 0.001) In Arm 1, the increase in intratumoral CD8+ cell density after T-VEC treatment was correlated with longer RFS in the sensitivity analysis and with longer OS
Conclusions This is the largest randomized neoadjuvant trial of patients with resectable stage IIIB IVM1a melanoma to date As previously reported, no grade 5 TEAEs were reported in the trial and no unexpected toxicities were identified in the T-VEC + surgery arm5 Increased CD8+ cell density after neoadjuvant T-VEC treatment was correlated with clinical outcomes 2-year RFS was improved with neoadjuvant T-VEC monotherapy + surgery compared with surgery alone (RFS per protocol: overall HR: 0.75, P = 0.07; RFS sensitivity: overall HR: 0.66, P = 0.038) 2-year OS was improved in the T-VEC + surgery arm (88.9%) compared with the surgery alone arm (77.4%; overall HR: 0.49, P = 0.050) Improved clinical outcomes were not driven by subsequent anticancer therapy, including checkpoint inhibitors TEAE, treatment emergent adverse event. 5. Dummer R et al. Presented at: Annual Meeting of the American Society of Clinical Oncology (ASCO); May 31 June 04, 2019; Chicago, IL. Abstract 9520.
References 1. Whitman ED, et al. Future Oncol. 2019;15:459-471. 2. McKean MA, et al. Cancer Treat Rev. 2018;70:144-153. 3. Liu BL, et al. Gene Ther. 2003;10:292-303. 4. Hu JCC, et al. Clin Cancer Res. 2006;12:6737-6747. 5. Dummer R, et al. Presented at: Annual Meeting of the American Society of Clinical Oncology (ASCO); May 31 June 04, 2019; Chicago, IL. Abstract 9520. 6. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02211131. Accessed Sept 3, 2019. 7. AJCC Cancer Staging Manual, 7th Edition. 2015. 8. Ribas A, et al. Cell. 2017;170:1109-1119.e10.
Acknowledgments The authors thanks the investigators, patients, and study staff who contributed to this trial Medical writing support was provided by Sarah Madsen (Amgen Inc.) The trial is sponsored and funded by Amgen Inc.
No Surgery Due to Disease Progression (Arm 1) or Early Recurrence Post-surgery (Arm 2) Randomization 1:1 n = 150 Arm 1 Arm 2 T-VEC + Surgery n = 76 Surgery Alone n = 74 Surgery During Weeks 1 6 T-VEC + T-VEC + Received No T-VEC or Surgery n = 69/74 (93%) Surgery During Weeks 13 18 n = 57/76 (75%) No Surgery Due to Progressive Disease n = 11/76 (14.5%) 1 local 3 regional 2 local and regional 5 metastatic Early Recurrence (Postsurgery Before Week 14) n = 17/74 (23%) 3 local 1 regional 1 local and regional 12 metastatic n = 3/76 (4%)
Patient Treatment Status Arm 1: T-VEC + Surgery (n = 76) 5.4 (1.2) Arm 2: Surgery Alone (n = 74) N/A Visits where patients received T-VEC doses mean (SD) Patients who received T-VEC n (%) 73 (96.1) N/A Patients who completed T-VEC n (%) 57 (75.0) N/A Patients who never received T-VEC n (%) 3 (3.9) N/A Patients who discontinued T-VEC n (%) Disease progression No injectable lesions Patient request Adverse event Ineligibility determined Requirement for alternative therapy Patients who did not receive protocol-defined surgery n (%) Disease progression Patient request Decision by sponsor Ineligibility determined Requirement for alternative therapy 16 (21.1) 7 (9.2) 4 (5.3) 2 (2.6) 1 (1.3) 1 (1.3) 1 (1.3) 19 (25.0) 11 (14.5) 4 (5.3) 2 (2.6)a 1 (1.3) 1 (1.3) N/A N/A N/A N/A N/A N/A N/A 5 (6.8) - 4 (5.4) - 1 (1.4) - ITT Analysis Set: 150 patients enrolled and randomized aOne was due to new diagnosis of glioblastoma multiforme during study treatment; the second was due to patient unable to be compliant with treatment visits and never received study drug.