2025 Medicare Physician Fee Schedule Proposed Rule with 2.8% Payment Cut
The Medicare Physician Fee Schedule Proposed Rule for 2025 was released on July 10, 2024, with a 2.8% payment cut due to a decrease in the conversion factor. Comments on the proposed rule are due by September 9, 2024, as it must remain budget-neutral from year-to-year as required by current law.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
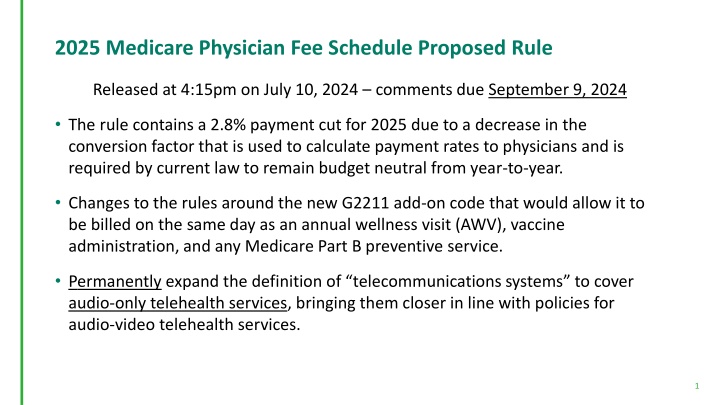
2025 Medicare Physician Fee Schedule Proposed Rule Released at 4:15pm on July 10, 2024 comments due September 9, 2024 The rule contains a 2.8% payment cut for 2025 due to a decrease in the conversion factor that is used to calculate payment rates to physicians and is required by current law to remain budget neutral from year-to-year. Changes to the rules around the new G2211 add-on code that would allow it to be billed on the same day as an annual wellness visit (AWV), vaccine administration, and any Medicare Part B preventive service. Permanently expand the definition of telecommunications systems to cover audio-only telehealth services, bringing them closer in line with policies for audio-video telehealth services. 1
2025 Medicare Physician Fee Schedule Proposed Rule A new enhanced program for Advanced Primary Care Management (APCM) services that could relieve administrative burdens and more appropriately reimburse physicians caring for patients with complex medical and social needs, helping to promote health equity. Surgical Global Codes: a new add-on code, GPOC1, for post-operative care services to more appropriately reflect the time and resources involved in these post-operative visits to compensate the additional resources involved by practitioners who were not involved in furnishing the surgical procedure. 2
2025 Medicare Physician Fee Schedule Proposed Rule RFI about designing a potential ambulatory specialty care model that would leverage the Merit-based Incentive Payment System (MIPS) Value Pathways (MVPs). Proposes new coding and payment for caregiver training for direct care service and supports, including services furnished via telehealth. RFI on the newly implemented Community Health Integration (CHI) services, Principal Illness Navigation (PIN) services, and Social Determinants of Health (SDOH). Establish a new prepaid shared savings option for ACO s with a history of earning shared savings to allow for investments to better serve beneficiaries in underserved communities. 3
2025 Medicare Physician Fee Schedule Proposed Rule New payments to physicians and other health care professionals who are assisting patients at high risk of suicide or overdose, including separate payments for safety planning interventions and post-discharge follow-up contacts. Medicare payment for digital mental health treatment devices used in conjunction with ongoing behavioral health care treatment. Proposes three new HCPCS codes to monitor the usage of these devices. Seeking input on whether coding and payment for Intensive Outpatient Program (IOP) services would be appropriate in additional settings, such as Certified Community Behavioral Health Clinics, as well as seeking comment on facilities that offer crisis stabilization services and non-emergent, urgent care. Expanded coverage of Hepatitis B vaccinations by covering those with unknown or incomplete vaccination histories. 4
Proposed Rule: Advanced Primary Care Management (APCM) For CY 2025 CMS is proposing to establish a set of APCM services described by three new HCPCS G- Codes. Physicians and non-physician practitioners who use an advanced primary care model of care delivery could bill for APCM services for a beneficiary when they intend to be responsible for all primary care and are the continuing focal point for all needed health care services. The Proposed APCM Services Would: Incorporate elements of several existing care management and communication technology-based codes into a bundle Remove some of the more burdensome elements of billing and coding the individual service elements Not be time-based, but rather based on a set of service elements and practice level requriements Be stratified into 3 levels to reflect patient medical complexity and social complexity Billed on a monthly basis 5
Proposed Rule: Advanced Primary Care Management (APCM) Cont... Proposed APCM Service Elements and Practice-level Capabilities Proposed Code Levels Three levels of coding allow for appropriate payment for APCM service provision on a monthly basis Consent Initiating Visit for New Patients 24/7 Access to Care and Care Continuity Level 1 Level 2 Level 3 Comprehensive Care Management Patients with one or fewer chronic conditions Proposed RVU: .17 Patients with 2 or more chronic conditions Proposed RVU: .77 Patients with 2 or more chronic conditions AND AND who are Qualified Medicare Beneficiaries Proposed RVU: 1.67 Patient-Centered Comprehensive Care Plan Management of Care Transitions Practitioner, Home, and Community-based Care Coordination Enhanced Communication Opportunities Patient Population-level Management Performance Measurement *See Table 21 in the Proposed Rule 6
CY 2025 Modifications to the Quality Payment Program The proposed rule for the Quality Payment Program (QPP) for 2025 outlines changes that emphasize alignment and new participation options for clinicians, aiming to enhance healthcare quality for Medicare beneficiaries. MVP Development and Maintenance 6 new MVPs that would be available beginning with the 2025 performance period related to ophthalmology, dermatology, gastroenterology, pulmonology, urology, and surgical care. Limited modifications to the currently finalized MVPs, including the consolidation of 2 neurology-focused MVPs into a single neurological MVP. APP Plus Quality Measure Set An additional quality measure set under the APP which would include the 6 measures currently in the APP quality measure set and incrementally incorporate the remaining 5 Adult Universal Foundation quality measures for a total of 11 measures in the APP Plus quality measure set by the 2028 performance period/2030 payment year. Medicare Shared Savings Program (Shared Savings Program) Accountable Care Organizations (ACOs) would be required to report the APP Plus quality measure set, either as electronic clinical quality measures (eCQMs) or Medicare Clinical Quality Measures for Accountable Care Organizations Participating in the Medicare Shared Savings Program (Medicare CQMs) 7
CY 2025 Modifications to the Quality Payment Program Measure/Activity Inventories and Scoring Methodologies 6 new episode-based cost measures. Revisions to 2 existing episode-based cost measures. Revises cost measure scoring methodology to assess clinician cost of care more appropriately in relation to national averages. Revises methodology for scoring topped out quality measures in specialty sets with limited measures. Remove improvement activity weighting and streamline the reporting requirements for the performance category. Minimum criteria for a qualifying data submission (i.e., eligible for scoring) in the quality, improvement activities, and Promoting Interoperability performance categories. Maintaining Stability Maintain current performance threshold policies, which would leave the performance threshold set at 75 points for the CY 2025 performance period/2027 MIPS payment year. Maintain the 75% data completeness criteria through the 2028 performance period. 8