A Case of High Myopia with Coloboma Post Prophylactic Laser Retinopexy
Patients with coloboma face up to a 40% risk of retinal detachment. Prophylactic laser retinopexy can help prevent this by creating a barrier around the coloboma. Find out more about the case study involving a male patient with high myopia and coloboma.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
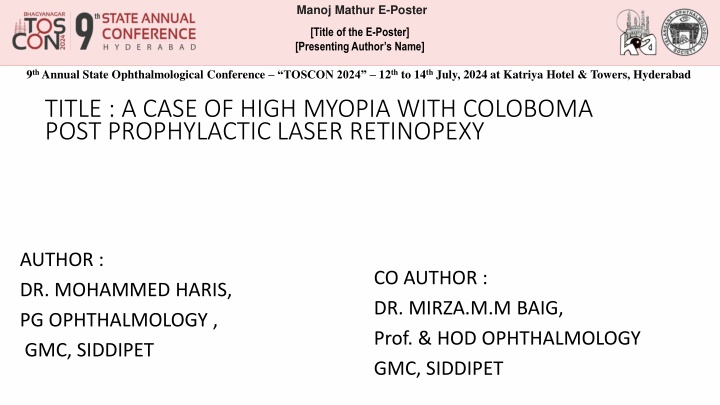
Manoj Mathur E-Poster [Title of the E-Poster] [Presenting Author s Name] 9thAnnual State Ophthalmological Conference TOSCON 2024 12thto 14thJuly, 2024 at Katriya Hotel & Towers, Hyderabad TITLE : A CASE OF HIGH MYOPIA WITH COLOBOMA POST PROPHYLACTIC LASER RETINOPEXY AUTHOR : DR. MOHAMMED HARIS, PG OPHTHALMOLOGY , GMC, SIDDIPET CO AUTHOR : DR. MIRZA.M.M BAIG, Prof. & HOD OPHTHALMOLOGY GMC, SIDDIPET
Introduction A coloboma is defined as a defect in one or more ocular structures due to incomplete closure of embryonic fissure. The embryonic fissure of the developing eye is located inferiorly and slightly nasally and extends from optic nerve to the margin of the pupil. Patients with coloboma carry a risk of up to 40% rhegmatgenous retinal detachment (RRD In most of the cases of RRD in fundus coloboma, the break lies inside the coloboma, or at locus minoris resistentiae and in this presentation we will explore role of prophylactic laser retinopexy in order to prevent retinal detachment. The process is by surrounding the coloboma with contiguous rows of laser spots theoretically preventing spreading of an RRD from the colobomatous to the non-colobomatous region
Materials &Methods We are reporting a case of a male patient, 28 years old presenting with complains of decreased distant vision in both eyes since childhood. On examination he was moderately built and nourished and normal stature. Right Unaided vision CF 1 meter BCVA 6/60 Ocular position Eyelids Normal Conjunctiva Normal Cornea Clear Ant. Chamber WNL , depth PACD = 1CT Iris Normal colour but coloboma + Pupil Oval, reacting to light lens Cataractous involvement of lens ( NS gr II) Left CF 2 meter 6/60 hypertropia Exotropia + hypertropia normal Normal Clear WNL, Depth PACD= 1CT Normal colour but coloboma + Oval, reacting to light Cataratous invovement of lens ( NS gr II) Fundus Hazy media, normal optic disc with CDR 0.2:1, macula: FR+ with coloboma inferior to disc (Ida Mann type 5)and laser burn marks present around coloboma. Hazy media, normal optic disc with CDR 0.2:1, macula: FR+ with coloboma inferior to disc (Ida Mann type 5)and laser burn marks present around coloboma.
Discussion Transition zone between coloboma and normal fundus Histologically, near the coloboma margin, the terminated RPE is adherent to the outer retinal layers. Beyond this point, the retinal layers transition into the non-descript fibrotic tissue called inter-calary membrane (ICM). This zone of adhesion is the point of least resistance termed Locus minoris resistantiae Identification of even a rim of ICM detachment indicates the contribution of coloboma to the causation of RD. In the presence of ICM detachment, OCT can detect dehiscence in zone of least resistance seen as communications between sub-retinal space and sub-ICM space. A OCT demonstrating gradual transition of retina to ICM (arrow). Also notice the detachment of ICM with extension into normal retina beyond coloboma margin and the detached macula located just beyond the coloboma margin. The role of prophylactic laser is to close these communications hence preventing the retinal detachment.
PATHOGENISIS Rudimentary retina (ICM) Myopic fundus resulting in vitreous syneresis Abnormal preretinal tissue causing traction and retinal break results Extremely thin fundus causing atrophic hole to form C) Fluid spreads through ICM break to cause detachment before spreading beyond coloboma to cause RD D)Fluid enters subretinal space both from peripheral retinal break and through break in ICM Prophylactic laser retinopexy : For the treatment to be effective, the entire coloboma margin must be surrounded by at least 2 3 rows of laser burns in an attempt to segregate the coloboma from the rest of the retina and not permit any breaks in the zone of least resistance and ICM to lead to clinical RD.
Conclusion The previous studies concluded that the cases of fundus coloboma, which underwent PLP, maintained visual acuity during follow up which ranged from a minimum of 3 years to a maximum of 17 years (median 5 years). Colobomas are a rare ocular pathology, which may not have overt symptoms early on, but can lead to debilitating defects causing acute vision loss later in life. Early recognition is essential to prevent the development of complications. This presents a challenge as individuals are often asymptomatic and thus may not present for checkups until after the development of acute vision loss due to complications such as retinal detachment. Routine ophthalmology screening can help in identifying potential cases. However, no current screening programs exist for retinal detachment, and thus, it warrants further study for the development of such screening protocols. Prompt management with prophylactic laser retinopexy can reduce the development of complications and improve the quality of life of the patient. References 1. Lingam G, Sen AC, Lingam V, Bhende M, Padhi TR, Xinyi S. Ocular coloboma-a comprehensive review for the clinician. Eye (Lond). 2021 Aug;35(8):2086-2109. doi: 10.1038/s41433-021-01501-5. Epub 2021 Mar 21. PMID: 33746210; PMCID: PMC8302742. 2. Khan TA, Liaqat T, Shahid M, Janjua TA, Rauf A. Isolated Chorioretinal Coloboma: A Case Report. Cureus. 2022 Aug 16;14(8):e28048. doi: 10.7759/cureus.28048. PMID: 36127994; PMCID: PMC9477557. 3. Gopal L, Badrinath SS, Sharma T, Parikh SN, Shanmugam MS, Bhende PS, Agrawal R & Deshpande DA (1998): Surgical management of retinal detachments related to coloboma of the choroid. Ophthalmology 105: 804 809. 4. Mann I (1937): Developmental abnormalities of the eye. London: Cambridge University Press 65 103. 5. Patnaik B & Kalsi R (1981): Retinal detachment with coloboma of the choroid. Indian J Ophthalmol 29: 345 349.