Abnormal Uterine Bleeding: Causes and Evaluation
Abnormal uterine bleeding (AUB) is a common gynecologic complaint that can be caused by various diseases and medications. Clinicians must be familiar with its causes and have an organized approach to evaluation and treatment. The prevalence causes of AUB vary with age, and different age groups have specific causes to consider. Complications of pregnancy should always be excluded, particularly in adolescents. The FIGO classification helps identify structural causes of AUB, such as polyps, adenomyosis, leiomyomas, and malignancy. Treatment options vary depending on the underlying cause, ranging from hysteroscopic surgery for polyps to uterine artery embolization for adenomyosis.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Abnormal uterine bleeding DR. SHAHNAZ AHMADI FELLOWSHIP OF INFERTILITY PROFESSOR OF IUMS
AUB a term which refers to menstrual bleeding of abnormal quantity, duration, and schedule is a common gynecologic complaint, accounting one-third of outpatient visits to gynecologists. AUB can be caused by a wide variety of local and systemic diseases or related to medications. All clinicians must therefore be familiar with its causes and have an organized, logical approach to the evaluation and treatment of the problem
DDX bleeding The prevalence causes of AUB vary with age Pre menarch (foreign bodies, Trauma, and infection) Post menarch ( Anovulatory bleeding, coagulopathies, infections , pregnancy) Reproductive years ( anovulation, hormonal contraception, pregnancy, infections, endocrine disorders, and polyps and myomas) Peri menopausal (anovulation, benign uterine neoplasia, and endometrial hyperplasia) Post menopausal (vaginal/endometrial atrophy and hormone therapy, endometrial cancer) Complications of pregnancy always should be considered and excluded, particularly in adolescents.
DDx AUB The PALM portion of the FIGO classification acronym encompasses structural causes for AUB: Polyps, Adenomyosis Leiomyomas, malignancy hyperplasia
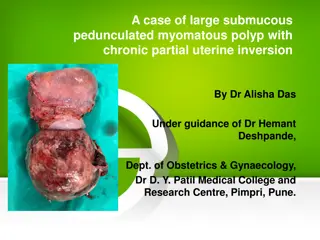
Polyp polyps are identified by TVS or sonohysterography hysteroscopic surgery offers ,a simple and highly effective remedy.
Adenomyosis extension of endometrial glands and stroma into the myometrium. DX: TVS - MRI Treatment: Insertion of a LNG-IUS Uterine Artery Embolization
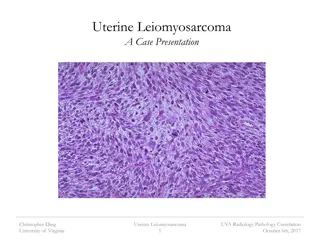
Lyomyoma when they protrude into or displace the uterine cavity. DX: TVS Sono hysterography Treatment: Surgical management after considering the size, number and location of the fibroids Hysterectomy: an option for women with AUB, multiple large fibroids, and no interest in future pregnancy
Malignancy or hyperplasia Endometrial hyperplasia with atypia has significant risk (10-30%) of progression to adenocarcinoma office biopsy reveals endometrial hyperplasia further evaluation is required to exclude atypia or a coexisting cancer that was not represented in tissue specimen and if the subsequent curettage reveals atypical endometrial hyperplasia, there is significant risk of an unrecognized adenocarcinoma.
Treatment Hysterectomy ( in patients with persistent hyperplasia with atypia that is unresponsive to aggressive progestin regimens) Women who respond to medical management should be encouraged to pursue pregnancy at the earliest possible time and must be carefully monitored. Once childbearing is completed, placement of LNG-IUS and periodic TVS and endometrial sampling may be considered. Repeat BX to confirm regression in 3 months following initiation of treatment, without removing the device.
NONSTRUCTURAL causes of AUB are represented in the COIN portion Coagulopathy Ovulatory Dysfunction Endometrial Factors Iatrogenic and Not Yet Classified
Coagulation or bleeding disorder history of pph or excessive bleeding with surgery, dental procedures, or trauma should raise suspicion, but heavy menstrual bleeding since menarche may be the only clue 10-20% of women with unexplained heavy menses. Von Willebrand Disease is the most common inherited bleeding abnormality affecting women. Treatment: Desmopressin, Antifibrinolytic therapy( Tranexamic Acid) Estrogen-Progestin contraceptives or the LNG-IUS
Ovulatory dysfunction Anovulation or Oligo ovulation can result : Thyroid disease Hyperprolactinemia PCOS Hypothalamic Dysfunction from nutritional deficiency, systemic illness or stress.
Endometrial Polyps and the fibroids Chronic Endometritis Acute Endometritis Subclinical Chlamydia trachomatis infections, pelvic tuberculosis, and PID
Iatrogenic Using of various forms of hormonal contraceptives is probably the most common iatrogenic cause of abnormal bleeding in reproductive age women. Abnormal bleeding patterns are commonly reported in association with both copper and levo norgestrel IUD
Not other classified chronic endometritis typically present with AUB, which can vary from intermenstrual spotting and postcoital bleeding to heavy menstrual bleeding. AV Malformations
Diagnostic evaluation of AUB history Onset of Abnormal menses( pre menarchal, sudden, gradual) Duration ( normal or prolonged, consistent or variable) Intermenstrual Interval ( number of days, regularity) Volume ( heavy, light, or variable) Temporal Associations ( post coital, postpartum, post pill, weight gain or loss) Associated symptoms ( premenstrual molimina, dysmenorrhea, dyspareunia, galactorhea, hirsutism) Underlying systemic illness ( renal , hepatic, hematopoietic, thyroid) Medications ( hormones, anticoagulants, antipsychotics, antidepressants, anti seizure)
In the majority of women with true anovulatory bleeding, the menstrual history alone can establish the diagnosis with sufficient confidence that treatment can begin without extensive laboratory evaluation or expensive imaging. regular monthly periods that are heavy or prolonged are more likely related to an anatomical lesion or a bleeding disorder than to anovulation.
History of changing pads or tampons more often than every 3 hours, use of more than 20 over single menses, the need to change protection during the night, frequent episodes of accidental soiling of clothing and bedsheets, the passage of clots larger than an inch, menses lasting longer than 7 days, and diagnosis of anemia should all raise concerns about abnormally heavy menstrual bleeding
Extrauterine sources of abnormal bleeding include the urethra (urethritis or caruncle) Bladder ( UTI and cancers) Vagina ( vaginitis, trauma, and ulcerative lesions) Vulva ( Trauma , skin lesions) Anorectal lesion ( anal fissures, hemorrhoid, IBD, cancers) During pelvic examination, attention should be paid to uterine size, contour (smooth and symmetrical or irregular), consistency ( firm or soft), mobility and tenderness, and presence of adnexal masses.
Physical exam Vital signs and complete pelvic examination with a particular focus on: Potential sites of bleeding from the vulva, vagina, cervix, urethra, anus, or perineum Any abnormal findings tract (mass, laceration, ulceration, vaginal or cervical discharge, foreign body. Size and counter of the uterus, an enlarged uterus may be due to pregnancy, uterine leiomyomas, adenomyosis,or uterine malignancy. Limited uterine mobility can be caused by pelvic adhesions, or a pelvic mass, endometriosis. A boggy, globular, tender uterus : Adenomyosis Uterus tenderness: PID Presence of an adnexal mass or tenderness
A general examination should be performed to look for signs of systemic illness, such as fever, ecchymosis, an enlarged thyroid gland, or evidence of hyper androgenism. Acanthosis nigricans may be seen in patients with PCOS. Galactorrhea : Hyperprolactinemia
Laboratory Pregnancy test CBC Serum Progestron between cycle day 22 and 24 in a 28-day cycle. In sexually active women, a nucleic acid-based test for chlamydia and gonorrhea and a wet prep to exclude trichomonas infection, particularly in those with evidence of vaginitis or cervicitis. Liver or Renal function test PT, PTT, Von Willebrand factor, factor VIII level, and blood typing.
TFT : If ovulatory dysfunction, and also HMB. Prolactin: anovulatory bleeding, amenorrhea, or galactorrhea, or are taking medications that cause hyperprolactinemia. Androgen Levels: AUB and signs of androgen excess. FSH: if POF is suspected FSH, LH, Estradiol: suspected hypothalamic dysfunction Estradiol Levels: if POF is suspected or an adnexal mass is present( due to an estrogen-secreting ovarian tumor)
Assessment of ovulatory function: TSH , Prolactin Coagulation Tests: HMB, Bleeding diathesis (VWF, Immune Thrombocytopenia, or Platelete function defect, patients who take warfarin
Endometrial sampling Endometrial hyperplasia and cancer are more commonly detected in older then in younger women, but the duration of exposure to unopposed estrogen stimulation is the more critical risk factor. Pipelle suction curette Current indications for D&C include: A nondiagnostic office Or Cervical Stenosis Or patient discomfort
Cont. Age 45 years to menopause: In patients who are ovulatory, any AUB, including IMB. In any patient, bleeding that is frequent intervals, heavy, or prolonged > 8d. Younger than 45 years: History of unopposed estrogen exposure( obesity, chronic ovulatory dysfunction) Failed medical management of the bleeding High risk patients for endometrial cancer (eg, Tamoxifen therapy, LYNCH)
Imaging TVS : The 1st line MRI: Only as a follow-up imaging test and only when it will provide information that is not available on ultrasound CT: To evaluate pelvis for metastatic disease in some malignancies. SIS: If intra cavitary pathology is suspected, and also useful in evaluating AUB associated with caesarean scar defects. Hysteroscopy; direct visualization of the endometrial cavity, and allows targeted Bx or excision of lesions identified during the procedure
Compared with hysteroscopy, the major advantage of SIS is that can assess the depth of extension of leiomyomas into the myometrium or subserosal surface. SIS also is able to identify asymmetric or focal endometrial thickening , a potentially important marker of endometrial neoplasi
Case Study 1 a 24-year-old married female, calls the clinic with a complaint of heavy vaginal bleeding. I bled through my tampon and pad again, and my nightgown and bedding are soiled. I m sick of this - I just want it to stop! Her call is sent to the triage nurse.2
Q1: What is the most important information for your triage to obtain at this point? Acute vs. Chronic Has this happened before? Stable vs. UnstableIs she lightheaded? Short of breath? pregnancy Status LMP Contraception? Systemic Symptom sAbdominal pain? Pelvic pain? Urinary symptoms?
answer : her periods have gradually gotten worse. They are now lasting 6-7 days instead of 3- 4, and come every 30 days instead of every 26. The flow on her first few days has also gotten much heavier. She currently has no pain, cramping, vaginal discharge, or urinary symptoms. She has never missed a menstrual cycle. Her LMP was about a month ago , she and her husband use condoms, and she has not been sexually active for a month.
Vital signs: T 37, HR 80, RR 16, BP 130/86;, ,BMI 37.2, pain 0/ her medical history is remarkable only for severe reflux disease for which she takes daily Panthoperazol . She smokes occasionally urine HCG :The test is negative.
Other Lab Tests to Consider Hb/ HCT for anemia and ferritin for iron deficiency Hypothyroidism presents with heavy menses and should always be ruled out Von Willebrand disease is the most common coagulation disorder causing menorrhagia, but it is not usually checked unless there are other signs of bleeding or the patient is an adolescent laboratory test results are normal. She reports missing 1-2 days of work per month and she is avoiding social activities during the first three days of her period. She adamantly declines to consider combination hormonal contraception.
The best alternative strategy for managing her cycles includes which of these? Reassurance Iron supplementation ibuprofen from the beginning of her menstrual cycle through the end of her menses Contraception containing progesterone only
appropriate management depends on the patients medical history, risks, and personal choice contraception is desired, either combination contraception or Mirena IUD/IUS would be indicated she is unable to take estrogen (i.e., clotting risk), a progesterone-only contraception is appropriate she does not desire contraception, or doesn t want to take any hormones, NSAIDs alone may be enough
What if pregnancy test had been positive? How would that change your management? bleeding in early pregnancy warrants emergency evaluation to rule out: Ectopic pregnancy Spontaneous, threatening, or impending abortion
Case Study 2 a 51-year-old female, complains of heavy menstrual bleeding. She reports 6 weeks of bleeding all the time . She cannot be more specific about her bleeding pattern. She is fatigued. On further questioning, she endorses increased sweating, palpitations, and insomnia.
What additional information would you want Does she need a pregnancy test? Pregnancy status Any woman with a history of abnormal menses should have a urine pregnancy test! Hypotension, tachycardia, orthostasis Fever,ill appearance, Abdominal /pelvic pain , Menstruation pattern , Estimated blood loss Note FSH/estradiol levels not useful in perimenopause
pregnancy test is negative. history suggests that she is peri menopausal. Her blood work shows a normal TSH and a low ferritin level. She has a history of fibroids, polycystic ovarian syndrome with anovulatory cycles, and long-term oral contraceptive use however she stopped taking her OCPs about 6 months ago. She reports that she has sometimes gone months without a period over the past 2 years. Vital signs: T 37, HR 80, RR 15, BP 130/85; BMI 36.3; pain 1/1018
Because she has a history of PCOS and anovulatory cycles, the provider decides to order a pelvic (transvaginal) ultrasound, and to refer to gynecology for an endometrial biopsy.
transvaginal ultrasound and endometrial biopsy test results are normal. Appropriate management for abnormal bleeding in the peri menopausal time period include All : EXCEPT OCP postmenopausal hormone therapy with E + MP Mirena IUD/IUS , Intermittent medroxyprogesterone acetate