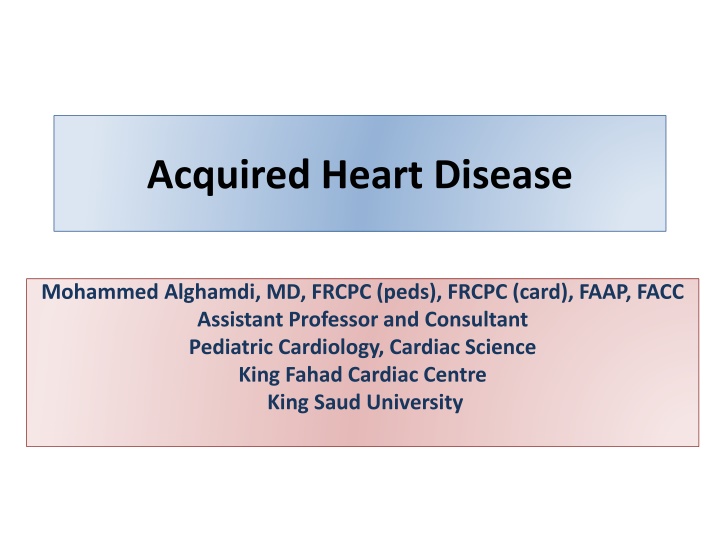
Acquired Heart Disease
Acquired heart disease in children, including rheumatic fever and Kawasaki disease, is crucial for pediatric cardiologists to diagnose and treat effectively. Rheumatic fever, often precipitated by Group A Streptococcal pharyngitis, can lead to rheumatic heart disease if not recognized promptly. Recognizing the Jones criteria for diagnosing rheumatic fever is essential in identifying children at risk. Genetic, environmental, socioeconomic, and immunological factors play roles in the susceptibility to these heart conditions. Early detection and management are key in preventing severe complications in pediatric patients with acquired heart disease.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Acquired Heart Disease Mohammed Alghamdi, MD, FRCPC (peds), FRCPC (card), FAAP, FACC Assistant Professor and Consultant Pediatric Cardiology, Cardiac Science King Fahad Cardiac Centre King Saud University
Acquired Heart Disease Rheumatic Fever Most common Kawasaki Disease Infective Endocarditis Pericarditis Myocarditis Cardiomyopathy Cardiac Arrhythmias: Any case scenario of heart failure and a heart rate more than 200 is arrhythmia until proven other wise. The commonest arrhythmia in children is SVT.
Rheumatic Fever RF: most common cause of acquired heart disease in developing countries. 150 in 100,000 in developing countries (more common in developing) 1 in 100,000 in developed countries. It called : Rheumatic heart disease (RHD) if the inflammatory changes involve the cardiac valves and myocardium. RF is the commonest acquired heart disease in developing countries while Kawasaki is the commonest in developed countries.
Rheumatic Fever Precipitated by Group A Streptococcal (GAS) pharyngitis (not other types of GAS infections) Acquiring the disease depends on the host susceptibility which depends on genetic, environmental, socioeconomic and immunological status. 2-4 weeks after untreated GAS Pharyngitis T-cell and B-cell lymphocytes produce antibodies against some Streptococcal antigens that cross-react with antigens on myocytes or cardiac valve tissue. RF no heart sequale unlike RHD. RHD will lead to rheumatic fever which will lead to well established disease.
It is not due to the infection itself rather due to cross-reactivity between myocytes and bacterial antigens. Not from one infection but clinical + sub- clinical infection leading to acute rheumatic fever, and if it is not recognized rheumatic heart disease.
Rheumatic Fever Jones criteria (1992) Major Manifestations Carditis Polyarthritis Chorea Erythema marginatum Subcutaneous nodules Minor Manifestations Arthralgia Fever Raised ERS or CRP Prolonged PR interval on ECG Evidence of antecedent GAS infection 1. Positive throat culture or rapid antigen test for GAS 2. Raised or rising streptococcal antibody titre
Rheumatic Fever Jones criteria (1992) Two majors or one major and two minors plus evidence of antecedent GAS infection . ASO titer may be ve; repeat in 2-4 weeks if there is a high index of suspicion. Exceptions: Chorea & indolent carditis do NOT require evidence of antecedent GAS infection Recurrent episode requires : Only one major OR Several minor manifestations Plus evidence GAS infection
Rheumatic Fever Arthritis: Most common ARF presentation (75% of first attacks) Migratory, Asymmetrical, Polyarthritis, of large joints Typically: extremely painful Highly responsive to salicylate and NSAID therapy Within 3 days Monoarthritis if history of early use of NSAID Premature abortion the polyarthritis manifestation. You can t give aspirin if patient has already started on NSAID
Rheumatic Fever Cardiatis: Valvulitis: Isolated MV is the commonest followed by MV plus AV then AV, and rarely affects the right side. Early disease leads to valvular regurgitation, Prolonged or recurrent attacks lead stenosis Pericarditis and myocarditis may occur RHD is less rare in children less than 5 ears because it requires recurrent infection.
Rheumatic Fever Sydenham s chorea Jerky, uncoordinated movements esp. of hands, feet, tongue and face. Disappear during sleep More common in adolescence female Occur after a prolonged latent period following GAS 6 wks - 3 yrs following GAS infection Strong association with carditis In sydenham chorea, it s RHD until proven otherwise. Because it can happen 3 years post-GAS where it s hard to find any evidence of strep infection. Therefore, anyone with chorea should do echo. Usually seen in people who have beautiful handwriting and suddenly drops.
Rheumatic Fever Erythema marginatum Rare & difficult to detect esp. in dark-skinned patients Circular patterns of bright pink macules or papules that blanch under pressure Trunk and proximal extremities Almost never on face Not itchy or painful vs eczema
Rheumatic Fever Subcutaneous nodules Rare < 2% of cases, Highly specific manifestation of ARF but it is not sensitive. Round, firm, mobile and painless nodules mostly affect the elbow Appear 1-2 weeks after onset of other symptoms last 1-2 weeks (rarely > 1 month) Strongly associated with carditis It is specific to RF but not sensitive
Rheumatic Fever Treatment: Antibiotics to eradicate of residual GAS bacteria Anti-inflammatory agents High dose aspirin or NSAIDs. Steroids for severe carditis CHF therapy as indicated Primary prevention by preventing the infection from happening, secondary prevention to prevent repeated infection (because RHD does it occur from the first attack it needs several episodes to occur. Sydenham Chorea: Haloperidol
Rheumatic Fever Secondary prophylaxis Secondary Prophylaxis ANTIBIOTIC DOSE First line ROUTE FREQUENCY Benzathine penicillin G (BPG) 1,200,000 U 20kg 600,000 U < 20kg IM Best route Q4 wks OR Q3 wks if confirmed recurrent ARF despite adherence to 4 wks injection Second line Penicillin V 250mg Oral BID Penicillin allergy 0.2% only stop penicillin if patient has anaphylactic shock Erythromycin 40mg/kg/day (children) Oral BID QID 400mg (adults) Oral BID
Rheumatic Fever Duration of Secondary Prophylaxis CATEGORY DURATION OF PROPHYLAXIS ARF with no or mild carditis Min of 10 years after most recent episode ARF OR until age 21 years (whichever is longer) ARF with moderate carditis Min of 10 years after most recent episode ARF OR until age 30 years (whichever is longer) with ARF with severe carditis Min of 10 years after most recent episode ARF OR until age 30 years (whichever is longer) May need life long prophylaxis
Damage to the heart is permanent whereas the arthritis.
Kawasaki Disease KD: inflammatory disease of unknown etiology causing acute, diffuse vasculitis of medium size blood vessels (mainly coronary arteries). Most common cause of acquired heart diseases in developed countries. More common in Japanese population Higher in males than females Typical age: 6 months - 5 years Nb : this Dz followed mainly by cardiologist with association of rumatologist
Kawasaki Disease Cardiac Involvement: Coronary arteries( late): if left untreated the risk of CAD is 25%, this is reduced to 2% with treatment. Dilation and aneurysm formation Thrombus formation Fibrosis and stenosis Myocardial infarction. May cause myocarditis and endocarditis Other medium size arteries Axiliary, femoral, iliac, and renal arteries.
Kawasaki Disease Fever: at least 5 days duration At least 4 of the following (to call it complete typical KD). 1 Conjunctivitis: bilateral, non-purulent 2 Skin Rash: polymorphous skin rash 3 Mucous membrane changes: red, dry, and cracked lips, strawberry tongue 4 Extremities changes: palms/soles erythema, hands/ feet edema, Skin peeling 5 Cervical lymphadenopathy: unilateral and >1.5 cm in diameter
Kawasaki Disease DDX of KD: Scarlet fever EBV infection Adenovirus infection Staphylococcal scalded skin syndrome Drug reactions Stevens Johnson syndrome.
Kawasaki Disease Atypical (incomplete) KD: Cases of KD that do not fulfill diagnostic criteria. More common in infants Children with Fever greater than 5 days Two or three classic symptoms Supporting laboratory abnormalities or echo evidence of coronary involvements Should be treated as KD Nb : better treat As complete to avoid complications (( coronary arteries complications ))
Kawasaki Disease Labs abnormalities in KD: Elevated ESR > 50 (70%) Elevated C-reactive protein (50%) CBC: Neutropenia , leukocytosis (50%) Nonspecific anemia Thrombocytosis more than 500,000 is very pathagnomonic. Marker of KD Not seen until 2nd week of the disease Elevated liver transaminases (40%) Low serum albumin level Sterile pyuria (33%) Aseptic meningitis (up to 50%).
Kawasaki Disease Treatments: IVIG 2 g/kg 2nd dose if persistent fever within 48 h of the initial dose High dose of aspirin of 30 100 mg/kg/day. Once afebrile: aspirin is decreased to 3 5 mg/kg/day Aspirin acts as an anti-inflammatory agent if give in high doses for long time, analgesic if given in medium doses when needed and antiplatelet if given in small doses for long time. Echo at base line Repeat echocardiogram and inflammatory markers at 6 8 weeks If normal coronary arteries and inflammatory markers : aspirin can be stopped If coronary artery abnormalities: long-term Rx with aspirin Other anticoagulants warfrin if giant aneurysm of coronary arteries
Infective Endocarditis infection of the endocardial lining of the heart or cardiac vessels Rare but with high mortality Usually affect abnormal cardiac structure Valvular disease Septal defects Presence of foreign material such as mechanical valves and patch material after surgical repair.
Infective Endocarditis Etiology: Gram- positive bacteria: > 90 % 0f bacterial case Streptococci Viridans : most common infectious agent Staphylococcal species especially prosthetic valves. Enterococci : less common pediatric age group. Gram-negative bacteria: < 10% of bacterial cases Example: HACEK group Haemophilus, Actinobacillus, Cardiobacterium, Eikenella and Kingella Fungal uncommon Neonate, immunocompromised patients, prolonged antibiotic 10% IE case: organisms cannot be identified.
Infective Endocarditis Clinical Features: General: Fever Nonspecific manifestations myalgias, arthralgias, headache, and general malaise Cardiac: New onset or worsening valvular regurgitation Congestive heart failure Heart block
Infective Endocarditis Clinical Features: Extracardiac - septic embloism: ischemic changes can occur anywhere even in the brain causing stroke. CNS: infraction, brain abscess Renal: proteinuria, hematuria, pyuria PHx - Stigmata of SBE: Janeway lesions:Non-tender, flat lesions on palms and soles. Osler s nodes: Tender, raised nodules on fingers and toes. Roth s spots: Exudative lesions of the retina. Splinter hemorrhages: Non-blanching, linear, under nails. Splenomegaly
Infective Endocarditis Labs: Blood cultures are the most important lab test Three blood cultures collected over a 24-h period from different sites at different times. Because if only one of the cultures is positive it could be contamination. CBC: Anemia Elevated ESR/CRP Positive rheumatoid factor
Infective Endocarditis Treatment: Supportive medical therapy Prolonged antibiotic therapy Initially empiric broad spectrum Abx which then adjusted according to organism sensitivity. Admit for I.V Abx with a combination of two or three drugs. 4-8 weeks course depending on the type of organism and resistance. Removal of infected line Surgical intervention: may be required
Infective Endocarditis SBE prophylaxis: Only indicated at dental procedures or respiratory procedure (not for gynecological procedures anymore) for high risk patients No longer recommended for GI or GU procedures Prophylaxis regimens: Oral amoxicillin 50 mg/kg (up to 2 g) OR IV/IM ampicillin 50 mg/kg Patients allergic to penicillin Cephalexin 50 mg/kg PO (up to 2 g) OR Clindamycin 20 mg/kg (up to 600 mg) OR Azithromycin (or clarithromycin) 15 mg/kg (up to 500 mg)
Infective Endocarditis SBE prophylaxis Prosthetic cardiac valve Previous IE Congenital heart disease Unrepaired cyanotic CHD, including those with palliative shunts and conduits Repaired CHD with prosthetic material or device (surgery or cath), during the first 6 months after the procedure Repaired CHD with residual defects at the site or adjacent to the site of a prosthetic patch or prosthetic device Cardiac transplantation recipients with cardiac valvulopathy
Myocarditis Inflammatory infiltrate of the myocardium with necrosis/degeneration of the myocytes Viral infections: most common causes in order: Coxsackievirus type B Adenovirus Parvovirus B19 Others: CMV, EBV, HIV, Hep C Other infectious causes: bacteria, rickettsiae, protozoa. Non-infectious causes: Rheumatologic disease: SLE, rheumatoid arthritis Drugs and Toxins: chemotherapy
Myocarditis Variable initial presentation Viral prodrome: fever, URTI or GI symptoms precede the S/S of HF by 3 weeks. Hx: lethargy, poor feeding, irritability, respiratory distress, exercise intolerance PHx: Signs of CHF Tachycardia Tachypnia (increase work of breathing) Gallop rhythm and murmur of mitral regurgitation Hepatomegaly
Myocarditis Investigation: CXR: Cardiomegaly Pulmonary congestion ECG: Sinus tachycardia Low voltage QRS Non-specific T wave changes Echo: Dilated LV with reduced systolic function MR Pericardial effusion
Myocarditis Investigation: Myocardial biopsy: Historically used to be the gold standard test Currently not routinely performed Invasive low sensitivity of the procedure (3 63%) patchy involvement of the myocardium Treatment: Cardio-respiratory Support: Inotropes, Ventilation, ECMO Anti-CHF therapy IVIG and Steroid not supporting evidence for their benefit Antiviral agents and interferon need further studies.
Cardiomyopathy Cardiomyopathy: myocardial disease resulting in thickening of myocardial fibers or fibrosis. Pediatric cardiomyopathy: almost exclusively non- ischemic Types: Dilated cardiomyopathy (58%) the commonest, must rule out arrhythmia. Hypertrophic cardiomyopathy (30%) syncope while exercising might lead to sudden cardiac death in athletics because of ventricular tachycardia progressing to ventricular fibrillation. Restrictive cardiomyopathy (5%) Arrhythmogenic Right Ventricular Cardiomyopathy ARVC (5%)