Acute Coronary Syndrome: Symptoms, Diagnosis, and Treatment
Learn about Acute Coronary Syndrome (ACS), a spectrum of cardiac conditions ranging from ST-segment elevation myocardial infarction (STEMI) to unstable angina. Discover the symptoms, physical exam findings, and treatment options associated with ACS.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
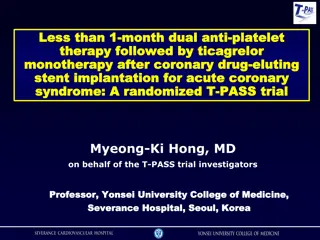
ACS Zohair Al Aseri 2019
Acute Coronary Syndrome Introduction Chest Pain history Physical Exam Cardiac risk factors Cardiac biomarkers ECG in ACS New imaging modality Treatments Summary 2
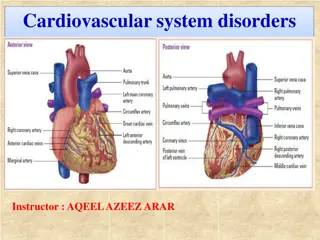
Acute coronary syndrome (ACS) Is a spectrum of clinical presentations: Ranging from: ST-segment elevation myocardial infarction (STEMI) Non ST-segment elevation myocardial infarction (NSTEMI) Unstable angina
Acute coronary syndrome (ACS) It is almost always associated with rupture of an atherosclerotic plaque and partial or complete thrombosis of the infarct-related artery.
Acute coronary syndrome (ACS) Symptoms Palpitations Pain: Usually pressure, squeezing, or a burning sensation across the precordium May radiate to the neck, shoulder, jaw, back, upper abdomen, or either arm
Acute coronary syndrome (ACS) Symptoms Exertional dyspnea that resolves with pain or rest Diaphoresis from sympathetic discharge Nausea from vagal stimulation Decreased exercise tolerance Abdominal Pain for inferior MI
Acute coronary syndrome (ACS) Angina Equivalents Shortness of breath Severe weakness, Light-headedness Diaphoresis, nausea and vomiting.
Acute coronary syndrome (ACS) Physical Examination Hypotension - Indicates ventricular dysfunction due to myocardial ischemia, infarction, or acute valvular dysfunction Hypertension - May precipitate angina or reflect elevated catecholamine levels due to anxiety or to exogenous sympathomimetic stimulation Diaphoresis
Acute coronary syndrome (ACS) Physical Examination Pulmonary edema and other signs of left heart failure Extracardiac vascular disease Jugular venous distention Cool, clammy skin and diaphoresis in patients with cardiogenic shock
Acute coronary syndrome (ACS) Physical Examination Third heart sound (S3) may be present, Fourth heart sound (S4) prevalent in patients with inferior-wall ischemia and may be heard in patients with ischemia or systolic murmur secondary to mitral regurgitation A systolic murmur related to dynamic obstruction of the left ventricular (LV) outflow tract may also occur. A new murmur may reflect papillary muscle dysfunction
Acute coronary syndrome (ACS) Differential Diagnoses Acute Pericarditis Anxiety Disorders Aortic Stenosis Asthma Dilated Cardiomyopathy Emergent Treatment of Gastroenteritis Esophagitis Hypertensive Emergencies in Emergency Medicine Myocardial Infarction Myocarditis
Acute coronary syndrome (ACS) Complications pulmonary edema rupture of the papillary muscle left ventricular free wall, and ventricular septum.
Peak A is the early release of myoglobin or creatine kinase isoenzyme MB (CK-MB) after acute MI. Peak B is the cardiac troponin level after infarction. Peak C is the CK-MB level after infarction. Peak D is the cardiac troponin level after unstable angina. Acute coronary syndrome (ACS)
Acute coronary syndrome (ACS) Troponin Troponin levels increase about 6 h after the onset of infarction They remain elevated for as long as 2 weeks. As a result, troponin values cannot be used to diagnose reinfarction.
Acute coronary syndrome (ACS) Highly sensitive Troponin Highly sensitive troponin I assay (hsTnI) or contemporary troponin I assay (cTnI) determination 3 hours after admission for chest pain may facilitate early rule-out of acute myocardial infarction.
Acute coronary syndrome (ACS) Myoglobin Not cardiac specific May be detected as early as 2 hours Results should be supplemented with other, more specific cardiac biomarkers, such as CK-MB or troponin.
Acute coronary syndrome (ACS) CBC Electrolytes, especially K Blood glucose level Renal profile.
Acute coronary syndrome (ACS) Electrocardiography Should be reviewed promptly. KPI Door to ECG is 10 minute Recording an ECG during an episode of the presenting symptoms is valuable. Transient ST-segment changes (>0.05 mV) that develop during a symptomatic period and that resolve when the symptoms do are strongly predictive of underlying CAD and have prognostic value. Comparison with previous ECGs is often helpful.
Acute coronary syndrome (ACS) Electrocardiography A normal ECG or one that remains unchanged from the baseline does not exclude the possibility that chest pain is ischemic in origin
Acute coronary syndrome (ACS) Electrocardiography Differential of transient ST-segment elevations: LV aneurysm pericarditis, Prinzmetal angina early repolarization Wolff-Parkinson-White syndrome. Fixed ECG changes suggest acute myocardial infarction.
Acute coronary syndrome (ACS) Electrocardiography Difficult cases where there is ST elevation Bundle-branch block LV aneurysm Ventricular hypertrophy Paced Rhythm
Acute coronary syndrome (ACS) Computed Tomography Coronary Angiography and CT Coronary Artery Calcium Scoring The triple rule out protocol might be helpful in the evaluation of select patients, but these findings suggest that it should not be routinely used with the expectation that it will improve efficiency or reduce resource use.
Acute coronary syndrome (ACS) Chest X Ray Cardiomegaly and pulmonary edema Complications of ischemia, such as pulmonary edema. Provide clues to alternative causes of symptoms, such as thoracic aneurysm or pneumonia
Acute coronary syndrome (ACS) Echo: Echocardiogram help in Defining the extent of an infarction Assessing overall function of the left and right ventricles. Identify complications, such as acute mitral regurgitation, LV rupture, and pericardial effusion
Acute coronary syndrome (ACS) Cardiac Angiography Diagnostic and therapeutic The earlier that coronary angiography is performed, the lower the risk of recurrent ischaemia
Acute coronary syndrome (ACS) Stress cardiac magnetic resonance imaging (MRI) in an observation unit setting reduce the medical costs, compared with inpatient care, for patients who present with emergent, non-low-risk chest pain, without missing acute coronary syndrome.
Acute coronary syndrome (ACS) Treatment for NSTEMI Aspirin Clopidogrel Unfractionated heparin or (LMWH) IV platelet glycoprotein IIb/IIIa complex blockers (eg, tirofiban, eptifibatide) beta blocker ACEI Statin. Pain management nitro The goal is early revascularization.
Acute coronary syndrome (ACS) Treatment for STEMI Aspirin Clopidogrel Unfractionated heparin or (LMWH) IV platelet glycoprotein IIb/IIIa complex blockers (eg, tirofiban, eptifibatide) PCI if not available fibrinolysis beta blocker ACEI Statin. Pain management nitro The goal is early revascularization.
Acute coronary syndrome (ACS) Nitrates Do not improve mortality Provide symptomatic relief by means of several mechanisms, including coronary vasodilation, improved collateral blood flow, decrease in preload (venodilation and reduced venous return), and decrease in afterload (arterial vasodilation). Don t give in Hypotension Right, posterior or inferior MI Sever brady or tachycardia Or with physphodistrase inhibitors
Acute coronary syndrome (ACS) Beta-blockers Beta-blockers are indicated in all patients. Contraindications: Systolic blood pressure less than 90 mm Hg Cardiogenic shock Severe bradycardia Right, posterior or inferior MI Second- or third-degree heart block Asthma or emphysema that is sensitive to beta agonists Peripheral vascular disease Uncompensated CHF
Acute coronary syndrome (ACS) Aspirin 162 mg to 350 mg oral immediately if no contraindicationes Aspirin permanently impairs the cyclooxygenase pathway of thromboxane A2 production in platelets, in this way inhibiting platelet function. Aspirin reduces morbidity and mortality and is continued indefinitely
Acute coronary syndrome (ACS) Clopidogrel Clopidogrel (thienopyridine) inhibits adenosine 5'-diphosphate (ADP) dependent activation of the glycoprotein IIb/IIIa complex, a necessary step for platelet aggregation. Optimal loading dose still being evaluated. 600 mg vs 300 mg. Then 75 mg daily Withhold clopidogrel for at least 5 days before elective coronary artery bypass grafting (CABG).
Acute coronary syndrome (ACS) Dual antiplatelet therapy with clopidogrel and aspirin compared with aspirin alone: Reduces major CV events in patients with established ischemic heart disease Reduces coronary stent thrombosis. Not routinely recommended for patients with prior ischemic stroke because of the risk of bleeding Need PPI to prevent GI bleeding???
Acute coronary syndrome (ACS) Prasugrel Like clopidogrel, prasugrel is a thienopyridine ADP receptor inhibitor that inhibits platelet aggregation. Reduce new and recurrent myocardial infarctions. Loading dose is 60 mg PO once and maintenance is 10 mg PO qd (given with aspirin 75-325 mg/d). Indicated for the reduction of thrombotic cardiovascular events (including stent thrombosis) with ACS that is managed with PCI.
Acute coronary syndrome (ACS) Heparine Unfractionated or LMWH Was associated with a 33% reduction in the risk of myocardial infarction or death in patients with unstable angina who were treated with aspirin plus heparin, compared with patients who were treated with aspirin alone May be LMWH is better thn Unfractinted heparine
Acute coronary syndrome (ACS) Abciximab, eptifibatide, and tirofiban Glycoprotein IIb/IIIa receptor antagonists Inhibit the glycoprotein IIb/IIIa receptor, which is involved in the final common pathway for platelet adhesion and aggregation. IIb/IIIb antagonists in combination with aspirin are considered standard antiplatelet therapy for patients at high risk for unstable angina. Eptifibatide or tirofiban in patients with high-risk features in whom invasive treatment is not planned
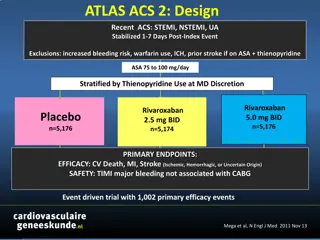
Acute coronary syndrome (ACS) Factor Xa inhibitors (need further studies) Oral Xa inhibitor rivaroxaban Xda inhibitor, fondaparinux (Arixtra)
Acute coronary syndrome (ACS) Fibrinolysis TNK TPA Sterptokinase Urokinase Should be given immediately to STEMI patient if no contraindications and if PCI is not available KPI: 60 minutes (door to needle time) in emergency department
Fibrinolytics In the ED fibrinolytics should be given to patients with symptoms of ACS and ECG evidence of on of the following: STEMI New LBBB True posterior infarction
Fibrinolytics The AHA recommends Fibrinolytics within 30 to 60 minutes of arrival in the emergency department. It is encouraged that AMI patients who undergo primary PTCA have therapy initiated no later than 90 minutes after arrival.
The four Ds of emergency department (ED)based diagnosis and management of the patient with acute myocardial infarction (AMI).
Fibrinolytics TNK TNK has several interesting characteristics and associated potential benefits: (1) its longer half-life allows it to be administered as a single bolus (2) 14 times more fibrin specific than t-PA and even more so than r- PA (3) 80 times more resistant to plasminogen activator inhibitor type 1 than t-PA. TNK was equally or minimally more effective, particularly in late presenters.
Chest Pain Evaluation Summary Chest Pain Inclusion Exclusion Life Threatening Conditions Prognostic Complication Esophageal perforation Pneumothorax Anti ischemic contraindications A Dissection CXR, Bil BP PE 48
Chest Pain Evaluation Summary In Triage Chest pain or angina equivalent Entry Working diagnosis ACS In Monitored bed ECG ST Elevation No ST elevation Troponin positive Troponin negative Biomarkers CKMB Final Diagnosis Acute MI Unstable angina 49
ED ACS Management and Algorithms Comprehensive management plan can be assembled through ABCDE Approach A Antiplatlet, anticoagulant, ACEI & ARB B B. blocker and blood pressure control C Cholesterol and cigarette control and cessation D Diet and Dm control E Exercise