Allograft Transplantation and Immune Rejection Mechanisms
Allograft transplantation involves the transfer of organs between individuals of the same species, leading to potential rejection reactions mediated by immune responses against MHC molecules. This process involves direct and indirect pathways of host T cells recognizing allograft HLA, leading to hyperacute, acute, and chronic rejection scenarios. Additionally, hematopoietic stem cell transplantation serves as a therapy for hematopoietic malignancies, aplastic anemia, and certain inherited disorders, with sources including bone marrow and umbilical cord blood.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Allografts transplantation of organs from one individual to another of the same species. Rejection is a complex phenomenon involving both cell- and antibody-mediated reactions that destroy the graft. Immune Recognition of Allografts Rejection of allografts is a response mainly to MHC molecules. Immune Recognition of Allografts
Host T cells recognize allograft HLA by two pathwaysdirect and indirect: Direct from the donor; the most important cells in this process are donor dendritic cells. Host CD8 T cells recognize donor class I HLA molecules and mature into CTL; host CD4 T cells recognize donor class II HLA molecules; they proliferate and differentiate to form TH1 (and possibly TH17) effector cell populations. Direct pathway: pathway: Host T cells recognize donor HLA on APC derived Indirect and presentation on host APC (analogous to any other exogenous processed antigen). The principal response is therefore a DTH mediated by CD4 T lymphocytes. Indirect pathway: pathway: Host T cells recognize donor HLA after processing
Hyperacute Occurs when the recipient has been previously sensitized to graft antigens (e.g., by blood transfusion or pregnancy). Mediated by preformed antibodied Occur immediately after transplantation (minutes to days) Acute Rejection Typically occurs within days or months of transplantation or after cessation of immunosuppressive therapy. Both cellular and humoral mechanisms can contribute. Gradual onset of oliguria and azotemia. Treated with increase immunosuppressive dose Chronic rejection occurs over months to years gradual onset of oliguria, hypertension and azotemia Micro: arteries show dense obliterative intimal fibrosis, causing allograft ischemia. Poor response to treatment Hyperacute Rejection Rejection Acute Rejection Chronic rejection
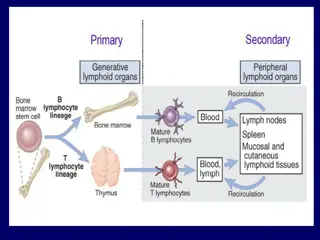
Transplantation of Hematopoietic Stem Cells(HSC) Hematopoietic stem cell (HSC) transplantation is used as therapy for: 1. Hematopoietic malignancies.e.g. Leukemia 2. Aplastic anemia s. 3. Certain inherited disorders e.g. immune deficiency states and severe forms of thalassemia. Transplantation of Hematopoietic Stem Cells(HSC) Sources of Hematopoietic Stem Cells for Transplantation: 1. from donor bone marrow, 2. from the umbilical cord blood of newborns, a readily available rich source of HSCs.
The recipient receives chemotherapy and/or irradiation to destroy malignant cells (e.g., in leukemia) and to create a graft bed; then, HSCs are infused into the peripheral blood, from which they home to bone marrow. Rejection of allogeneic HSC transplants seems to be mediated by some combination of host T cells and NK cells that are resistant to radiation therapy and chemotherapy.
graft-versus-host disease(GVHD) :This occurs when immunologically competent T cells (or their precursors) are transplanted into recipients who are immunologically compromised. 1. Acute GVHD (occurring days to weeks after transplantation): causes epithelial cell necrosis in three principal target organs: liver, skin, and gut. Chronic GVHD may follow the acute syndrome or may occur insidiously. The patients develop skin lesions resembling those of systemic seclerosis.
Primary immunodeficiencies are usually hereditary and manifest between 6 months and 2 years of life as maternal antibody protection is lost. Secondary immunodeficiencies result from altered immune function due to infections, malnutrition, aging, immunosuppression, irradiation, chemotherapy, or autoimmunity.
X X- -Linked Definition: inherited immunodeficiency characterized by developmental failure to produce mature B cells and plasma cells, resulting in aggamaglobulinemia Result from genetic mutation of B cell kinase(BTK B-cell maturation, T cells are entirely normal. Linked Agammaglobulinemia Agammaglobulinemia ( (Bruton s Bruton s Agammaglobulinemia Agammaglobulinemia): ): B cell bruton bruton tyrosine tyrosine kinase(BTK)(normally expressed in early B cells and is critical for Clinical finding: Male infant Recurrent infections beginning at 6 months of life Common infections: pharyngitis, otitis media, bronchitis, and pneumonia Organisms: H.influenza, s. pneumococcus, and staph aureus
DiGeorge definition: embryologic failure to develop the 3rd and 4thpharyngeal pouches, resulting in the absence of the parathyroid gland and thymus DiGeorge syndrome syndrome: : clinical findings: hypocalcemia and tetany T cell deficiency Recurrent infection with viral and fungal organisms
Severe combined immunodeficiency (SCID) Definition: combined deficiency of both cellular and humoral mediated immunity due to stem cell defect Severe combined immunodeficiency (SCID) Mode of inheritance X-linked ( chemokine receptor mutation) Autosomal recessive ( deficiency of adenosine deaminase) Clinical features: Susceptible to candida cytomrgalovirus and pneumocystic carini infection Other Wiskott Aldrich syndrome Isolated IgA immunodeficiency Hyper IgM syndrome Genetic deficiency of the complement Other immunodeficiency disease: immunodeficiency disease:
Thank you Thank you