Anti-diuretics
Anti-diuretics are substances that inhibit water excretion without affecting salt excretion, primarily used in conditions like diabetes insipidus. They work by acting on specific receptors in the body, influencing water permeability and blood pressure regulation. Learn more about anti-diuretics, their classifications, synthesis, and actions in this detailed guide.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
What are Anti-diuretics? Substances that inhibit water excretion without affecting salt excretion. Reduce urine output . More precise term anti-aquaretics Primary indication - diabetes insipidus
Drug classification Anti-diuretic hormone: ADH/Vasopressin, Desmopressin, Lypressin, Terlipressin Thiazide Diuretics: amiloride. Miscellaneous: indomethacin, chlorpropamide, carbamazepine
ADH Synthesis: posterior pituitary secretes both ADH and oxytocin. Regulation: osmoreceptors in hypothalamus volume receptors in left atrium, ventricles, pulmonary veins. Stimulus: rise in plasma osmolarity contraction of ECF volume. Human form: 8-arginine- vasopressin.
ADH receptors G protein coupled cell membrane receptors Types: V1 and V2 V1 receptors: all except on renal CD cells, AscLH cells and vascular endothelium. Subtypes: V1a and V1b V1a: vascular, uterine, visceral smooth muscle, adipose tissue, brain V1b: anterior pituitary, brain and pancreas.
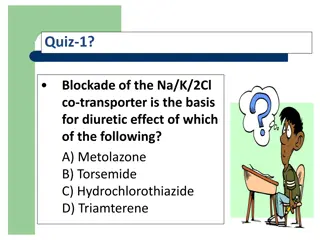
ADH receptors V2 receptor: more sensitive . location: collecting duct in kidney: regulate water permeability AscLH cells: activate Na/K/2Cl transporter . vascular endothelium: vasodilator
Actions Kidney: Acts on CD cells , increase the permeability. Water gets absorbed concentrated urine (hyperosmolar urine with same osmolarity of the medulla) Blood vessels: i. Constriction of blood vessels via v1 receptors Raises BP , Prolonged exposure causes smooth muscle hypertrophy.
Actions GIT: Increased peristalsis Evacuation and expulsion of gases Uterus: i. Contraction due AVP acting on oxytocin receptors. ii. Increases sensitivity to oxytocin. CNS: AVP doesn t penetrate blood brain barrier . Acts as a peptide neurotransmitter . Regulation of temperature . Systemic circulation . Task learning . ACTH release
Other uses: Platelet aggregation Hepatic glycogenolysis Coagulation factor VIII release Von willebrand s factor release
Mechanism of action V2R: Principal cells of collecting duct: increased aquaporins expression leading to increased water absorption decreased urine formed. Increased vasopressin regulated urea transporter expression in terminal CD cells , increased medullary hypertonicity ,increased water absorption , decreased urine formed.
V1R: Constricts vasa recta: diminished blood flow to inner medulla; reduces washing off effect and helps in maintaining high osmolarity; contributing to antidiuresis
AVP interactions Lithium, demelocycline; partially antagonise AVP action (limit CAMP formation) NSAIDS (indomethacin): augments AVP {increased renal PG synthesis} Carbamazepine, chlorpropamide: potentiates AVP action on kidney.
AVP uses Based on V2 actions: i. Diabetes insipidus ii. Bedwetting in children iii. Nocturia in adults iv. Renal concentration test v. Hemophilia, von willebrand s disease Based on V1 actions: i. Bleeding esophageal varices Before abdominal radiography
Adverse effects Transient headache Flushing Nasal irritation Congestion Belching Nausea Hyponatremia and fluid retention
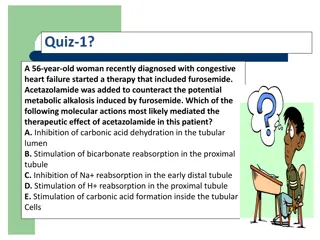
Thiazides Paradoxical anti-diuretic effect in DI Short and brisk action Low efficacy Valuable in renal DI as AVP is ineffective Induce state of sustained electrolyte depletion. Reduce GFR and fluid load Hydrochlorothiazide 25-50mg TDS
Other antidiuretics Amiloride: indomethacin i. Drug of choice, reduce polyurea in renal DI. ii. Reduces renal PG synthesis Chlorpropamide: i. long acting sulphonylurea oral hypoglycemic ii. Sensitizes the kidney to ADH action. Carbamazepine: anti-epileptic