Antibiotic Use and Selection in Infections
Antibiotics are commonly prescribed for bacterial infections, with indications based on clinical assessments and culture results. This guide covers the focus of infection, likely organisms, common causes for infections, culture result interpretation, and factors influencing antibiotic selection. Learn about antibiotic excretion, safety in pregnancy, and key considerations in choosing the right treatment. Stay informed to optimize antibiotic therapy for effective management of infections.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Antibiotic use Antimicrobials are the 2ndmost common drugs prescribed by office based physicians In USA1992: 110 million oral antimicrobial rx written by office based physicians annual antimicrobial drug use rate = 439 /1,000 populaation
A 21 year old university student presents with fever , body aches , and sore throat. A 54 year old lady complains of dysuria , frequency, loin pain and fever. A 36 year old man presents with cough , sputum , shotness of breath and fever
Indications for use : Definite or probable bacterial infection Serious infections NOT FEVER
Where is the focus of infection ? Clinical assessment Gram stain & cultures
What is the likely organism : focus of infection gram stain patients age epidemiological setting prior culture data
What is the commonest cause of : urinary tract infection cellulitis billiary infection meningitis septic arthritis nosocomial pneumonia
After 48 hours check culture results > Narrow antibiotic coverage >Infection vs colonization
Other factors for antibiotic selection : culture results tissue penetration bactericidal vs static renal disease liver disease pregnancy & lactation
Antibiotics excreted mainly by kidney Antibiotics excreted mainly by liver Antibiotics safe in pregnancy
Dosing of antibiotics depends on : MIC half life of drug patient factors Duration of therapy :
Antibiotic combinations Indications : Sepsis of unclear etiology Febrile neutropenia Prevent emergence of resistance Polymicrobial infection Synergy Disadvantages: Elimination of normal flora Colonisation by resistant organisms Drug toxicity Cost
Failure of therapy Patient factors Drug factors Organism factors
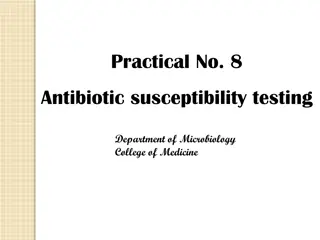
History of resistance Antibiotic Discovered Introduced Resistance into Clinical Identified Use Penicillin 1940 1943 1940 Streptomycin 1944 1947 1947 Tetracycline 1948 1952 1956 Erythromycin 1952 1955 1956 Vancomycin 1956 1972 1987 Gentamycin 1963 1967 1970
INCREASING ANTIBIOTIC RESISTANCE S. pneumoniae H. influenzae 50% 40% % of Total 30% 20% 10% 0% 1970 1975 1980 1985 1990 Year 1995 1997 1998
Antibiotic Resistance Current problems with antibiotic resistant bacteria include: MRSA 37% of all bloodstream isolates of S. aureus are now MRSA resistance in respiratory pathogens 2.2% of S. pneumoniae are penicillin-resistant ~15-20% of H. influenzae are amoxicillin-resistant
Antibiotic Resistance multi-resistant Gram-negative bacilli extended-spectrum -lactamase producers glycopeptide-resistant enterococci 21.6% of bloodstream isolates of E. faecium 3.3% of E. faecalis MDR-TB 6.2% of M. tuberculosis isoniazid-resistant 1% are true MDR strains
Stop Antimicrobial Treatment When infection is treated When infection is not diagnosed When infection is unlikely
Hospital Control: Monitor 2-Monitor and evaluate empiric, therapeutic & prophylactic use prescriptions include type of rx: E/T/P Time limits Empiric: Prophylactic: 2 days Therapeutic: 7 days 3 days extension requires justification written by the prescribing physician requiring MD to justify prescriptions proper usage.