Anuria Post Renal Transplantation Complications
Anuria post renal transplantation can be caused by various factors including prerenal, postrenal, and renal causes. Vascular complications such as renal artery thrombosis and renal vein thrombosis are rare but critical issues that require immediate attention to prevent graft loss. Risk factors for delayed graft function and treatment approaches for acute tubular necrosis are also discussed in this comprehensive overview.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Causes Prerenal Dehydration Post opaerative vascular complication ( renal artery thrombosis, renal vein thrombosis, hemorrhage and rupture of renal artery) Postrenal Urinary tract obstruction and it may be Intraluminal ( blood clots , stone and kinks) External compression edema , hematoma (early) lymphoacele (late) Renal Allograft rejection (hyper acute , acute and chronic ) Toxic ATN ( drug induced)
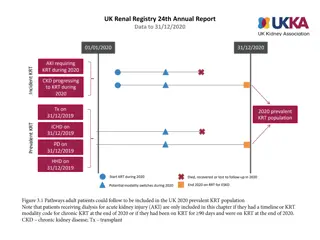
prerenal causes Ischemic ATN is one of the most common causes of DGF (delayed graft function ) Delayed graft function (DGF), defined as oliguria or anuria that necessitates dialysis during the first 7 days after kidney transplantation Other causes of ATN includes antibody-mediated rejection cortical necrosis/infarction endothelial damage drug-induced interstitial nephropathy, thrombotic microangiopathy. Donor tissue quality (ie, brain death, prolonged hypotension)
Risk factors for DGF include: older donor age prolonged warm and cold ischemia time diabetes as the cause of ESRD African American donor HLA mismatch, duration of dialysis ischemia/reperfusion injury. There is no treatment for ATN. If the kidney is viable (as determined by studies demonstrating vessel patency [ultrasound] and flow [radionuclide imaging]), patients are returned to dialysis and receive medical care for acute renal failure until kidney function returns. The expected outcome is that the kidney will begin clearing creatinine within approximately 4 weeks. During this time it is important to monitor fluid status,
Vascular complications Renal artery thrombosis Incidence : rare 0.2% Renal artery thrombosis is an early (within the first 2 days post transplantation) technical complication Causes Poor alignment of the intima Intimal injury Too long vessels (torsion) it is an indication of surgical exploration immediately without delay as if the ischemia time exceeded 30 minutes it will lead to loss of the graft
renal vein thrombosis Renal vein thrombosis is also an early (within the first 2 days post transplantation) technical complication Incidence rare 1-3.6% : Causes compression of the renal vein by fluid collection coagulopathy hypovolemia surgical technique(too long vein ) clinical presentation includes sudden oliguria or anuria, graft tenderness and swelling, and edema of the lower extremities that is more pronounced in the ipsilateral thigh and leg. Diagnostic methods include nuclear scan, ultrasound, angiography, and surgical exploration. If thrombosis is not complete, treatment includes heparinization and thrombectomy and insertion of a caval umbrella to prevent showers extension in cases of ileo-femoral vein thrombosis
Renal artery stenosis The most common vascular complication of kidney transplantation Incidence : 5% Causes atherosclerosis of the donor artery suture technique (stenotic running sutures) trauma to either donor or recipient artery reaction to the suturing material compression by fibrous reaction Transplant renal artery stenosis is more common at the site of the anastomosis of the donor artery to the native artery (surgical technique) and less common post anastomotic (intimal injury, perforation by cannula). Or it amy be multiple stenosis ( chronic rejaction or rec episodes of acute rejection
The clinical presentation of renal artery stenosis typically includes severe hypertension that is often refractory to treatment oliguria / anuria bruit can be heard over the femoral vessels or over the graft A bruit is not always diagnostic of transplant renal artery stenosis because a bruit may be caused by altered blood flow in the iliac arteries. However, auscultation of a new-onset bruit coupled with severe hypertension is highly suggestive of transplant renal artery stenosis and warrants immediate investigation. This complication is most commonly diagnosed by Doppler ultrasonography ( high PSV over the stenotic area) selective graft arteriography ( detect site extent of the stenosis) graft biopsy ( in case of chronic rejection )
The treatment of transplant renal artery stenosis includes percutaneous transluminal balloon renal angioplasty (PTRA) with 80% success rate surgical intervention with success rate of 50% and incidence of 25% graft loss due to tense adhestion and difficult dissection . Transplant renal artery stenosis is associated with an increased risk for graft loss as a result of unsuccessful treatment with PTRA, complications of surgical intervention, and chronic rejection. The expected outcome is successful treatment of the stenotic vessel; however, treatment may not totally correct the problem. Careful monitoring of blood pressure for hypertension becomes a long- term need in order to preserve graft function.
Post renal causes Urinary Tract Obstruction Anuria due to acute allograft failure can occur as a result of obstruction of the urinary tract, usually early in the postoperative period. The urinary tract can become obstructed by intraluminal blood clots, kinking, external compression from edema or hematoma (immediate) or lymphocele (late), bladder retention, inflammation secondary to urine leak
lymphocele a collection of lymphatic fluid around the renal allograft caused by leakage from lymphatic vessels severed during the transplant surgery Lymphocele occurs in up to 20% of kidney transplant recipients Lymphocele can develop early (within the first year) or late (up to 4 years after transplantation). There are 2 origins of lymphocele: (1) donor lymphatics, and (2) native lymphatics. Lymphoceles that arise from donor lymphatics collect immediately adjacent to the allograft and tend to obstruct the proximal ureter and urine outflow to the bladder. Lymphoceles that arise from native lymphatics collect in an area more distant from the allograft (ie, proximal to the native iliac vessels) and tend to obstruct venous drainage from the leg, resulting in obstruction of blood flow to the allograft or deep vein thrombosis, and edema of the ipsilateral lower extremity.
Clinical picture includes edema of the leg on the side of the graft, tenderness over the incision mild-to-moderate abdominal discomfort. If the lymphocele is large (> 5 cm), urinary output may decrease, leading to a presumptive diagnosis of acute rejection. Diagnosis of lymphocele is made via ultrasound. Aspiration of clear fluid with a creatinine level similar to the serum creatinine level is also diagnostic of a lymphocele. Depending on the size of the lymphocele and the clinical presentation, interventions include observation, aspiration, and surgical creation of a window into the peritoneal cavity. Avoiding infection is the primary concern once treatment has been implemented
urinoma, a technical complication resulting in a collection of urine outside the bladder incidence : up to 3% of kidney transplant recipients. Causes trauma to the ureter during dissection ureteral necrosis as a result of ischemia acute rejection. Less commonly, urine leaks occur as a result of leakage from the anastomosis (eg, inadequate suture line, failure to keep the bladder decompressed during the early postoperative period).
Clinical picture suprapubic pain suprapubic mass fever. Anuria and elevated serum creatinine are less common signs. Diagnosis of a urine leak is verified by an ultrasound that reveals a fluid collection. When aspirated, the fluid has a high creatinine level compared with the serum creatinine in a patient with a functioning graft. The diagnosis is more difficult in the setting of DGF. A diagnosis can also be made via cystogram that shows contrast media outside of the bladder. A small leak can often be treated with prolonged urinary catheter drainage to relieve pressure. Surgical treatment options include reimplantation of the ureter or anastomosis of the native ureter to the transplant ureter over a stent. After treatment, it is imperative to keep the bladder decompressed so that the sutures can heal.