ARCPs: Ready for Progress in Paediatrics
"The purpose and timing of ARCPs in paediatric training, understand your role as a specialty doctor, and learn how to manage your learning effectively. Key messages include competency mapping, formative and summative assessments, and setting SMART objectives."
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
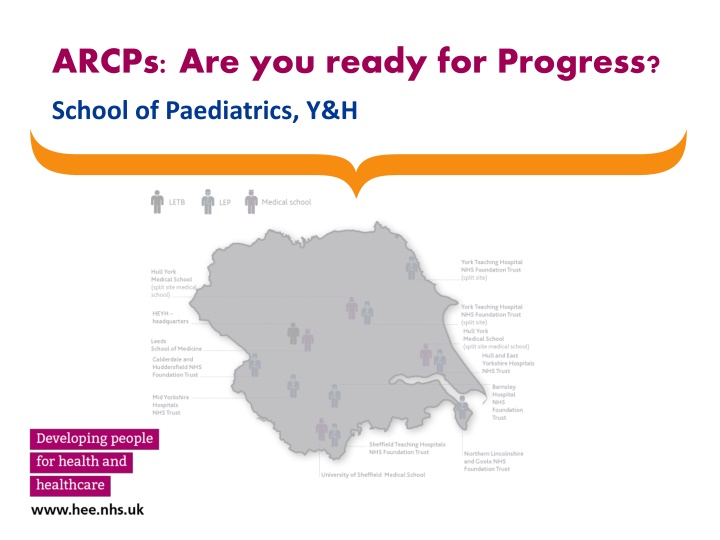
ARCPs: Are you ready for Progress? School of Paediatrics, Y&H
Key messages Tag all entries SLEs, Dev and Skills Log Domain and level of competency Map learning to RCPCH Domains Clinical and non-clinical Level of competency your level or above Demonstrate progression 3
ARCPs - Purpose Summative assessment Assess each training year Progress to next training year? Gained competencies at each level? Confirm/ recalculate CCT date Recommendation for revalidation Formative assessment and guidance Provide feedback on e-portfolio Set SMART objectives for next training year 4
ARCPs Timing (1) ARCP assessment only done during training Assess each training year Annual ARCP Pass to next training year?........ At the end of each training year Gained competencies at each level?............. And end of level Absences from training (OOPC/ OOPE/ OOPR) During OOP: Form R reviewed, ARCP outcome 0 (non-assessment) Before OOP: outcome 1 is essential prior to OOPE/R/T Inform HEE if you are planning to apply for OOPE/R/T/C
ARCPs Timing (2) Acceleration through training Educational supervisor and TPD s recommendation interim Advance to next training year Early outcome 6 (completion of training) Doctor needs additional support/ training When concerns flagged by ES/ CS TPD s recommendation Review after adverse outcome: 3 - 6 months
Your role as a Specialty Doctor in Training (1) Manage Learning & Collect Evidence of Progress Keep e-portfolio up to date Initiate supervision meetings and reports Initiate assessments (SLEs, MSF, START) and respond to feedback Meet ARCP requirements by deadline (on School website)
Your role as a Specialty Doctor in Training (2) Keep Up to Date with Requirements for Training Maintain contact with HEE and TPD Act on and respond to emails Familiarise yourself with RCPCH Curriculum and assessments GMC requirements HEE YH School of Paediatrics website YH Paediatrics ARCP e-portfolio review tool
ARCP STANDARDS Progress Curriculum Progress in ALL Generic Professional Capabilities in each LEVEL Level 1 ACQUIRE KNOWLEDGE BASE Level 2 APPLY KNOWLDEGE TO CLINICAL PRACTICE DEMONSTRATE AUTONOMY Level 3 DEVELOP PROFESSIONAL EXPERTISE, ANALYSE & EVALUATE KNOWLEDGE, TEACH & DEVELOP OTHERS
Progress Curriculum (1) Progression in all GPCs relating to direct clinical care is mandatory in each training year Professional Values and Behaviour Professional Skills and Knowledge Communication Clinical Procedures Patient Management Safeguarding Health Promotion and Illness Prevention Patient Safety - includes Safe Prescribing
Progress Curriculum (2) Level 1: Progress in one or more of the non- clinical GPCs is mandatory during each year Level 2 & 3: Progress in two or more non-clinical GPCs is mandatory during each year Leadership and Team working Quality Improvement Education and Training Research
E-portfolio Evidence Required for ARCP 1) MANDATORY: (RCPCH and YH HEE) 2) OPINIONS: Supervisors meetings and reports 3) ASSESSMENTS: Summative and formative 4) DEMONSTRATION OF PROGRESS: Your evidence
Evidence in ARCP folder (1) Mandatory (RCPCH) Form R completed and signed GMC survey receipt Up to date Curriculum vitae Mandatory courses (APLS, NLS/ ARNI, Safeguarding as per level) Essential (HEE YH) Tag ALL SLEs and entries in development and skills log Completed CCT calculator Panel will calculate date of end of training year and CCT
Evidence in e-portfolio TAGGING Tag EVERYTHING SLEs, Skills & Development log Tag Domain Tag Level of competency If you do not tag, the ARCP panel may not see and give you credit for it
Supervisors Opinions (1) Clinical supervisor Observation and feedback from MDT Educational supervisor (triangulates evidence) Clinical Supervisor s Trainer s Report Assessments (MSF, SLEs & START) Your evidence development & skills log
SUPERVISION MEETINGS & REPORTS (2) Number of meetings per 6 month placement/ calendar year same for FT and LTFT CLINICAL SUPERVISION (3 meetings/6 months calendar placement EDUCATIONAL SUPERVISION (3 meetings/year) One may be via phone CSTR post 2 previous year CS Trainer s report Long term career goals: Post 1 Post 2 Essential Essential Essential Initial meeting and Personal development plan Essential Essential Essential Mid-point review Essential Essential End of term Essential Essential Trainer s report
Assessments - Summative and Formative (3) Multi-source feedback and START Reflection Address areas for development Supervised Learning Events Generate Learning Objectives SMART PDP Evidence of achieving the objectives Development and Skills Log SLEs
DEMONSTRATE PROGRESS IN TRAINING Experience Assessments (SLEs, MSF) Reflection Learning objectives/ CPD &/or Development Skills log PDP
Assessments LEVEL 1 ACQUIRE KNOWLEDGE BASE MSF 1/per calendar year (not training year) unless OOP Separate MSF - general paediatrics and neonatal placements MRCPCH EXAMINATIONS: ST1: 1-2 written exams desirable ST2: 2 written exams essential ST3: Full MRCPCH exam essential SUPERVISED LEARNING EVENTS: At least one of each mandatory SLE by consultant or senior SSAG/ speciality doctor Demonstrate learning reflection develop SMART PDPs and complete objectives
MANDATORY ASSESSMENTS: LEVEL 1 Mandatory clinical cases (per level): Respiratory, gastroenteritis, convulsions, fever, rash, abdominal pain DOPS: 1 each in level 1: bag & mask ventilation tracheal intubation of newborn infants peripheral venous cannulation umbilical venous cannulation lumbar puncture Safeguarding CBD: 1/training year Demonstrate knowledge of recognition and response as per level 2 safeguarding training HAT: 1/level Demonstrate appreciation of patient safety, risk, ability to prioritise clinical issues CBDs: Minimum 1, suggest 4 Demonstrate reasoning, decision making, application of knowledge to patient care Mini-CEX: Minimum 1, suggest 4 Demonstrate good clinical care
ASSESSMENTS: LEVEL 1 Demonstrate learning: reflection, develop SMART PDPs, and complete objectives ACAT: Demonstrate ability to assess risk and prioritise tasks when managing clinical workload in acute settings over a period of time day shift DOCS: Letters referral/ clinical/ discharge, medical reports, medical notes Demonstrate ability to document pertinent information accurately LEADER: Apply to a clinical case or clinical problem how could the management of this situation be improved?
Assessments LEVEL 2 (slide 1) APPLY KNOWLDEGE TO CLINICAL PRACTICE, DEMONSTRATE AUTONOMY MSF 1/per calendar year (not training year) unless OOP One each in general paediatrics, community child health and neonatal placements SUPERVISED LEARNING EVENTS: Must complete SLEs in all these settings: General paediatrics, neonates, community child health, ward and out-patient clinics. SUPERVISED LEARNING EVENTS: At least one of each mandatory SLE by consultant or senior SSAG/ speciality doctor Demonstrate learning reflect develop SMART PDPs complete objectives
MANDATORY ASSESSMENTS: LEVEL 2 (slide 2) Demonstrate learning: reflect, develop SMART PDPs, complete objectives Safeguarding CBD: 1/training year Demonstrate skills to assess, form and opinion and manage per level 3 safeguarding training HAT: 1/ training year Demonstrate plans to maximise patient safety, minimise risk and prioritise and action relevant clinical tasks LEADER: 1/training year Apply to a clinical case or clinical problem- how will you improve your leadership and the NHS system? ACAT: mandatory 1/level Demonstrate autonomy in managing clinical workload in an acute setting over a period of time day shift DOCS: 5/level Letters referral/ clinical/ discharge, medical reports, medical notes
ASSESSMENTS: LEVEL 2 (slide 3) DOPS: Demonstrate autonomous practice and evolving proficiency to deal with complications CBDs: Minimum 1, suggest 4 Demonstrate reasoning, decision making, application of knowledge to patient care Mini-CEX: Minimum 1, suggest 4 Demonstrate good clinical care
Assessments LEVEL 3 (slide 1) DEVELOP PROFESSIONAL EXPERTISE, ANALYSE & EVALUATE KNOWLEDGE, TEACH & DEVELOP OTHERS MSF 1/per calendar year (not training year) unless OOP ST8: Must support ability to perform at consultant level by CCT date START: Must demonstrate completion of learning objectives highlighted in feedback Demonstrate this in skills and develop log and through SLEs CSAC PROGRESSION FORM: Doctors undertaking Subspecialty Grid training
MANDATORY ASSESSMENTS: LEVEL 3 (slide 2) SUPERVISED LEARNING EVENTS: At least one of each mandatory SLE by consultant or senior SSAG/ speciality doctor Demonstrate learning reflect develop SMART PDPs and complete objectives Safeguarding CBD: 1/training year Demonstrate ability to take overall responsibility in managing safeguarding issues in CYP LEADER: 1/training year Demonstrate leadership in improving own and team s performance, and in improving NHS clinical systems HAT: 1/level Demonstrate appreciation of patient safety, risk, ability to prioritise clinical issues DOCS: 5/level Letters referral/ clinical/ discharge, medical reports, medical notes
ASSESSMENTS: LEVEL 3 (slide 3) Demonstrate learning: reflection, develop SMART PDPs, and complete objectives DOPS: Demonstrate autonomous practice and evolving proficiency to deal with complications HAT: Demonstrate leadership in managing team to maximise patient safety, minimise risk and prioritise and action relevant clinical tasks ACAT: Demonstrate leadership skills in managing clinical team in an acute setting over a period of time day shift CBDs: Minimum 1, suggest 4 Demonstrate reasoning, decision making, application of knowledge to patient care Mini-CEX: Minimum 1, suggest 4 Demonstrate good clinical care
Evidence Presented by You for ARCP (4) E-portfolio of learning Response to SLEs, MSF and START Personal development plan - GOALS Development log Skills log
Responses to SLEs, MSF and START (3) IDENTIFY learning objective(s) DEVELOP SMART PDP Evidence of achieving GOAL
Personal Development Plan COMPLETE SMART PDP REVIEW Dev / Skills Log Assessments Clinical GPCs Non- Clinical GPCs Regularly Set new goals
Development Log (3) Professional values & behaviours, Communication Patient Safety safe prescribing Clinical procedures, Leadership and Teamwork Health Promotion & Illness Prevention Patient management, Quality Improvement Safeguarding Educational and Teaching Research
Skills Log (3) Expert Can teach Proficient Autonomous practice Competent Knows > Knows how > Shows how > Does 32
Key messages TAG EVERYTHING RCPCH Domains PROGRESSION through levels 33
Take home message TAG! 34