Basic Concepts in Noninvasive Positive Pressure Ventilation
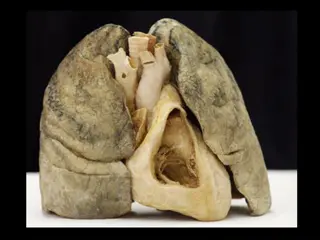
This presentation covers the basic concepts of noninvasive positive pressure ventilation and includes information on indications, exclusion criteria, and pressure-targeted ventilators such as CPAP, PSV, and S/T modes. It explains how these ventilators work and their modes of operation to support patients' breathing effectively.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Basic concepts in noninvasive positive pressure ventilation Presentation by: Dr mohammadreza zeraati M.D. FCCM DR Ali reza Zeraatchi M.D Specialist of Emergency medcine Dr mitra Hojatansari M.D Anesthesilogist
B Basic concepts in noninvasive positive pressure ventilation
E Exclusion criteria for non invasive positive pressure ventilation
P Pressure targeted ventilators CPAP (Spontaneous) PSV (IPAP-EPAP) SPONTANOUS TIMED (S/T) In the CPAP mode the patient breathes spontaneously at a set baseline pressure. The patient controls both the rate and depth of breathing. Flow sensors and pressure transducers respond to the patient s inspiratory and expiratory effort and increase or decrease flow through the circuit to maintain a stable level of pressure.
Pressure targeted ventilators Pressure targeted ventilators With the PSV (bilevel) mode, the difference between two pressure levels (IPAP and EPAP) determines the level of pressure support for each assisted breath. A change to the set IPAP occurs only in response to the patient s inspiratory effort. When the patient reaches a predetermined flow threshold, the breath is terminated and the patient exhales to the set EPAP level. There is no set rate; the patient must initiate each breath.
PRESSURE TARGETED VENTILATORS PRESSURE TARGETED VENTILATORS In the S/T mode (older models may use the term A/C), the clinician sets the IPAP and EPAP, a respiratory rate, and an inspiratory time (e.g., IPAP%). The patient may initiate breaths that are supported to the IPAP level, as in the PSV mode, but if the patient fails to make an inspiratory effort within a set interval, the machine triggers inspiration to the set IPAP level. IPAP then cycles to EPAP based on the IPAP% period.
PRESSURE TARGETED VENTILATORS PRESSURE TARGETED VENTILATORS In all modes of bilevel positive-pressure ventila tion, the patient s delivered V T depends on the gradient between the IPAP and EPAP, the inspiratory time, and the patient s inspiratory effort and lung characteristics. AVAPS devices operate with several modes of ventilation, including CPAP, S/T, spontaneous, timed, and PCV. The manufac turer s suggested setting for initiating AVAPS include a target VT of 8 mL/kg, ideal body weight (IBW), maximum IPAP of 25 cm H2 O (depending on the patient s pathology), minimum EPAP of +4 cm H2 O, respiratory rate 2 to 3 beats/min below resting respiratory rate, and an inspiratory time of 1.5 seconds
PRESSURE TARGETED VENTILATORS PRESSURE TARGETED VENTILATORS A pressure-targeted ventilator s ability to deliver flow in response to patient demand is equivalent and often superior to that of ICU adult ventilators and portable homecare ventilators.
P Pressure targeted ventilators Most units now have adjustable inspiratory and expiratory sensitivity controls that improve synchronization between the patient and the ventilator. Pressure-targeted ventilators also allow adjustment of the amount of time required to reach the IPAP (i.e., risetime control). Use of the rise-time control may enhance patient comfort, reduce WOB, and improve patient-ventilator synchrony. Two other features of portable PTVs that can enhance patient comfort are the ramp and delay-time controls. Ramp allows positive pressure to increase gradually over a set interval (delay time). The ramp rate generally can be set in increments of 1, 2, or 3 cm H2 O, and the delay time can be set in 5-minute increments between 5 and 30 minutes. The ramp and delay-time controls are more likely to be used in home or chronic care NIV.
Pressure Pressure targeted ventilation targeted ventilation the FI O 2 can vary and is affected by four factors: Oxygen flow rate Type of leak port in the system Site where oxygen is bled into the circuit IPAP and EPAP To prevent CO 2rebreathing, EPAP level should be set at 4 cm H2 O or higher so that adequate gas flows can flush CO 2 from the breathing circuit.
Interfaces Interfaces
Appropriate mask size Appropriate mask size