Behavioral Health Care Integration Pathways at Beth Israel Deaconess Hospital-Milton
Explore the initiative at Beth Israel Deaconess Hospital-Milton focusing on care integration pathways for behavioral health patients to address ED boarding issues, improve patient care, and reduce length of stay.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Care Integration Pathways for Behavioral Health Patients in Beth Israel Deaconess Hospital-Milton s Emergency Department Marian Girouard-Spino, RN, MSN, CCM Director of Care Integration Lisa Braude, PhD Senior Advisor, Health Policy & Grant Management Ashley Yeats, MD, FACEP Vice President of Healthcare Quality & Clinical Integration/Chief Medical Officer
Statement of the Problem & Intervention Prolonged ED boarding of BH patients contributes to ED crowding and impedes timely access to ED services Care Integration activities assure accuracy of medication reconciliation in the ED and the development of individualized care plans which ensure comprehensive assessment of collateral patient information and effective handoffs across care transitions.
Key Issues Approx. 95% of all ED boarding was accounted for by ED behavioral health (BH) boarders (~40/month) w/ boarding for up to 21 days in the ED awaiting inpatient psychiatric placement. 1% of ED patient registrations and consumed 11% of ED resources, impeding access of other acute patients to ED services. More than 3 BH boarders (defined as boarding in the ED for more than 2 hours after the decision to admit/transfer to a higher level of care) was strongly associated with DPH mandated activation of Code Help disaster plan activation.
Program Goal Support the Care Integration Program (CI) to reduce ED length of stay & improve patient care for boarding long- stay (>8hours) BH patients perpetuated by spike in ED volume: Closure of Quincy Medical Center Shortage of inpatient psychiatric beds Statewide opioid crisis Changing patient demographics
Overview of the Care Team Masters-prepared RN Director of Care Integration Two co-located Licensed Independent Clinical Social Workers from the regional Behavioral Health Emergency Services Provider (South Shore Mental Health) Part-time Music Therapist & Chaplain ED physician and RN champions Pharmacist Security officer Administrative & analytical support
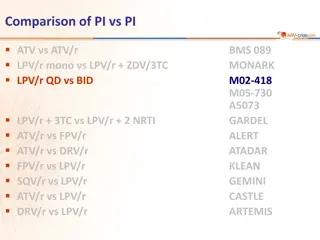
Key Outcome Based on Equation of Line, Trend Over Time Oct-14 Dec-16 % Change 3.49 3.76 8% ER LOS 35.73 30.72 -14% BH Boarder LOS In spite of the December 2014 closure of Quincy Medical Center leading to a spike in ED volume and BH boarding, a shortage of inpatient psychiatric beds and a statewide opioid crisis, the Care Integration Team was able to reverse an upward trend in length of stay for BH patients. FY16 interventions resulted in a 14% average LOS reduction for BH boarders, reversing and upward trend and 30% increase in FY15.
Lessons Learned There are significant gaps in the construct of a traditional ED model of care which impede care to ED BH boarders and the ability to provide optimal milieu management. There are barriers within state agencies and payer organizations that perpetuate emergency department patient boarding for BH patients. Barriers to electronic record sharing between disparate providers impede a seamless, integrated and coordinated system of care. Early identification, ED treatment intervention and coordination with community resources decreases ED BH boarding, recidivism and utilization.
For more information, contact: Marian Girouard-Spino RN, MSN, CCM Director - Care Integration Phone: 617-313-1650 Fax: 617-313-1518 Email: Marian_GirouardSpino@bidmilton.org