BLS Resuscitation Scenario: Emergency Response for Unresponsive Patient
You are dispatched to assist an unresponsive 78-year-old man at home. Quickly assess the situation, perform necessary actions, and follow proper resuscitation protocols. Learn about pulse checks, chest compressions, defibrillation, and ventilation techniques in this challenging scenario.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Chapter 13 BLS Resuscitation
Part 1 You are dispatched as a BLS crew to 401 Oak Hill Road for a 78-year-old man whose wife says he fell off the toilet and she can t get him up. An elderly woman greets you at the door and tells you her husband isn t answering her now. She takes you to a small bathroom where you find an unresponsive man between the toilet and a wall.
Part 1 You call to the gentleman, but there is no response, and you note that he is not breathing except for an occasional gasping sound. You and your partner quickly extract him to an open area. While you are checking for a carotid pulse, you tell your partner to call for ALS and report a cardiac arrest.
Part 1 1. How long should you check for a pulse at the carotid artery? 2. What should you do now?
Part 2 You continue chest compressions as your partner applies the defibrillation pads to the patient s chest, and you then follow the AED s verbal directions to defibrillate the patient. You immediately have your partner resume compressions while you prepare to ventilate with a bag-valve mask (BVM).
Part 2 3. What is the ratio of compressions to ventilations that you and your partner should be using during resuscitation?
Part 3 While your partner is doing a cycle of compressions, you insert an oropharyngeal airway and prepare to ventilate at the end of the 30 compressions. You notice that your partner is compressing a little slowly and shallowly, so you encourage him to push harder and deeper and to pick up the pace of compressions.
Part 3 4. What is the depth at which your partner should be compressing, and at approximately what rate?
Part 4 After 2 minutes, the AED prompts you to clear for analysis, and then to push the shock button to defibrillate the shockable rhythm.
Part 4 5. What should you do after the shock is delivered? 6. How often will the AED prompt you to hold off CPR for analysis, and how often should the compressor and ventilator switch roles?
Part 5 After the third shock, you notice that the patient seems to be trying to take a breath, and his color seems to have improved. You continue your 2 minutes of CPR, and when the AED analyzes and says to check for a pulse, you find that the patient has a carotid pulse. However, the patient is only taking an occasional breath at a rate of about 4 breaths/min.
Part 5 7. What should you do now? 8. At what rate should you ventilate?
Summary As you are ventilating the patient and preparing to move him to the ambulance, the ALS crew arrives and switches to their monitor. The paramedic tells you that the patient now has a sinus rhythm, and that the 12-lead ECG shows signs that the patient probably has had a myocardial infarction. The paramedic asks you to get a blood pressure while an intravenous line is being started, and you report that it is 82/40 mm Hg. The heart rate is 72 beats/min and the oxygen saturation is 90%. The patient is intubated as he is still unresponsive and breathing slowly.
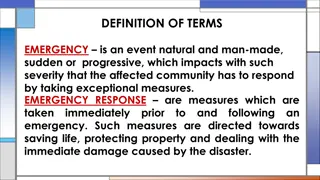
Summary It is essential to recognize cardiac arrest quickly because brain damage is possible after only 4 to 6 minutes without oxygen. An unresponsive patient should be assessed for adequate breathing and a carotid pulse for no more than 10 seconds. If pulseless, CPR is begun with compressions alternating with ventilations at a 30:2 ratio for adults.
Summary Compressions should be at a depth of 2 to 2.4 inches, or 5 to 6 cm, on the adult. The rate of compressions should be 100 to 120 per minute. The compressor and ventilator should switch every 2 minutes, as compressions become less effective when the compressor becomes fatigued.
Summary The automatic defibrillator (AED), or a manual cardiac monitor if ALS is on scene, should be attached to the patient as soon as possible, with immediate analysis and defibrillation if the rhythm is shockable. The rhythm should be analyzed every 2 minutes with defibrillation as needed, as long as the patient is being treated for cardiac arrest.