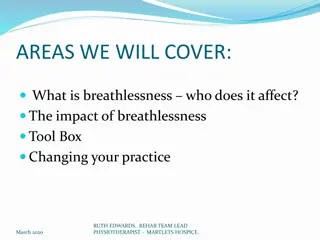
Breathlessness in Palliative Care Nursing
Explore the complexities of breathlessness in palliative care nursing, its impact on patients with cancer and non-malignant diseases, causes, psychological aspects, and assessment techniques. Learn about the prevalence, progression, and management strategies for this distressing symptom.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Breathlessness Barbara Mackie and Jo Lenton Community Specialist Palliative Care Nurses
Breathlessness Breathlessness is an uncomfortable sensation or awareness of breathing. Subjective measuring lung function does not correlate with sensation or severity of breathlessness A complex experience of mind and body that is likely to progress with disease severity Significant correlation with impaired quality of life and poor survival. Effects Patients and Carers. A common complex distressing symptom at the end of life
Prevalence of Breathlessness in cancer The prevalence of breathlessness varies with the primary tumour site; Breathlessness occurs as a symptom most frequently in lung cancer, where it might affect 75% of people with primary disease of the lung, bronchus and trachea (Muers & Round 1993).
Breathlessness in non-malignant disease For patients with COPD, intractable breathlessness develops late in the course of the disease, gradually increasing in severity over a period of years in the majority of people. There is a long pre-clinical phase when patients may not have any respiratory symptoms at all, although lung damage exists.
Breathlessness in non-malignant disease There is then a protracted period of gradual decline punctuated by severe exacerbations, which may be life- threatening and require inpatient management. Breathlessness tends to be associated with exertion. However at end of life it may be present at rest.
What are the Causes of Breathlessness?
Psychological Aspect of Breathlessness
Assessment of breathlessness Listen/Observe What does it mean to the patient / carer? Onset Triggers / What eases it? Levels of significance during activity, in different positions, at rest Pattern of breathing, colour, respiratory rate Are they anxious? Oxygen saturations
Manage reversible causes optimally according to patients wishes Consider active treatment of: Infection Pleural effusion Pneumothorax PE Airway obstruction SCVO Anaemia CCF
Non Pharmacological Management Positioning Airflow - use of fan /window Relaxation / Distraction/ Reassurance Energy conservation / Pacing Controlled Breathing techniques /physio Loose clothing Mouth Care
Breathing Techniques Start with position of ease Relax shoulders / upper chest Diaphragmatic tummy breathing Breath out twice as long as breath in Pursed lips on breathing out if needed
Relaxation Time and calm environment essential Relax and Breathe CD Visual imagery Calming hand Touch across back Distraction
. Pacing activities Encourage activity Allow time for tasks Starting and stopping with rest intervals Inspiration: expiration ratio during activity Use of aids stair lift etc Adapting functional tasks, e.g. Ironing sitting down
Pharmacological Management Opioids Opioids are the most effective pharmacological agents for the relief of dyspnoea Oral morphine (normal release) 2.5mg (if Opioid naive/elderly and renal impairment) Gradual titration upwards according to response High level evidence supports: Low dose slow release oral morphine for opioid na ve (10-20mg/24hours), .
Pharmacological management Benzodiazepines Lorazepam 0.5-1mg sublingual (SL) - rapid relief during panic attacks Diazepam (oral) for longer term management Midazolam 2.5mg subcutaneous 5 -10mg in Syringe driver over 24hrs Above medication are sedative, therefore should be monitored carefully. However in the terminal stages of illness the benefits usually out-weigh the risks.
Pharmacological Management Oxygen therapy only where appropriate (mixed evidence, check sats if hypoxic resting O2 below 90% 2l/min) Steroids Bronchodilators nebulised (Salbutomol 2.5 5mg prn) Antibiotics Nebulised saline to thin secretions or Carbocisteine if secretions difficult to expectorate and exacerbating breathing difficulties Blood transfusion
End of life secretions Often referred to as death rattle Caused when a patient s coughing and swallowing reflex is impaired or absent, causing fluids to collect Not easily relieved by drug therapy once established Treatment should therefore be started at first sign of rattle
Non-pharmacological management of secretions Re-positioning of the patient by tilting side to side, or tipping bed head up to reduce noise Management of halitosis with frequent mouth care and aromatherapy Discrete management of oral secretions mouth care oral hygiene Suction not advised, except when secretions are excessive Reassurance to family that the noise is due to secretions, and not causing suffocation, choking or distress Reduce oral fluids if at risk of aspiration
Pharmacological management of secretions Hyoscine Butylbromide (Buscopan) 60- 240mg/24hr s/driver, prn dose SC 20mg hrly If not effective, discuss with palliative care team who may consider - Glycopyronium Bromide (Glycopyrolate) 400-2400mcg/24hr s/driver or prn dose 200mcg NB: Hyoscine Hydrobromide was historically drug of choice, but not currently recommended due to side effects of sedation and confusion
References DAVIS.C(1998) Breathlessness,cough and other respiratory problems.In: FALLON.N.O NEILL.B(eds)ABC of Palliative Care BMJ Books. London pp 8-15 MUERS.M. ROUND.C (1993)Palliation of symptoms in Non Small Cell Cancer:A Study by the Yorkshire Regional Cancer Organisation Thoracic Group. Thorax.48 (7) 339-349 Sheffield Palliative Care Formulary 3rdEdition