Broker Services Partner Integrity Program
Explore the Broker Services Partner Integrity Program, how complaints are tracked, notifications process, and classification of commercial-related complaints. Learn about the resolution steps for complaints in the healthcare setting.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
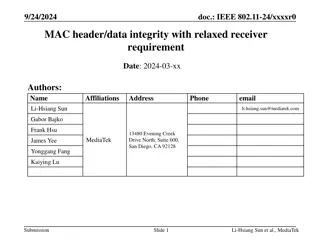
Broker Services Partner Integrity Program Broker Training 10142021
Module Description This module is designed to review: The Broker Services Partner Integrity Program How Health First Health Plans/AdventHealth Advantage Plans is notified of a complaint Immediate Need/Urgent Complaints Member s Right to File a Grievance Process Following a Notification How to Avoid a Complaint Complaint Resolution
What is the Broker Services Partner Integrity Program? The Broker Services Partner Integrity Program tracks complaints and/or concerns from the following: A member or prospective member in reference to a broker with any aspect of the Health Plans operations, activities or behaviors Any first-tier, downstream or related entity of the Health Plans The Health Plans takes each complaint seriously and responds accordingly to all complaint allegations.
Broker Complaint Notifications The Health Plans is notified of broker complaints by way of: Email communication Phone call to Health Plans representative Prospective member/member contacting the Centers for Medicare & Medicaid Services (CMS) directly Medicare complaints can also be received through the Health Plans Management Systems (HPMS) Complaints Tracking Module (CTM) All broker-related complaints will be routed to the Director of Sales and/or Manager of Broker Services for initial review to determine if founded or unfounded, and necessary steps to follow.
Commercial-related complaints are classified as either Immediate Need or Urgent Immediate Need Member expresses dissatisfaction with any broker activity or conduct that IS NOT related to: Privacy concern Access to care Premium payment Benefit misinterpretation Urgent Member expresses dissatisfaction with any broker activity or conduct that IS related to: Privacy concern Access to care Premium payment Benefit misinterpretation Note: Commercial encompasses both Group and Individual line of business
Medicare-related complaints are classified as either Immediate Need or Urgent Urgent Member expresses dissatisfaction with any broker activity or conduct that IS related to: Access to care but no immediate need exists Part D, when need for medication falls within three to 14 days of medication left Immediate Need Member expresses dissatisfaction with any broker activity or conduct that IS NOT related to: Access to care Limited access to medical services Part D services
Members Right to File a Grievance If a member calls with the intention of filing a complaint against a broker: Customer Service will document and track the call with details of the member s dissatisfaction. Customer Service will escalate to determine appropriate action, if applicable. If a member calls with the intention of filing an appeal or grievance against a broker: Customer Service will follow the appeal or grievance process at the request of the member. Appeals and Grievance department will review, research and follow up with the member on the outcome. Appeals and Grievance will notify the Manager of Broker Services and provide details of the appeal/grievance. The Manager of Broker Services will follow up with the broker on a formal outcome of the complaint. Grievances include but are not limited to the following: Unprofessional behavior Language or cultural competency issues Customer service, marketing or sales complaints Confidentiality or privacy issues Lack of access to records
Policy and Procedure for a Commercial Broker Complaint First Complaint A conference call will be held between the Broker Services Manager and the broker to determine if the complaint is founded or unfounded. Second Complaint An interview will be conducted between the Broker Services Manager, Sales Directors and the broker to determine if the complaint is founded or unfounded. Third Complaint If three or more complaints are received within the same calendar year, it is grounds for termination from selling all products at the discretion of the Health Plans. Details of the conversation and outcome will be documented and reported to the VP of Sales and the directors of Commercial, Individual and Medicare Sales. A field evaluation will also be conducted to determine any learning opportunities and improvements to sales techniques. The broker may be considered for reinstatement after no less than 12 months and subject to completing Broker Services onboarding and training programs. Details of the interview and outcome will be documented and reported to the VP of Sales and Corporate Integrity Officer. Florida Statutes: 30- to 60-day notice prior to termination
Policy and Procedure for a Medicare Broker Complaint Second Complaint An interview will be conducted between the Director of Medicare Sales (Medicare Supervisor or Broker Services Manager) and the broker to determine if the complaint is founded or unfounded. Third Complaint If three or more complaints are received within the same calendar year, it is grounds for termination from selling our Medicare products and possible appointment termination at the discretion of the Health Plan. First Complaint An interview will be conducted between the Director of Medicare Sales (Medicare Supervisor or Broker Services Manager) and the broker to determine if the complaint is founded or unfounded. A field evaluation will also be conducted to determine any learning opportunities and improvement to sales techniques. Results are reported to the Centers for Medicare & Medicaid Services (CMS). Details of the interview are reported back to the Centers for Medicare & Medicaid Services (CMS). Florida Statutes: 30 to 60 days notice prior to termination Details of the interview are reported back to the Centers for Medicare & Medicaid Services (CMS), VP of Sales, and Corporate Integrity Officer.
The Health Plans views broker-related complaints as critical The Health Plans will provide updates as needed: At the time of appointment Broker Kick-Off meetings Broker e-blasts and communications
How to AVOID a Complaint Always remain professional Always remain ethical Always act in the best interest of the prospective member/member Always discuss benefit information when it is permissible Always follow Health First policies and procedures as defined in your contract In Addition, for Medicare Line of Business: Always use CMS-approved materials Always follow Medicare Guidelines
Formal Outcome of Complaint The Manager of Broker Services will email the broker detailing the final outcome. The email will include: Recap of the conversation with the broker Final outcome on how Health First is handling the complaint Options on how the broker may challenge or appeal the complaint Contact information on how to reach the Manager of Broker Services
If you have any questions about the Broker Services Partner Integrity Program, please contact: Broker Services at HFBroker@HF.org Manager of Broker Services at Joyann.Moore@HF.org