Brucellosis
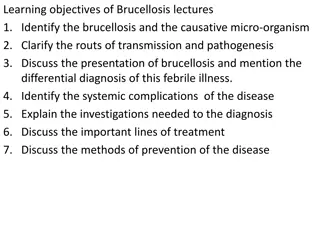
Brucellosis, also known as undulant fever or Malta fever, is a zoonotic infection transmitted to humans from infected animals through consumption of unpasteurized dairy products or contact with infected animal tissues or fluids. It is endemic in various regions worldwide, with increasing cases due to factors like international travel and trade. The disease is linked to occupational exposure in individuals such as shepherds, abattoir workers, and veterinarians. Various species of the Brucella bacteria are responsible for causing brucellosis, each associated with different host animals. Laboratory identification involves specific characteristics and growth requirements, with Castaneda's medium being a key tool for detection.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
BRUCELLOSIS DR.SREERAJ.H
Undulant fever Mediterranean fever Malta fever zoonotic infection transmitted to humans from infected animals (cattle, sheep, goats, camels, pigs) by ingestion of food products -unpasteurized dairy products or by contact with tissue or fluids MC zoonosis worldwide
EPIDEMIOLOGY ENDEMIC-countries of Mediterranean basin, Middle East, Central Asia, China, Indian subcontinent, sub-Saharan Africa, and parts of Mexico and Central and South America. 500,000 cases are reported annually Age groups -ALL Prevalence - has been increasing due to growing international tourism, trade, and migration Imported unpasteurized dairy products, such as fresh goat or sheep consumption of unpasteurized milk from domestic sources.
TRANSMISSION Consumption of infected, unpasteurized animal products (MC) Contact of skin or mucous membranes with infected animal tissue (such as placenta or miscarriage products) or infected animal fluids (such as blood, urine, or milk) Inhalation of infected aerosolized particles
occupational disease in shepherds, abattoir workers, veterinarians, dairy-industry professionals, and laboratory personnel Rare cases of human-to-human transmission blood transfusion tissue transplantation Breastfeeding sexual contact congenital transmission nosocomial infection
MICROBIOLOGY TAXONOMY 4 species B. melitensis - sheep and goats, camels (MC) VIRULENT B. suis - swine B. abortus - cattle B. canis - dogs
LABORATORY IDENTIFICATION nonmotile, facultative intracellular aerobic rods 0.5 to 0.7 micron in diameter and 0.6 to 1.5 micron in length gram-negative coccobacilli optimum growth temperature is 35 to 37 C Some biovars of B. abortus and B. suis require carbon dioxide
CASTANEDA S MEDIUM- biphasic medium requires 6 weeks of incubation yield is variable Automated blood culture systems are more effective Bactec and BacTAlert shorten the detection time considerably can be detected by the third day of incubation SENSITIVE to heat, ionizing radiation, disinfectants, and pasteurization
TYPE SURVIVAL AT/UPTO Milk 2 days at 8 degree Frozen Meat 3 weeks Goat Cheese 3 months Animal Secretions >40 days if soil is damp
CLINICAL FEATURES IP- 2 to 4 weeks Features Percentage of cases Signs and symptoms Fever (symptom) 76 Malaise 68 Night sweats 72 Arthralgia 80 Hepatomegaly 50 Splenomegaly 29 Laboratory findings Elevated alanine aminotransferase 33 Anemia 27 Leukopenia 9 Leukocytosis 8 Relative lymphocytosis 24 Thrombocytopenia 12 Pancytopenia <1
COMPLICATIONS can affect any organ system 1. Osteoarticular disease -MC form of focal brucellosis 70 percent of patients include peripheral arthritis, sacroiliitis, and spondylitis sacroiliac and spinal joints are the most commonly affected sites Peripheral arthritis and sacroiliitis occur in the context of acute disease Peripheral arthritis -knees, hips, and ankles
Spondylitis - serious complication more in older patients and patients with prolonged illness prior to treatment frequently associated with residual damage following treatment Osteomyelitis -lumbar vertebrae >> thoracic and cervical vertebrae Osteomyelitis may also accompany septic arthritis. Septic arthritis-knee, hip, sacroiliac, shoulder (mono or polyarthritis)
2. Genitourinary involvement 2ndMC form of focal brucellosis 10 percent of cases orchitis and/or epididymitis -MC In women- tubo-ovarian abscess has been described Additional manifestations -cystitis, interstitial nephritis, glomerulonephritis, and renal abscess In pregnant women -risk of spontaneous abortion, intrauterine fetal death, premature delivery, and intrauterine infection with possible fetal death
3.Neurologic-occurs in up to 10 percent of cases include meningitis (acute or chronic), encephalitis, brain abscess, myelitis, radiculitis, and/or neuritis 4.Cardiovascular -occurs in up to 3 percent of cases include endocarditis, myocarditis, pericarditis, endarteritis thrombophlebitis, and/or mycotic aneurysm of the aorta or ventricles. Endocarditis MC cardiovascular complication (1 to 2 percent of cases) Main cause of death
5.Pulmonary involvement - 2 percent of cases . Bronchitis, interstitial pneumonitis, lobar pneumonia, lung nodules, pleural effusion, hilar lymphadenopathy, empyema, or abscesses. 6.Intra-abdominal manifestations rare Hepatic or splenic abscess, cholecystitis, pancreatitis, ileitis, colitis, and peritonitis. 7.Ocular involvement rare Uveitis is MC. Keratoconjunctivitis, corneal ulcers, iridocyclitis, nummular keratitis, choroiditis, optic neuritis, papilledema, and endophthalmitis
8.Dermatologic manifestations - 10 percent macular, maculopapular, papulonodular, and erythema nodosum-like eruptions, ulcerations, petechiae, purpura, granulomatous vasculitis, and abscesses
CHRONIC BRUCELLOSIS patients with clinical manifestations for >1 year after the diagnosis of brucellosis Two categories Focal complication -such as spondylitis, osteomyelitis, tissue abscess, or uveitis and objective evidence of infection ( elevated antibody titers and/or recovery of Brucellae from blood or tissue culture) Persistent symptoms- in the absence of objective signs of infection (such as positive serology or cultures); symptoms may include malaise, psychiatric complaints (depression, anxiety, emotional lability), insomnia, sexual disturbances, tremor, or arthralgias
Relapse rate of relapse following treatment is 5 to 15 percent . Relapse usually occurs within the first six months following completion of treatment, but may occur up to 12 months later independent predictors included temperature 38.3 C, duration of symptoms <10 days prior to treatment, and positive blood cultures at baseline differentiation between relapse and reinfection can be difficult Causes -inadequate antibiotic regimen, inadequate duration of antibiotic therapy, lack of adherence, or localized foci of infection
LABORATORY FINDINGS elevated transaminases anemia, leukopenia or leukocytosis with relative lymphocytosis, and thrombocytopenia. synovial fluid Tc is usually 15,000 cells/microl (lymphocyte-predominant) organism can be grown in synovial fluid CSF-pleocytosis (10 to 200 white blood cells, predominantly mononuclear cells) mild to moderately elevated protein level
Low CSF glucose ADA - useful adjunctive test for diagnosis of CNS brucellosis . Elevated CSF ADA levels may also be observed in the setting of TB and other infections no clear threshold to distinguish neurobrucellosis from meningitis caused by other infectious agents antibody or agglutination testing of spinal fluid may be used to establish the diagnosis Genitourinary involvement- pyuria may be observed organism may be grown in urine culture
DIAGNOSIS suspected in patients with relevant signs and symptoms (fever, malaise, night sweats, and arthralgia) in the setting of relevant epidemiologic exposure. DEFINITIVE DIAGNOSIS Culture of the organism from blood, body fluids (urine, cerebrospinal fluid, synovial fluid, and pleural fluid), or tissue (such as bone marrow or liver biopsy) or fourfold or greater rise in Brucella antibody titer between acute and convalescent phase serum specimens obtained 2 weeks apart
PRESUMPTIVE DIAGNOSIS Brucella total antibody titer 1:160 by standard tube agglutination test (SAT) in serum specimen obtained after onset of symptoms or Detection of Brucella DNA in a clinical specimen by PCR
negative blood cultures and negative serologic studies, further investigation should be guided by the clinical presentation signs and symptoms of osteoarticular disease warrant synovial fluid analysis and radiographic imaging neurologic manifestatation- LP CSF Study. If unrevealing, bone marrow biopsy for culture and histopathology can be done If not diagnostic and there is evidence for liver involvement (based on liver function tests and/or radiographic imaging), proceed with liver biopsy
DIAGNOSTIC TESTS 1.CULTURE 2.SEROLOGICAL TESTS 3.MOLECULAR TESTS
1.Culture sensitivity of blood culture -15 to 70 percent . Automated blood culture systems are most effective biphasic (solid and liquid) blood culture (Castaneda technique) - used in some resource-limited settings . Blood cultures are often negative in the setting of chronic disease
Bone marrow culture is more sensitive than blood culture is considered the gold standard Bone marrow culture has a shorter time to detection than blood culture its sensitivity is not diminished by prior antibiotic use
2.Serological tests-must be interpreted in context of clinical presentation and epidemiologic data MC- SAT and enzyme-linked immunosorbent assays (ELISAs) Others-Rose Bengal agglutination test and the immunochromatographic lateral flow assay complicated and/or chronic infection -2-mercaptoethanol (2-ME) agglutination test, immunocapture agglutination (Brucellacapt) test, and indirect Coombs test
useful to use a combination of two serologic tests approach allows antibody detection at different stages of disease A/C- any of the assays may be positive C/c or complicated disease, SAT may be negative while 2-ME, Brucellacapt, Coombs, and ELISA IgG may be positive.
STANDARD AGGLUTINATION TEST(SAT) sensitivity and specificity of SAT are high 95 and 100 percent + SAT: titers consist of >1:160 outside endemic regions and >1:320 within endemic areas Evolution of titers ( a fourfold or greater rise in titer between acute and convalescent phase serum specimens obtained 2 weeks apart) may be used as a diagnostic tool not be used for diagnosis of B. canis infection B. canis serology should be requested specifically if brucellosis is suspected but the SAT is negative, or if there is clinical suspicion for B. canis infection
ELISA measure IgM, IgG, and IgA, and typically use whole cells or purified lipopolysaccharide (LPS), protein extracts, or other antigens sensitivity of ELISA- lower than SAT ELISA is preferred for diagnosis of neurobrucellosis used to distinguish from other infections that give false positive results
tests with short turnaround time that may be used as screening tools TESTS SENSITIVITY SPECIFICITY Rose Bengal agglutination test 87% 100% Immunochromatographic lateral flow assay 92% 97%
Disadvantages 1.Cross-reactivity -Francisella tularensis, Yersinia enterocolitica, Escherichia coli, Salmonella urbana, Vibrio cholerae 2.False-negative results - common early in the course of infection, in the setting of immunosuppression, and in presence of incomplete or blocking antibodies 3."prozone" phenomenon (eg, inhibition of agglutination at low dilutions due to an excess of antibodies or to nonspecific serum factors) is also seen.
interpretation difficult in the setting of chronic infection, reinfection, relapse, and in endemic areas where a high proportion of the population has antibodies against brucellosis . Positive serologic test results can persist long after recovery in treated individuals so it is not always possible to distinguish serologically between active and past infection
3.Molecular tests development of molecular testing for diagnosis of brucellosis is promising but this is not yet a routine diagnostic tool . Brucella 16S rRNA gene sequences have been determined to be identical 16S rRNA gene sequencing is useful for genus identification, but cannot be used for species identification
OTHERS IMAGING-useful for evaluation of patients with signs and symptoms of brucellosis, but does not enable definitive diagnosis. For evaluation of spondylitis, MRI is the preferred imaging study Other modalities - plain radiography, computed tomography (CT), and bone scintigraphy Pons sign -a step-like erosion of the anterosuperior vertebral margin
For patients with brucellosis who present with fever of uncertain etiology and undergo CT scan, hepatosplenic disease with localized calcification may be observed.
In the setting of suspected endocarditis, echocardiography to be done . Histopathology Bone marrow biopsy and liver biopsy - noncaseating granulomas (consisting of epithelioid cells, polymorphonuclear leukocytes, lymphocytes, and some giant cells) in the setting of infection due to B. melitensis and B. abortus B. melitensis infection, granuloma are very small. B. suis infection is often accompanied by chronic abscess formation
D/DS 1.Malaria 2.HIV 3.TB 4.Visceral leishmaniasis 5.Malignancy 6.Q fever 7.Enteric fever
In patients with osteoarticular manifestations 1.Spondyloarthritis 2.Reactive arthritis 3.Septic arthritis 4.Lymes disease 5.Viral infections 6.SLE 7.RA
TREATMENT General approach Goal of brucellosis therapy is to control the illness and prevent complications, relapses, and sequelae Use of antibiotics with activity in acidic intracellular environments (doxycycline and rifampin), use of combination therapy (given high relapse rates with monotherapy), and prolonged duration of treatment
preferred regimen is doxycycline combined with an aminoglycoside Less treatment failure and relapse many favor doxycycline-rifampin :- it is more convenient than parenteral therapy may be better tolerated than aminoglycosides (which are associated with nephrotoxicity and ototoxicity) is less costly
Alternative agents Alternative agents include fluoroquinolones and TMP-SMX, used in combination regimens may be used as alternative second or third agents in combination regimens containing doxycycline or rifampin . not appropriate first-line agents decreased activity in acidic environments, as well as cost may be beneficial in the setting of drug resistance, antimicrobial toxicity, and some cases of relapse ciprofloxacin 500 mg BD for 6 weeks or ofloxacin 200 to 400 mg orally BD for 6 weeks TMP-SMX one double-strength tablet (160 mg TMP and 800 mg SMX) orally twice daily for six weeks
PREGNANCY <36 weeks gestation, rifampin plus TMP-SMX, both for six weeks . 36 weeks gestation, rifampin monotherapy until delivery given risk of neonatal kernicterus with the use of TMP-SMX in the last month of pregnancy. After delivery, we continue combination therapy as in nonpregnant adults; the total duration of treatment is 6 weeks
TREATMENT OF SPECIFIC COMPLICATIONS Spondylitis optimal approach to treatment of Brucella spondylitis is uncertain
36 weeks gestation, ceftriaxone and rifampin until delivery, given risk of neonatal kernicterus with the use of TMP-SMX in the last month of pregnancy. After delivery, continue combination therapy as in nonpregnant adults; the total duration of treatment is 12 weeks duration of therapy is as important as the choice of antimicrobial agents treatment for Brucella spondylitis for adults should consist of antibiotic therapy for 12 weeks.
with persistent symptoms and/or radiographic findings, the duration of treatment should be extended beyond 12 weeks, based on individual patient circumstances Surgery indications spinal instability persistence or progression of neurologic deficit vertebral collapse localized abscess (epidural or paravertebral)