Care Closer to Home Model Benefits and Reforms
Explore the Care Closer to Home (CCtH) model focusing on preventing hospital admissions with Integrated Neighbourhood Teams. Discover the idea behind it, patient benefits, and necessary reforms to meet the growing demand for healthcare services among the elderly population.
Uploaded on | 0 Views
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Care Closer to Home(CCtH) Model -Preventing hospital admission with Integrated Neighbourhood Teams (INT) Dr Keith Remedios GP/ Joint Locality lead
Where did the idea come from ? Fuller stock take report (2022) Reorientate health and social care to a local population health approach Dazi Review (2024)- It emphasizes the need to shift resources towards primary and community care, as these settings offer a superior return on investment compared to acute hospital service
Why have Care closer to home? Benefits for patients Respecting patient's wishes to be managed at home Decrease risk of deconditioning and loss of independence Hospitals are associate with increased risk of Hospital acquired infection and delirium Benefits to Local healthcare system Doing the right thing for our patients increasing staff morale Reducing pressure on emergency services to improve their capacity Redirect money to help community care
Initial focus on Frailty NNT =5 Therefore would need to review 130 patients per month
Why Care closer to home model? Over 65 years > 4000 PPPY compared to 250 PPPY for the healthy population. There will be significant growth in over 65 year olds (44% increase between 2018 and 2043) and very significant growth in over 85 year olds (73% increase between 2018 and 2043). There is no alternative plan or strategy to cope with this increase in demand. No new hospitals
BUT no money for the NHS without Reform! Sir Keir Stammer
What reforms ? Analogue to digital Reactive to proactive to preventative care Hospital to community care No Wrong Door approach Patient Focused
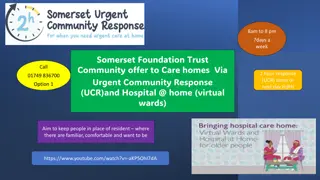
Care Closer to Home Model: 5 Steps 1 Keeping well Core general practice, public health campaigns, Voluntary Community Faith and Social Enterprise (VCFSE) sector, and local council initiatives for example, loneliness cafes and befriending services It also includes Strength and Balance classes as a falls prevention intervention 2 Care Maintenance Supporting patients to maintain or improve their current health status Delivered through core and enhanced general practice and integrated community specialist services Particular focus on chronic disease management Remote monitoring for patient s with Long Term Conditions 3 Proactive Care The main intervention for this component of the model is Integrated Neighbourhood Teams: Multi-disciplinary teams will deliver proactive and holistic case-management to maximise health, deliver the evidence-based interventions shown to reduce non- elective admissions and improve quality of life with a focus on primary, secondary and tertiary prevention Community nursing and therapy teams are also integral to this component of the model 4 Urgent Care in the Community This includes providing a single, short intervention for an acute presentation which could be managed at a Minor Injuries Unit (MIU), Urgent Treatment Centre (UTC) or Same Day Emergency Care (SDEC) It also incorporates providing an integrated urgent care response in the community, avoiding the need for hospital attendance Hospital at Home services which provide hospital-level care to patients in their usual place of residence (including care homes) 5 Acute hospital admission The CCH model of care aims to prevent acute hospital admission where possible, however some patients will require acute level hospital inpatient care to support their needs
Integrated Neighbourhood Teams (INT) Integrated Neighbourhood Teams bring together professionals from different organisations across health and care services. The aim is to deliver more joined up, preventative care at a neighbourhood level with the aim of keeping people safe and well in their own homes
Case study without proactive care John aged 76 Has dementia, heart failure, cared for by his wife Holly. Holly Main carer for John - is 73 years old with severe Chronic obstructive pulmonary disease (COPD) Scenario Holly call ambulance via 999 with worsening shortness of breath. John is deemed to not be safe at home so both are admitted to hospital. Holly sadly dies 10 day later due to severe pneumonia. John is place in an interim care bed before moving to a nursing home to meet his needs. Unfortunately, following his hospital admission his care needs increased.
Same case with proactive care John is identified as being at high risk of hospital admission on a population search. A holistic assessment is conducted for both John and Holly (with their daughter (Julie) present!) respecting their wishes to remain at home for the best community care via an Advance Care Plan. They are discussed at the Neighbourhood MDT. Holly is given a recue pack to start at home if she becomes unwell. The family has expressed that if Holly was to die, he would like to go to his chosen care home. Coordination number is given to the family for future reference. Scenario Holly becomes short of breath and starts the rescue pack of medication Daughter called the coordination number, who set up a 2 hour responses and start Holly on IV antibiotics, interim carers are put in place for John Holly recovers and goes back to looking after John.
Other Integrated working Diabetes Heart failure Respiratory Childhood obesity
We MUST focus on prevention. Challenging govt policy does not support this No sugar tax, local authority building Macdonalds near schools, advertising around sports events, screen time
Active Practice Discourage sedentary behaviour in Patient/ Staff Encourage activity in patients and staff
Living Well Pillars Healthy Eating Ultra processed food increase risk of diabetes/ heart disease linked to early death Stress- causes increase adrenaline / cortisol level causing high blood pressure, muscular problems Purpose -More than half of young adults (58%) reported that they lacked meaning or purpose in their lives in the previous month and half of young adults reported that their mental health was negatively influenced by not knowing what to do with my life. Exercise sedentary behaviour 4th biggest cause of mortality Sleep- Restorative process - lowers risk of long term conditions/less likelihood of getting sick
Summary Care closer to home Integrated neighbour Teams Focus on frailty Prevention is key!