Caries Activity Tests Overview
Dental caries, a multifactorial infectious disease, leads to cavity formation. Caries activity tests help assess the speed of lesion progression, evaluate risk, and determine personalized preventive measures. They play a crucial role in maintaining oral health and guiding treatment decisions.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
CARIES ACTIVITY TESTS 2
Lesson plan Topic: Caries Activity tests Date: 20-04-13 Class: 4th B D S Duration: 1 hour Setting: Classroom At the end of the session, the learners should know need of caries activity tests, Characteristics of ideal test and Various types of caries activity tests
Contents Introduction Caries activity Need for caries activity test Ideal caries activity test Caries activity tests Summary 4
Introduction Dental caries is an infectious microbial disease that begins as demineralization of inorganic portion of the tooth followed by destruction of organic portion leading to cavity formation. Dental caries is a multifactorial disease. 5
Caries risk assessment Caries risk assessment determines the probability of caries incidence, i.e., the number of new cavities or incipient lesions over a given period of time. 7
Caries susceptibility Inherent tendency of the host and the target tissue, the tooth, to be afflicted by the caries process. This is the susceptibility (or resistance) of a tooth to a caries producing environment. 8
Caries activity Increment of active lesions (new or recurrent) over a stated period of time. Caries activity is a measure of the speed of progression of a carious lesion. 9
Caries activity tests Measure environmental challenge favours the probability of occurrence of carious lesions. the degree to which the local Degree of caries activity Caries activity tests 10
Caries activity test helps to: 1. Identify high risk groups and individuals 2. Determine the need for personalized preventive measures and motivate the individual 3. Ensure a low level of caries activity before starting any extensive restorative procedure. 11
4. Monitor effectiveness of oral health education programs by establishing an initial baseline level of cariogenic pathogens as a basis for future evaluation. 5. Serve as an index of success of therapeutic measures: reduction in the number of Strep mutans and Lactobacilli as a part of counselling to decrease sucrose intake. 12
Ideal requisites Ideal requisites Sound theoretical basis Maximum correlation with clinical status Accurate duplication of results Simple Inexpensive Less time consuming 13
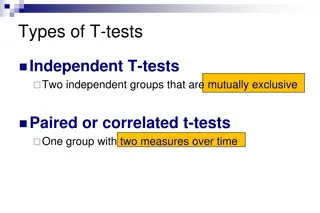
Caries activity tests Caries activity tests 1. Lactobacilli colony count test 2. Colorimetric Snyder test 3. Salivary reductase test 4. Salivary buffer capacity test 5. Fosdick calcium dissolution test 6. Streptococcus mutans screening tests 14
Streptococcus mutans screening tests i. ii. iii. Dip slide method iv. Adherence test v. Replicate test Plaque / tooth pick method Saliva / tongue blade method 15
1. Lactobacillus Colony Count Test (Hadley 1933) Principle: Estimates the number of acidogenic and aciduric bacteria in the patient s saliva by counting the number of colonies appearing on tomato peptone agar plates (pH 5.0) after inoculation with a sample of saliva. 16
Procedure: Saliva is collected by asking the subject to chew paraffin before breakfast and then collecting saliva in a bottle. The specimen is shaken to mix it. The dilution of 1:10 and 1:100 are prepared by mixing with sterile salt solution. 17
Then 0.4ml of 1:100 diluted saliva is spread on the surface of agar plate with a bent glass rod. The plates are labelled and incubated at 37 C for 3-4 days. Then numbers of colonies are counted using Quebec counter. 18
It takes only few minutes to do the test, but the results are not available for several days. Counting the number colonies is a very tedious process.
Lactobacillus test Number of organisms per cubic cm Symbolic designation Degree of caries activity suggested 0 1000 + Little or none 1000 5000 + Slight 5000 10,000 ++ Moderate More than 10,000 +++ Marked 20
Limitations Not simple Needs professional training Requires complex equipment and hence costly Lactobacillus count varies in the same individual. Does not completely exclude growth of other relatively aciduric organisms. 21
Dentocult-LB Dip-slide culture method Collecting and pouring stimulated saliva over a Dentocult dip-slide. The slide is covered on both sides with modified Rogosa medium for culture of lactobacilli. Incubated at 37 degrees for 4 days. Shows lactobacilli as white to transparent colonies on the agar surface.
Lactobacilli per ml. of saliva Model chart for comparison of colony density. Lactobacilli per ml saliva high more than 100.000 (105) risk value low less than 10.000 (104)
2. Snyder Test (1951) Principle: Measures the rapidity of acid formation when sample of stimulated saliva is inoculated into glucose agar adjusted to pH 4.7 to 5 and with bromocresol green as colour indicator. 24
Procedure Saliva is collected before breakfast by having the subject chew paraffin. A tube of Snyder glucose agar is melted and then cooled to 50 c. Then 0.2ml of saliva is pipetted into the tube of agar and immediately mixed by rotating the tube. 25
The agar is allowed to solidify in the tube and is incubated at 37 C. The colour change of the indicator is observed for 24, 48 and 72 hours of incubation. 26
Snyder test Time (hours) 24 48 72 Colour Yellow Yellow Yellow Caries activity Colour Marked Definite Limited Green Green Green Caries activity Continue test Continue test Inactive 28
Advantages Limitations 1. Time more. (24 48 hours) consumed is 1. Simple 2. Requires only simple equipment. training is needed and the cost is moderate 3. Correlation with clinical trials. Some 2. Sometimes changes are not so clear. colour 29
Albans test It is a simplified substitute for the Snyder test. The depth of colour change in the medium. Level of colour change Scoring No change Beginning of colour change (from top) + Onehalf colour change (from top) + + Three forth colour change (from top) + + + Total colour change to yellow + + + + 30
3. Salivary Reductase Test (Susceptibility test) Principle: Measures the rate at which an indicatordiazo resorcinol, changes from blue to red to colourless on reduction by mixed salivary flora. This test measures the activity of enzymereductase - secreted by salivary bacteria. 31
Saliva is collected before breakfast having subject chew paraffin and expectorating directly into the collection tube. When the saliva reaches the calibration mark (5ml) the reagent cap is replaced. 32
The sample is mixed with a fixed amount of diazo resorcinol, the reagent upon which the reductase enzyme is to react. The change in colour after 30 seconds and after 15 minutes is taken as a measure of caries activity. 33
30s. Diazo Resorcinol dye 15 min. Stimulated saliva
Salivary Reductase test Colour Time Scor e 1 Caries Activity Blue 15 minutes Non conducive Orchid 15 minutes 2 Slightly conducive Red 15 minutes 3 Moderately conducive Highly conducive Red Immediately 4 Pink or white Immediately 5 Extremely conducive 35
Advantages Good correlation with clinical experience. Measure of oral hygiene status of an individual. Caries-free adults exhibit low or negative scores on reductase test. 36
4. Salivary Buffer Capacity test Principle: Measures the number of ml of acid required to lower the pH of the saliva through an arbitrary pH interval, such as from pH 7 to 6 or amount of acid or base necessary to bring colour indicators to their end point. 37
Procedure Ten ml of stimulated saliva is collected at least one hour after eating; 5 ml of this are measured into a beaker. After correcting the pH meter to room temperature, the pH of saliva is adjusted to 7 by addition of acid or base. 38
Lactic acid is then added to the sample until a pH of 6 is reached. The number of ml of lactic acid needed to reduce pH from 7 to 6 is a measure of buffer capacity. This number can be converted to milliequivalents (mEq) per litre. 39
This test gives inverse relationship between buffering capacity of saliva and caries activity. The saliva of individuals whose mouths contain a considerable number of carious lesions frequently has a lower acid-buffering capacity than the saliva of those who are relatively caries-free. 40
Interpretation The yellow color indicates a final pH of 4 or less, meaning that the saliva was unable to raise the pH. There is an inverse relationship between buffering capacity of saliva and caries activity. Caries activity Buffering capacity of saliva
Advantages Disadvantages Simple to carry out Does not correlate adequately with caries activity. 42
5. Fosdick Calcium Dissolution Test Principle: Measures milligrams of powdered enamel dissolved in 4 hours by the acid produced by mixing patient s saliva with glucose and powdered enamel. 43
Procedure 25 ml of gum stimulated saliva is collected and this is analysed for calcium content. The rest is placed in a sterile tube with about 0.1g of powdered enamel. The tube is sealed and shaken for 4 hours at body temperature. 44
Then again it is analysed for calcium content. The amount of enamel dissolution increases as the activity increases. 45
Limitations Not simple Costly equipment High cost Require trained personnel. 46
6. MUTANS STREPTOCOCCI SCREENING TESTS 47
Streptococcus mutans screening tests i. ii. iii. Dip slide method iv. Adherence test v. Replicate test Plaque / tooth pick method Saliva / tongue blade method 48
a. Plaque toothpick method: Plaque samples are collected from the gingival third of buccal tooth surfaces (one from each quadrant)and placed in Ringer's solution. Then the plaque suspension is streaked across a mitis - salivarius agar plate. 49
Incubated at 37C for 72 hours, the cultures are examined under a low-power microscope and the total colonies in 10 fields are recorded. This test is an attempt to semiquantitatively screen the dental plaque for a specific group of caries inducing streptococci, mutans. Streptococcus 50