Chronic Migraine in Primary Care: Management and Treatment
Chronic migraines in primary care, from prevalence to diagnostic criteria and management options, including a holistic approach and differentiating between acute and preventative treatments. Explore primary and secondary headache types, including common causes like medication overuse. Get insights into recognizing dangerous secondary headache causes such as brain tumors and subarachnoid hemorrhage.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Chronic Migraine in Primary Care Nelya Drofyak Curry MPAS PA-C
Outline Approach to headache Migraine Prevalence Connect Migraine pathophysiology to phenotypic symptoms ICHD-3 Diagnostic criteria Evaluation of the patient Management of Chronic Migraines Treatment expectations Holistic approach Acute vs Preventative options Special cercumstatnces
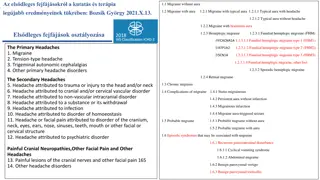
General Approach to Headache Primary Cluster headache Tension headache Migraine headache Secondary Symptom of headache due to secondary process Fewer than 5%
Primary Headache Overview Cluster headache Rare, 9M>1F Recurring 30min to 2 hrs Trigeminal autonomic cephalgia Unilateral pain c autonomic sx Tears, congestion, red eye, Horner syndrome Tension headache common Holocephalic squeezing +/- Photophonia +/- Sonophobia 1 to 2 hrs Chronic RO cancer & gammopathy
Secondary Headache First determine if headache is dangerous Brain tumor present c behavioral change, ataxia, cognitive dysfunction, seizures Subarachnoid Hemorrhage [SAH] >40 yo c worse HA of your life Meningitis Fever, chills, neck pain c movement Pseudotumor cerebri HA worse c changes in posture, mild pain c eye movement, vision sx Arterial dissection Acute Ha, neck pain, stroke sx, recent trauma/sports/cough
Secondary Headache Common disabling and disruptive headaches Headache due to substance withdrawal (alcohol, caffeine, Estrogen, Opioids, nitric oxide, Carbon monoxide, Histamine) Headache due to psychiatric disorder (somatization, GAD, MDD, PTSD) Medication overuse headache (MOH) Migraine is the most common primary headache associated c MOH 65% MOH is the most common cause of sx to suggest hronic migraine
Medication Overuse Headache Pts c pre-existing primary headache develop new headaches or significantly worsening headache due to >3 mo overuse of medications Headache occurring > 15 days per month Patient overuse: 10 days per mo for >3 mo of ergotamine, triptans, or opioids or combination analgesics 15 days per mo for >3 mo of simple analgesics (acetaminophen, aspirin, or NSAID) TX: Improves after the medication overuse is discontinued Supplement c Naproxen 500mg BID & Occipital Nerve Block
Lets talk about Migraines M affects 1 in 7 people in the world & 40 million people in USA M is ranked 3rdhighest cause of disability worldwide in <50yo by Global Burden of Disease Study 2010 and 2015 due to high prevalence and socio-economic and personal impacts M prevalence peaks at age 30 to 39 yrs; 24% females & 7% males Chronic M affects 2% of the world population Chronic M is the most disabling subset of migraine; 90% c sever impairment
What is a Migraine? Neurologic disorder (ie. brain dysfunction) due to a genetic predisposition combined with environmental factors that result in phenotypic symptoms with four phases: Premonitory symptoms, Aura, Headache, Postdrome
Pathogenesis Overview of Migraine Cortical spreading depression Trigeminovascular system Sensitization Role of Serotonin Role of CGRP Since 2014 functional imaging studies lead to novel insights Primary neuronal dysfunction leads to a sequence of changes intracranially and extracranially
Pathogenesis to Symptoms to Diagnosis Lets connect the dots Most patients are not fully aware of all their migraine symptoms Most patients with M experience headache during the aura phase
Prodrome / Premonitory Phase Early cortical spreading involvement of subcortical brain areas Symptoms: Neck discomfort 75% Fatigue Cognitive sx; brain fog Mood change; irritability Photophobia Yawning/sleepiness Polyuria/polydipsia Hunger / food cravings Occurs up to 48 hours before M headache Occurs in 77% of pts c M Reliable perdition of impending M *Best time to use PRN medication
Cortical Spreading Depression Self-propagating electrical wave of neuronal and glial depolarization Activates Trigeminovascular system Pain fibers release calcitonin gene- related peptide (CGRP) Alter blood-brain barrier permeability
Aura Phase Symptoms: Visual Auditory Sensory Verbal Motor Cortical spreading depolarization wave Develops over several minutes; typically occur 20 min to 1 hr before headache Complete Reversibility Triggers positive and negative neurological symptoms in 20-25% of M pts
Role of CGRP Mediate trigeminovascular pain transmission from intracranial vessels to the central nervous system and vasodilatory component of neurogenic inflammation Very effective target for treatment
Headache Phase Common Symptoms: Throbbing or pulsing quality Nausea +/- vomiting Photophobia +/- Phonophobia Exacerbation c routine activity Vertigo Allodynia Cutaneous allodynia particularly the scalp Due to Trigeminal vascular system and neuromediators Moderate to Severe head pain 4 to 72 hours duration (without treatment) *sleep counts towards time duration
Role of Serotonin Important for acute Tx Unclear in generation No Risk of Serotonin Syndrome c Triptans + SSRI/SNRI Unnecessary FDA warning per American Headache Society Evans RW, Tepper SJ, Shapiro RE, Sun-Edelstein C, Tietjen GE. The FDA alert on serotonin syndrome with use of triptans combined with selective serotonin reuptake inhibitors or selective serotonin-norepinephrine reuptake inhibitors: American Headache Society position paper. Headache. 2010;50(6):1089-1099. doi:10.1111/j.1526-4610.2010.01691.x
Postdrome Phase Symptoms: Neuromodulator inflammation subsiding? Motion-provoked residual head pain Tiredness Weariness Concentration impairment Mild elation or euphoria Once spontaneous throbbing of the headache resolves Lasting a few hours to 1 day
Sensitization Chronic Migraines Mediated by neuromodulators Process when neurons become increasingly responsive to nociceptive and nonnociceptive stimulation Response thresholds decrease Response magnitude increase Receptive fields expand Spontaneous neuronal activity develops
All Migraine Types per ICHD-3 M without aura Complication of M Status Migrainosus Persistent aura without infarction M infarction M aura-triggered seizure Episodic syndromes that may be associated c M Recurrent gastrointestinal disturbance Cyclical Vomiting Syndrome Abdominal M Benign Paroxysmal Vertigo Benign Paroxysmal Torticollis M with Aura M with typical aura Typical aura c HA Typical aura co HA M with brainstem aura Hemiplegic M Familial Hemiplegic Migraine Sporadic Hemiplegic M Retinal M Chronic M
Diagnostic Criteria Migraine co Aura (ICHD-3) Long-duration headache 4-72 hrs c 2 of 4 symptoms: At least 5 attacks At least 1 Associated Sx Nausea / gut dysfunction Photophobia Phonophobia Odophobia Unilateral frontotempora *bilateral in kids Pulsating quality Moderate to sever intensity Aggravated by activity
Screening tool that is >80% accurate Two affirmative answers for: stomach issues with headache light sensitivity during headache limited daily activities during headache
Chronic Migraine Diagnostic Criteria (ICHD 3) 15 days/month for > 3 months with migraine headache features for at least 8 days/month not better accounted for by another ICHD-3 diagnosis
Evaluation of Migraine Headache History Timing, untreated duration, onset, progression, premonitory symptoms, associated symptoms, +/- aura, character of pain, triggers, previous treatments, family history of migraine ( 66% of pts) Patient needs to keep a headache diary: record information on pain and associated symptoms day-by-day for at least one month
Evaluation of Migraine Physical Exam Detailed Neurologic exam CNII-XII Eval head for tenderness: nodular superficial temporal arteries, occipital nerve root tenderness Fundoscopic exam; consider refer to ophthalmologist Temporomandibular junction may be pain trigger *muscles of mastication innervated by trigeminal nerve Shoulder / neck tightness *activation of upper C2-4 roots
Evaluation of Migraine Diagnostic Testing Neuroimaging is not necessary in most patients Consider neuroimaging (head CT) in non-acute headache if: Patients c atypical headache features Recent significant change in pattern, frequent, or severity of headache (Rule out and treat MOH) Headache not responding to treatment New-onset headache after age of 50 years
Aligning therapeutic patient-provider goals Our job is to advise on best practices using medical based evidence Patient gets to decide what is ultimately best for them Compassionate approach Offer accommodations for work, school, ect. not only for chronic migraines, but also possible side effects of medications
Treatment Expectations; Benefits > Risks I help patients increase function despite having chronic migraines while focusing on reducing number of migraine days and/ or severity of symptoms Not realistic to eradicate all migraines, yet Multifactorial approach to optimize treatment response
Management of Chronic Migraine Patient education Advise self care Lifestyle Meditation, yoga, mindfulness, acupuncture, consistent sleep, routine exercise, health eating habits, caffeine <200mg/day Avoid triggers Cognitive Behavioral Therapy Physical therapy Supplements Acupuncture (10 sessions in 8wks) Neuromodulation Devices Medications
Common Triggers for Acute Migraine Attack Emotional stress (80%) Hormones in females (65%) Not eating (57%) Weather (53%) Sleep disturbances (50%) Odors (44%) Neck pain (38%) Lights (38%) Alcohol (38%) Smoke (36%) Sleeping late (32%) Heat (30%) Food (27%) Exercise (22%) Sexual activity (5%) Kelman L. The triggers or precipitants of the acute migraine attack. Cephalalgia. 2007;27(5):394-402. doi:10.1111/j.1468-2982.2007.01303.x
Diet Beyond Avoiding Triggers Higher levels of omega-3 fatty acid and lower omega-6 fatty acid decreased incidence (4 hrs per day) and severity of migraines Ketogenic Diet after 3 mo improves sleep in M patients, reduced M frequency, and lowers M intensity Ramsden C E, Zamora D, Faurot K R, MacIntosh B, Horowitz M, Keyes G S et al. Dietary alteration of n-3 and n-6 fatty acids for headache reduction in adults with migraine: randomized controlled trial BMJ 2021; 374 :n1448 doi:10.1136/bmj.n1448 Merlino G, Tereshko Y, Pez S, et al. Sleep of migraine patients is ameliorated by ketogenic diet, independently of pain control. Sleep Med. 2023;107:196-201. doi:10.1016/j.sleep.2023.05.006
Occipital Nerve Blocks q 3 months 80 mg depomedrone (40 mg/mL) and 2 mL of 2% lignocaine; total 4 mL per injection into each GON SE: local alopecia, transient dizziness, acute worsening headache
PRN 1st-tier (Analgesics) NSAIDs Naproxen APAP APAP-Aspirin-Caffeine Educate: limit use to 15 times / mo AVOID Opioids, Barbiturates, and Benzodiazepines unless Pregnant (Fioricet) Document if pt failed this
PRN 2nd-tier (Triptans) Treat early; at first sign of migraine Maximize initial dose May repeat after two hours if response to initial dose is suboptimal Pts who do not respond well to one triptan may respond to another Combine c Naproxen or Meloxicam to reduce migraine recurrence Common side effects: drowsy, nausea Avoid use within 24 hrs of ergotamine preparation CI: Early Pregnancy, ischemic heart dz, Stroke/TIA, hemiplegic or basilar M, PVD, uncontrolled HTN
Sumatriptan PO 100mg Max 200mg/day PO, intranasal (>5yo), SubQ Rizatriptan *reduce dose c Propranolol PO 10 mg Max 30mg/day PO, ODT, film most efficacious; better tolerated Zolmitriptan PO, ODT, Intranasal, skin patch Eletriptan PO most efficacious metabolized by CYP3A4 Almotriptan PO; Best tolerated metabolized by CYP3A4 Longer Duration (menstrual M) Naratriptan 2.5mg Max 5mg/day [1/2 life ~8 hrs] Least effective Frovatriptan 2.5mg Max 5mg/day [1/2 life ~26hrs] Kids 6-11yo <40kg smallest dose Kids >11yo > 40kg tolerate adult dose Key PO: tablet ODT: oral disintegrating tablet
Sinclair AJ, Sturrock A, Davies B, Matharu M. Headache management: pharmacological approaches. Pract Neurol. 2015 Dec;15(6):411-23. doi: 10.1136/practneurol-2015-001167. Epub 2015 Jul 3. PMID: 26141299; PMCID: PMC4680181.
Newer Acute PRN Treatment Gepants CGRP antagonist Rimegepant (Nurtec) ODT Atogepant (Qulipta) PO Ubrogepant (Ubrelvy) PO Zavegepant (Zavzpret) nasal Ditans 5-HT1FAgonists Lasmiditan (Reyvow) Avoid driving for 8 hr; Schedule V SE: Dizziness Must consider for your Pts c hemiplegic migraines*, basilar migraines, cardiovascular dz, cerebrovascular dz SE: Nausea
In-Depth systematic review & meta-analysis Among 64 randomized clinical trials c a total of 46,442 pts comparing Nurtec, Ubrelvy, Reyvow to Triptans *Zavzpret + Qulipta excluded Triptan > Gepants & Ditans for pain freedom at 2 hrs Gepants = Ditans; not statistically significant difference in outcome Rayvow had highest risk of SE Yang C, Liang C, Chang C, et al. Comparison of New Pharmacologic Agents With Triptans for Treatment of Migraine: A Systematic Review and Meta-analysis. JAMA Netw Open. 2021;4(10):e2128544. doi:10.1001/jamanetworkopen.2021.28544
+ Antiemetics Include antiemetic, even if no nausea, to counter gastric stasis and facilitate PRN medication absorption / pain relief Meclizine (25 mg PO) Diphenhydramine (25 to 50 mg PO) Promethazine (12.5 to 25 mg PO, rectum, IM) Ondansetron (4 to 8 mg PO, ODT) Metoclopramide (10 mg IM, PO) *Avoid in Pregnancy Prochlorperazine (10 mg IM, PO)
My pitch for preventative medications Up to 50% of pts treated c one of these medications will have at least 50% reduction in frequency or severity after 12 weeks; if given adequate doses CGRP targeted therapies, Occipital Nerve Blocks, and Botox generally take at least 2-3 rounds to know if they work If this medication does not help you, stop it and try something else 80% of pts DC medication due to SE at <1 year and 60% at <6 mo. Side effects are common, its okay to discontinue
Preventative 1st line Propranolol 40 BID tapper to SE: bradycardia; CI: asthma Amitriptyline 10-30mg qHS SE: dry mouth, arrythmia Topiramate 25-200mg/d SE: groggy, weight loss *interferes c oral contraception efficacy CGRP antagonist (Erenumab, Fremanezumab, Galcanezumab, Eptinezumab, Atogepant) FDA approved for >18 yr; real world data established safety for > 5yr
CGRP-targeted therapies Acute + Prevention No evidence that one antibody is superior to the others in terms of effectiveness, both in chronic and episodic patients Gepants block CGRP receptor Ubrogepant (Ubrelvy) PO Rimegepant (Nurtec) ODT Atogepant (Qulipta) PO lower dose c CYP3A4 inhibitors (Cannabis)
CGRP-targeted therapies Prevention mAbs block CGRP receptors Erenumab (Aimovig) SubQ q 1 mo Bind to CGRP peptide Galcanezumab (Emgality) subQ q mo Fremanezumab (Ajovy) subQ q1 mo or q3 mo Eptinezumab (Vyepti) IV q 3 mo >80% pts had migraine decrease by 50% on day after infusion
Preventative 2nd line Magnesium 400-600mg daily Riboflavin (Vit B2) 400 mg daily CoQ10 100 mg TID Acupuncture Candesartan BB (Atenolol, Nadolol, Metoprolol) Gabapentin Venlafaxine Valproic acid *avoid if childbearing potential Tricyclic (Nortriptyline, Protriptyline) Occipital Nerve Block Botox ($) M 50% in <6mo & 70% in <1 yr After failing > 3 other preventatives
Preventative 3rd line Feverfiew 50 to 300 mg daily *CI: c anticoagulant Verapamil Tizanidine Memantine Pregabalin Cyproheptadine Zonisamide
Neuromodulation for Acute + Prevention Cefaly Relivion MG Stimulates occipital and trigeminal nerve Rx for >18 yr GammaCore vagal stimulator; efficacy not established Rx for >12 yr OTC supraorbital/supratrochlear nerve stimulator; effective Safe in pregnancy Nerivio Remote neuromodulation arm band Rx for >12 yr
Use of Estrogen with Migraine with Aura Use of estrogen-containing contraception increase relative risk an estimated 2- to 16- fold Migraine c aura have an independent risk for ischemic strokes 2-2.5 times higher compared to Migraine co aura Higher risk with female gender, age < 45yo, smoking Gillum LA, Mamidipudi SK, Johnston SC. Ischemic stroke risk with oral contraceptives: A meta-analysis. JAMA. 2000;284(1):72-78. doi:10.1001/jama.284.1.72
Acute Treatment in Pregnant People *People who get M co aura may experience M aura for the first time APAP; APPA + codeine If refractory, then 2nd tier: Butalbital until 2nd trimester: NSAIDs (avoid in 3rd trimester) Triptans Opioids Consider preventative treatments sooner AVOID Ergotamine and Isometheptene
Prevention in Pregnant People Magnesium Riboflavin Acupuncture Cefaly device Occipital Nerve Blocks Amitriptyline 10-15mg Calcium Channel blockers Bata Blockers Topiramate Offer if PRN not effective; debilitating M; >1 M / week Chronic M reduce by 50-80% during pregnancy Avoid Depakote Valproic Acid