Chronic Periodontitis: Causes, Symptoms & Management
Explore the ins and outs of chronic periodontitis, including its definition, risk factors, clinical features, and symptoms. Learn about disease progression, diagnosis, and classification to better understand this prevalent form of periodontal disease.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
SEMINAR ON CHRONIC PERIODONTITIS Presented by: Pooja Chamle BDS 4th Year ( Roll no. 15)
Learning Objectives What is Chronic Periodontitis? Clinical features and risk factors of it? Signs and symptoms of it ? Disease progression and diagnosis
INTRODUCTION Chronic periodontitis, formerly known as Adult periodontitis or Chronic adult periodontitis , is the most prevalent form of periodontitis. It is generally considered to be a Slowly progressing disease Definition: Chronic periodontitis has been defined as an infections disease resulting in inflammation with in supporting tissues of the teeth, progressive attachments loss and bone loss.
Risk Factors for disease 1. Prior History of periodontitis 2. Local factors. 3. Systemic factors. 4. Environmental and behavioral factors. 5. Generic factors.
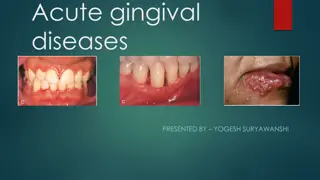
CLINICAL FEATURES: Supragingival and subgingival plaque accumulation (frequently associated with calculus) Gingival inflammation. Pocket formation. Loss of periodontal attachment. Occasional suppuration. Poor oral hygiene gingiva is typically may be slightly to moderately swollen.
Color- pale red to magenta. Consistency- Soft or Firm. Surface topography- loss of stippling. Blunted or rolled gingival margin. Flattened or cratered papillae. Tooth mobility. Furcation involvement. Spontaneous gingival bleeding. Pocket depths are variable and both suprabony and infrabony pockets can be found.
SYMPTOMS- Bleeding gums during brushing or eating. Increase spacing between teeth as a result of tooth movement. Loose teeth. Usually painless, but sometime localized dull pain radiating deep into the jaw. Sensitivity to heat cold or both due to exposed roots. Food impaction. Halitosis. Gingival tenderness or itching.
CLASSIFICATION Disease distribution Site specific disease . Inflammation, pockets, attachment loss and bone loss are due to direct site- specific effects of sub- gingival plaque accumulation as a result of this local effect, attachment loss and pockets may occur.
In addition to being site specific, chronic periodontitis may be described as: 1. Localized: - Periodontitis is considered localized when < 30% of the sites assessed in oral cavity demonstrate attachment loss and bone loss. 2. Generalized: - Periodontitis is considered generalized when >30% of the sites assessed demonstrate attachment loss and bone loss. - The pattern of bone loss in chronic periodontitis can be vertical or horizontal.
Disease Severity Severity can be categorized on the basis of the amount of clinical attachment loss (CAL) as follow: 1. Slight (Mild) periodontitis - When no more than 1 to 2 mm of clinical attachment loss. 2. Moderate periodontitis - 3 to 4 mm CAL. 3. Severe Periodontitis - >= 5 mm CAL.
DISEASE PROGRESSION The rate of disease progression is usually slow but may be modified by systemic and/or environmental & behavioral Factors. Chronic periodontitis does not progress at an equal rate in all affected sites throughout the mouth.
More rapidly progressive lesions occur- 1. Interproximal areas. 2. Areas of greater plaque accumulation. 3. Inaccessibility to plaque control measures. (e.g.: Furcation areas, overhanging margins, sites of malposed teeth, or areas of food impactions)
Clinical diagnosis Inflammation of the marginal gingiva extend to the attached gingiva. Clinical attachment loss. Radiographs (if bone loss)
TREATMENT 1. Non Surgical Therapy Scaling & root planning Antimicrobial therapy Improvement in oral hygiene Removal of all the factors contributing to plaque accumulation. e.g. Correction of ill- fitting appliances, over contoured crowns, overhanging restorations, etc.
2. Surgical Therapy - Pocket elimination procedures. - Regenerative therapy. A. Bone replacement grafts B. Guided tissue regeneration C. Combined regenerative techniques - Respective therapy A. Flaps with or without osseous surgery B. Gingivectomy.