Clinical Algorithm for Predicting Statin Response in Cardiovascular Disease Prevention
A study developed and validated a clinical algorithm to predict sub-optimal LDL-C response in patients starting statin therapy for primary prevention of cardiovascular disease. The algorithm included 11 variables and showed promising performance in two population cohorts. Patients predicted with sub-optimal LDL-C reduction had increased CVD risk over 10 years. Recommendations for clinical practice include considering individual likelihood for sub-optimal response alongside baseline CVD risk assessment.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
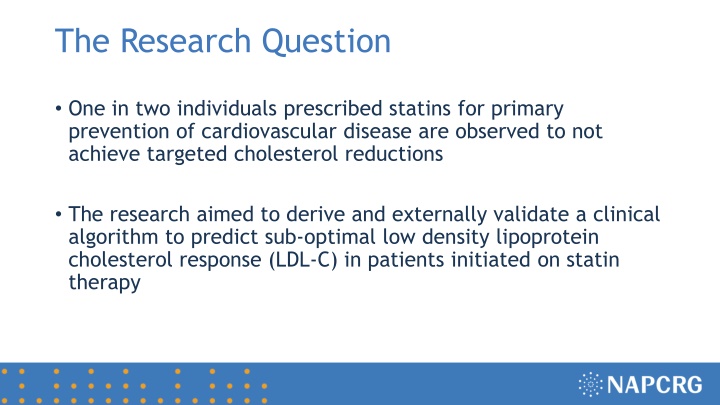
The Research Question One in two individuals prescribed statins for primary prevention of cardiovascular disease are observed to not achieve targeted cholesterol reductions The research aimed to derive and externally validate a clinical algorithm to predict sub-optimal low density lipoprotein cholesterol response (LDL-C) in patients initiated on statin therapy
Research Design and Method Two population cohorts were harmonized and used to develop and validate the clinical algorithm in different primary care settings United Kingdom (Clinical Practice Research Datalink) 183,213 patients initiated on statins Hong Kong (Clinical Data Analysis Reporting Systems) 170,904 patients initiated on statins We used both standard statistical approaches (multivariable logistic regression) and machine-learning algorithms (deep neural network) We assessed performance of the algorithm by area under the curve (AUC) and calibration slope (predicted vs observed risk) We then assessed 10-year risk of any major adverse CVD event, stratifying for predicted statin response and baseline CVD risk.
What the Research Found The clinical algorithm included 11 variables: age, gender, baseline LDL-C, atrial fibrillation, diabetes, dyslipidemia, statin dosage, treated hypertension, oral corticosteroids, non-statin drugs, number of concurrent medications prescribed Performance of the logistic regression model resulted in an AUC of 0.703 in the UK cohort and an AUC of 0.683 in the HK cohort. The more complex machine-learning algorithm resulted almost identical AUC compared to the simpler logistic model (0.702 in UK cohort; 0.682 in HK cohort) Calibration was nearly perfect in the UK population (slope = 1.0), but the algorithm under-predicted risk in the HK population (slope = 0.87) Patients with predicted sub-optimal LDL-C reduction (compared to optimal LDL-C reduction) also experienced significantly increased risk of CVD in both high and low risk CVD groups over 10 years follow-up
What this means for Clinical Practice Determining an individual s likelihood for sub- optimal LDL-C response to statins should be considered along baseline cardiovascular risk assessment to enhance cholesterol management, which could include more routine monitoring, higher dosage, combination therapies, or alternative medication if contra-indicated