Clinical Supervisor Workshop: OT Curriculum and Effective Feedback
This workshop covers the OT curriculum, providing effective feedback, learning from mistakes, and understanding policies and procedures. Sessions include agenda overview, burning questions, entry points into the Masters OT program, curriculum breakdown by year, and expected graduate profile. Course content prior to clinical courses and students' clinical profiles are also highlighted.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
+ Clinical Supervisor Workshop OT afternoon session
+Agenda Brief overview of the OT curriculum Effective feedback using the CBFE-OT Health break Learning from your mistakes FAQs on Policies & Procedures
+ MSc(A) OT Curriculum
Masters OT Program 2 Entry points into the program QY=Students with a previous Bachelor degree (35) CEGEP students (40) 75 Graduates U1 U2 U3/QY M1 M2 B.Sc in Rehabilitation Science (OT option) Master of Science in OT
+Curriculum Year Fall Winter Summer Campus-based Courses Campus-based Courses No courses U1 Campus-based Courses Campus-based Courses No Courses U2 Campus-based Courses Campus-based Courses Clinical Practicum 1 April May (6-week) Clinical Practicum 2 June July (7-week) U3/QY Campus-based Courses Clinical Practicum 3 Jan Feb (8-week) Campus-based Courses (9-week) Research Project M1 Clinical Practicum 4 Sept-Oct (8-week) Graduation (early November) M2
+Graduate Profile A clinician who is: Competent in all essential competencies Self-directed Empathetic and promoting health With practice, the therapist will be: Client centered Evidence-based using resources effectively
Course content prior to the 1stclinical course Manual muscle testing and goniometry Orthotic prescription, design, fabrication and evaluation Physical, cognitive and ADLs standardized assessments Therapeutic Interventions : grading activities; interviewing skills, role play PDSB, Patient Safety, Falls Prevention Child s normal development SOAP charting Wheelchair prescription and positioning, pressure sore prevention Mental health, Neurology, MSK Pediatric, Adult, Elderly
+Students clinical profile 1 physical-medicine adult Across different practice settings (acute care centers, rehabilitation centers, community, long-term care, private clinics) 1 geriatric 1 mental health
+Clinical course pre-requisites Students must successfully complete: PDSB Workshop CPR/First Aid Immunization Mask fitting Confidentiality form signed Language awareness form signed Vulnerable screening police check if requested by site and mandatory student affidavit
+Different models of supervision 1 student to 1 clinical educator (or 2:2) 1 student to 2 clinical educators 2 students to 1 clinical educator Group Role-emerging (peer collaborative model with 3-5 hrs supervision/week) Community service (direct supervision of 18-20 hrs/wk)
+Delivering Effective Feedback within the OT Competencies of Practice Using the Competency Based Fieldwork Evaluation and Student Feedback on Site Learning Program
+Change in Model of Education Fieldwork has moved away from a model of education where classroom learning was followed by skill practice and evaluation within the field setting.
+Philosophy of Fieldwork Education Application of knowledge and skills Transfer of skills Acquisition of context specific knowledge and skills Recognition that fieldwork can occur within any setting in which the profession can develop a role.
+Objectives of Clinical Evaluation Evaluate the student's performance in fieldwork Monitor the student's competency development Ensure the student is qualified to enter professional practice
+Learning Objectives Level 1 Define OT role and develop professional identity Understand the role of OT and comparing the role of OT in other settings Develop observational skills to observe all aspects of OT interventions and communicate observations with clinical educator to report his/her observations to peers, and other team members Interact Professional and demonstrate professionalism initiate contact with other professionals and share client issues understand the role of the interdisciplinary team Demonstrate competency in communication write simple notes share thoughts with clinical educator in a clear manner report client issues using professional terminology in team meetings (with supervision) Perform a client interview and share findings with clinical educator
+Learning Objectives Level 1 Analyze activity (plan activities for treatment and analyze the activities with accuracy) Implement assessments and plan treatment perform parts of or complete assessments (when appropriate) Collect data and synthesize information begin process of synthesizing information gathered from interviews and assessments write short and long term goals Apply the concepts of feedback, critical thinking, clinical reasoning as well as self-directed learning and reflective practice Develop personal learning objectives in CBFE Complete a critical appraisal of a research article
+Learning Objectives Level 2 Demonstrate self-directed learning in daily practice Be able to give and receive feedback to peers, supervisor and other team members Demonstrate initiative, problem-solving and clinical reasoning in all aspects of clinical practice Demonstrate competence in time management, setting priorities and arranging daily schedule (with minimal supervision) Be involved in the whole OT intervention (process as per fieldwork) setting from assessment to treatment and client discharge and understand the specific OT role in each of these stages of client care
+Learning Objectives Level 2 Critically assess patient change and modify care plan as appropriate Demonstrate flexibility and adaptability with regards to client care Be accountable for his/her patients Refine clinical reasoning process by asking questions, finding answers and demonstrating competence in patient care Identify and utilize all available learning resources to achieve competence in placement and enhance learning Develop personal learning objectives (in CBFE) Complete a critical appraisal of a research article
+Learning objectives Level 3 Establish own learning objectives and self-evaluate their performance (in CBFE) Achieve entry-level professional competence in communication, initiative, problem-solving and professionalism Be independent in work management skills Demonstrate entry-level to practice clinical reasoning and critical thinking Carry a workload which is close to that of entry-level practitioner upon completion Be fully accountable for his/her patients and use clinical educator as a coach/mentor. Demonstrate motivation to be involved in other areas of practice and role-emerging areas. Be independent in representing patients in all aspect of health care interventions Liaise with community agencies and be an advocate for his/her patients Complete a critical appraisal of a research article
+7 core competencies in CBFE - OT Professional Interaction and Responsibility Relationship with clients & colleagues Legal & ethical standards Practical Knowledge Discipline specific theory Technical knowledge 4. 1. Clinical Reasoning Analytical and conceptual thinking Judgment Decision making Problem solving 2. Communication Verbal, non-verbal & written 5. Professional Development Commitment to profession Self directed learning Accountability 6. Facilitating Change Assessment Intervention planning Intervention delivery Discharge planning 3. Performance Management Time and resource management leadership 7.
+Scoring Level 1: Scores 1 3: 1 = low Level 1 competencies 2 = rudimentary Level 1 competencies 3 = mastery of Level 1 competencies/transition to Level 2
+Scoring Level 2: Scores 3 - 6: 3 = transition to Level 2 4 = rudimentary Level 2 competencies 5 = intermediate Level 2 competencies 6 = mastery of Level 2 competencies/transition to Level 3
+Scoring Level 3: Scores 6 - 8: 6 = transition to Level 3 7 = rudimentary Level 3 competencies 8 = mastery of Level 3 competencies/ready to enter clinical practice
2. Clinical Reasoning Demonstrates analytical thinking Demonstrates conceptual thinking Demonstrates good judgment and sound decision-making Utilizes good problem solving Demonstrates reasoning based on evidence
Students learning objective (s) Critical Reasoning Resource(s) Required to Meet the Objective(s) Objective(s) Evidence Validation
+ Exercise: Scoring Practice Using the Competency-based Fieldwork Evaluation
+Vicky Level 1 student Undergrad in Rehabilitation Science (OT) Rotation: Private clinic pediatrics and adults Practiced an in-house evaluation and observed her supervisor perform this evaluation > 5 times Takes a long time to complete the evaluation despite the practice and tends to omit parts of the evaluation Requires help to look at the results and generate treatment goals Open to feedback and identifies the areas of improvement and potential tools to help herself
+Rebecca Level 2b student QY student with an undergrad in Psychology Rotation: Acute care setting (Medicine) Adult & Geriatrics Communicates easily with the team members In team meetings, she actively participates by commenting on the activities her clients are doing. When doing initial interviews, she has difficulty to speak loud enough and use a lot of technical terminology . Her progress notes are very detailed, but somewhat repetitive Responsible for making her own schedule Overwhelmed by her large caseload and difficulty to stay up-to-date and to prepare her interventions in advance
+David Level 3 student Undergrad in Biology Rotation: Out patient Mental Health, addiction unit Follows his own caseload (new clients and clients from his supervisor) Performs evaluation on new clients and designs treatment plan Consults his supervisor for some aspect of treatment (especially for different ideas) David s evaluations are thorough but still takes longer than his supervisor to complete Asks for regular feedback and prefers hands-on experience
+Any strategies you would recommend? Schedule time for midterm evaluation upon arrival Obtain feedback from other staff members Include specific areas for improvement and clear expectations Discuss in the midterm and final evaluation meeting the rationale behind the comments Clarify by providing examples to support the feedback Maintain positive approach to evaluation - provide areas of improvement balanced with areas of strength Keep the areas for improvement to a reasonable amount so student can focus on these Set aside time each week to discuss the placement overall Recognize that each placement is unique Allow time for the student to adjust
+Tips for Evaluation Before Meeting Ask student to engage in self evaluation in order to share perspectives While Meeting Give balanced feedback Be specific, give examples, use action verbs Discuss differences in evaluation At midterm, set objectives for rest of placement At final, indicate whether performance expectations were met and identify areas for future improvement Student s and supervisor s signature Provide a copy of the CBFE-OT to the student
+Fostering Self Critique What they want to work on What they need to work Climate and opportunities for self-critique
+Feedback and Expectations Expectations from McGill Expectations for each level of performance Supposing is good, but finding out is better . Mark Twain
+Functions of Feedback To confirm strengths To learn about areas for improvement To identify barriers to achieving goals To encourage alternate behaviors & actions To provide motivation for change.
+Feedback in Fieldwork Students want to know How am I doing? How can I improve? What does my supervisor think of my work? Supervisees reported receiving far too little direct feedback, especially feedback that was critical Gaiptman & Anthony, 1993, Kadushin (1992)
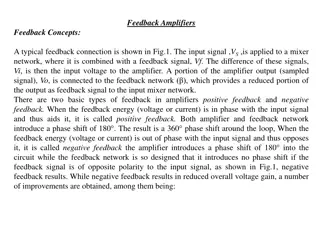
Presumed relationship between fieldwork experience and stages/levels Knowledge and Skills Learned in Stages ENTRY LEVEL CLINICIAN Consolidation Transition Stage 3 Knowledge Application Stage 2 Stage 1 ENTRY LEVEL STUDENT Stages of Professional Competency Development
+Expectations Level 1: Knowledge Application Primary emphasis is: Exploring the role of an OT Development of interaction skills with clients, family members, fieldwork educators and other health care personnel Style of supervision: Direct and active Primary Role of Preceptor: Educator
+Feedback to Level 1 Students Articulate performance expectations and objectives clearly Provide specific instructions of how to do things Feedback: Direct, concrete, frequent Consistent Supervision always readily available
+Expectations Level 2: Transition Primary emphasis is: As much practice and experience as possible! Style of supervision: Collaborative Primary role of preceptor: Coach
+Feedback to Level 2 Students Promote student self-reflection Prompt with appropriate questions Engage in discussion of several solutions to occupational performance problems Encourage student to begin to make decisions about the most viable course of action.
+Expectations Level 3: Consolidation Primary emphasis is: Final preparation for entry to practice Independence in application of the occupational therapy process Style of supervision: Consultative Primary role of preceptor: Mentor
+Feedback to Level 3 Students Student self-reflection should be self-initiated Encourage student to identify and pursue professional learning needs Work "collegially" with the student
+How to give feedback? Take into consideration the receiver s needs Describe the situation carefully and accurately first Verify the comprehension Accept the responsibilities Give feedback: for the good reasons at the right time and place appropriate and relevant to the context in small quantities
+Constructive Feedback Is offered on a voluntary basis (should not be imposed) Is descriptive ( interpretation) Is clear and concrete ( general) Focus on problems ( the person) Includes the ability to change
+Strategies for Giving Feedback Feedback should be kept to a reasonable amount Give bite-sized, time- limited chunks of feedback that are easy to comprehend and digest
+Strategies for Giving Feedback Be the One Minute Supervisor Give One minute feedback Recognize what the student is doing well Try to stick to a few key points per discussion.
+Providing feedback to Rebecca Meal preparation evaluation Provides clear and understandable instructions Conscientious of her client s safety (stay close by) Did not notice the poor posture and compensations used by her client Appears uncomfortable reminding her client that she had forgotten to turn off the stove When her client asked for feedback about the evaluation, she told her client that she did a great job, without informing her of the many difficulties observed
+ Learn from your mistakes
+ Policies: Frequently Asked Questions?