Combination of Abilify and Propofol Leading to Tardive Dyskinesia: A Case Presentation
A case study involving a 53-year-old female with a complex medical history who developed symptoms of Tardive Dyskinesia following a diagnostic bronchoscopy under general anesthesia. The patient's previous use of Abilify and Propofol raised concerns about the potential adverse effects of this combination. This comprehensive case presentation highlights the importance of medication management and monitoring in patients with multiple comorbidities.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Abilify and Propofol, a concerning combination leading to Tardive Dyskinesia A Case Presentation By Dr. Daniel Blair, R3 NCH Internal Medicine Residency Program Rural Research Symposium April 26th, 2018
HPI A 53 year old female, after a diagnostic bronchoscopy under general anesthesia for idiopathic pulmonary fibrosis, was noted to have immediate new onset of symptoms upon extubation from the ventilator. She presented to the clinic for post-op, and was found to have prominent repetitive tongue protrusion, and right lower extremity spasms. She was a well-known long-term patient at our community clinic, with a very complex medical history, including a new diagnosis of idiopathic pulmonary fibrosis, with concern for rheumatoid arthritis as the cause. In addition to these medical symptoms, she had recently been changed on her depression medications to Abilify two months prior to this procedure.
Medical History Cerebral Aneurisms Chronic Persistent Afib Several DVT And PE s, Requiring Coumadin Depression And Anxiety Epilepsy COPD (?) Type II Diabetes Mellitus Recurrent Pneumothorax Ischemic Strokes x1, Hemorrhagic Stroke x2 Obstructive Sleep Apnea Subarachnoid Hemorrhage Endometriosis Rheumatoid Arthritis Coronary Artery Disease, Status Post MI x2 Recent Diagnosis Of Idiopathic Pulmonary Fibrosis
surgical history (Pertinent ones) Open Laparotomy with tumor resection Laparoscopic cholecystectomy Chest tubes Greenfield filter placement Intracranial aneurysm repair x2 Ventriculostomy tube placement for hemorrhagic stroke x2 (later removed)
Family history: Mothers side of the family had diabetes, heart disease, hypertension, osteoporosis, AAA, Father had heart disease and hypertension Social: Disabled. Married with only sexual partner, never smoker, never drank alcohol. 3 children (adults) plus spouse and their kids, for total of 15 people in the house. Requires Cane Allergies: FluShield Influenza Virus Vac INJ (Syncope) and Pneumovax 23 INJ (Syncope)
ROS Constitutional: feeling poorly and feeling tired, but no fever and no chills. Eyes: no eye pain, eyes not red, no eyesight problems and no purulent discharge from the eyes. ENT: no earache, no hearing loss, no postnasal drip, no nosebleeds, no nasal discharge and no sneezing. Cardiovascular: intermittent leg claudication and lower extremity edema, but the heart rate was not slow, the heart rate was not fast, no chest pain and no palpitations. Respiratory: shortness of breath and shortness of breath during exertion, but no wheezing, no cough, no orthopnea and no PND. Gastrointestinal: no abdominal pain, no vomiting, no nausea, no constipation and no diarrhea. Genitourinary: no dysuria, no incontinence, no sexual dysfunction, no pelvic pain, no dysmenorrhea and no libido change. Musculoskeletal: arthralgias, joint pain, joint swelling, joint stiffness and limb pain, but no back pain. Integumentary: no skin lesions, no skin wound, no itching and no change in a mole Neurological: Uncontrolled movements of Right LE and tongue, twitching. no confusion, no convulsions, no dizziness and no fainting. Psychiatric: sleep disturbances, anxiety and depression, but not suicidal, no personality change and no emotional problems. Endocrine: no proptosis, no hot flashes and no deepening of the voice.
Meds (28) Abilify 10 MG 1 PO Daily Januvia 100mg 1 PO Daily Atrovent HFA 17 MCG/ACT Inhaler Levetiracetam 500mg, 1 PO BID Levothyroxine 100 MCG 1 PO daily Centrum Silver Ultra Women s 1 PO Daily Ursodiol 300 MG Oral Capsule Meclizine 25mg Claritin 10 mg 1 PO Daily Medroxyprogesterone Acetate 10mg Clonazepam 0.5mg Melatonin 10 MG Oral Tablet Fish Oil 1000 MG 1 PO BID Miralax Oral Powder 1 cap full daily Vitamin D3 50000 Unit Omeprazole 20mg 1 PO Daily Lexapro 20 MG Ondansetron 8 MG PO PRN Warfarin Sodium 3 MG Chronic 3L NC Oxygen Therapy Famotidine 20 MG Probiotic Acidophilus Ferrous Sulfate 325 (65 Fe) MG Oral Simvastatin 40 MG Fluticasone Propionate 50 MCG/ACT Nasal Spray Furosemide 20mg 1 PO Daily PRN Edema Hydrocodone-Acetaminophen 5-325 MG 1 PO BID PRN Ipratropium-Albuterol 0.5-2.5MG/3ML Nebulizer QID
Physical Exam General Appearance: In acute distress, the patient's affect was abnormal, flat, and not healthy appearing, but is A 52 year old female who presents: alert, appears older than stated age. HEENT: Normocephalic, atraumatic, with irregular pulsatile tongue protrusion, interfering with speech as well as shows difficulty with closing mouth. Cardiovascular: Irregularly Irregular, without signs of murmurs, rubs, or gallops Pulmonary: no signs of respiratory distress, on 3l NC, normal respiratory rhythm and effort, clear bilateral breath sounds and the lungs were clear to auscultation bilaterally. Abdomen: normal bowel sounds, soft, no abdominal mass palpated and non-tender. Extremities: lower extremity edema was present, with clubbing of the fingernails, showed no cyanosis and dorsalis pedis pulses were abnormal. Musculoskeletal: abnormal repetitive movement of all extremities, most prominent of Right Lower Extremity, similar to an abnormal tapping of foot, muscle strength and tone were abnormal. (weaker on right side, 2/5 strength on Right, 3/5 on Left). Skin: abnormal skin color and pigmentation with abnormal skin turgor, but no rash and no skin lesions.
Differential Diagnosis Succinylcholine And Etomidate- General Anesthesia Unlikely and short lived half-life. No Hx of interactions with Abilify, nor would their mechanisms affect the brain in a similar way. Acute dyskinesia- typically occurs immediately after introduction of an antipsychotic drug, but may resemble TD. Acute dyskinesia can sometimes occur late in treatment after switching to a more potent antipsychotic drug.
Differential Diagnosis Dystonia is a movement disorder characterized by sustained or intermittent muscle contractions causing abnormal, often repetitive, movements, postures, or both. It s movements are typically patterned, twisting, and may be tremulous. It is usually worsened by voluntary action and associated with overflow muscle activation Usually also in younger males
Assessment and Plan 1) Extrapyramidal dysarthria vs Tardive Dyskinesia- patient states that the tremors began in her mouth, shortly after her extubation from ventilator about week ago. Two months ago she was started on Abilify 10 mg. I have Increased concerns for and a high degree of suspicion that this is extrapyramidal effects due to the Abilify and propofol. Will Immediately wean off Abilify, with plan to take 1 week of 5 mg, and then stop the medication. Additionally this was started by psychiatrist at Saint Mary's family prevention Center, thus we will try and call to have her appointment moved up to as soon as possible. Patient states that the tremor started in her mouth, and then continued to worsen, noted prominently in the right leg. Her leg continues to shake dramatically unless pressed down, and continued even then, with noted fasciculations and tremors in her foot. She states that the tremors do not stop when she is asleep, and frequently wake her up, worsening her complaint of insomnia. As such I will follow up with her in 2 weeks once the Abilify has been stopped, and she is to discuss with the psychiatrist the possibility of increasing her Lexapro from 20 mg to 40 mg. Additionally she is to call back if the Norco is no longer helping with the pain, with considerations of possibly adding a muscle relaxer such as Flexeril.
Assessment and Plan 2) Generalized Weakness- continued generalized weakness, as mirrored in the musculoskeletal exam, showing profound weakness. Initially planned on physical therapy, however at this time due to extensive leg tremors and concerns with extrapyramidal symptoms, will hold off on physical therapy at this time, as she has continued to have constant leg cramping and pain due to the tremors. Once these tremors have resolved, will discuss further physical therapy at that time, with goals of making her stronger and increase mobility. Additionally today, we also discussed her previous medical history, refilled multiple medications, and discussed prior visits with other specialists, including pulmonologist and neurologist. As Dr. Pendola the neurologist is leaving in January, I will continue to prescribe her Keppra and migraine clear. She is also to follow up with Dr. Raj, her pulmonologist soon, as all
Follow-up Over the next three months, I began seeing the patient about every two weeks. Dr. Bentley and I both agreed that this was most likely tardive dyskinesia. After the first visit, two weeks later if the initial encounter, we started her on Cogentin (Benztropine). Cogentin is the only additional medication, other than Abilify, that is been shown to show some benefit with these symptoms. While it did show only little improvement in studies, as seen on up-to-date, as discussed in the assessment and plan, she did need to have a muscle relaxer on board. Initially in the first month, there is very little improvement, even after having stopped her Abilify, however we also found out that she was initially unable to afford the Cogentin. Her counselor at that time also agreed to stop the medication, but had no additional recommendations. The patient and her husband also agreed that they did not want to travel extensively just for symptom management. By one month, the tongue spasms and for circulation s had improved. By month and , the only symptoms left were mild tongue protrusion and right leg spasms. By 2 months, all symptoms are completely resolved.
Tardive dyskinesia Tardive Dyskinesia is becoming one of the less seen side effects observed with newer generations of antipsychotics. Once the diagnosis was made based on the noted symptoms, a cursory search of current evidence revealed that the initial step was to stop all likely offending medications. In her case, the Abilify was quickly stopped, and her psychiatrist was notified. She was already on Klonopin, for her chronic anxiety, and this was having no avail after having stopped the Abilify.
Treatment with Cogentin however was delayed slightly, due to her inability to afford the medication at that time. However, within two weeks of her starting the medication, which roughly was after a month and a half of symptoms, her symptoms began to improve quickly. After three months after the symptoms began, as well as about a month and a half of being treated on Cogentin, and having stopped Abilify, all of her symptoms had resolved, including the tongue protrusion.
Interestingly though, Abilify had actually been used in other patients for treating tardive dyskinesia in 2011, but has been noted for actually causing more of the TD symptoms in patients without other medications. As this does appear to be the inciting medication combined with propofol, some research based on other case studies show this may be a concerning medication that could lead to TD. To our knowledge, this interaction with propofol has never been previously noted, as tardive dyskinesia is typically diagnosed with dopamine blocking medications. At this time, we had no neurology consults available, and the large majority of the treatment and plan for this condition was done in our community clinic.
So, what is Tardive dyskinesia? (TD) is a hyperkinetic movement disorder that appears with a delayed onset after prolonged use of dopamine receptor blocking agents, mainly the antipsychotic drugs and the antiemetic drug, metoclopramide. Second-generation (atypical) antipsychotic agents are being used more however, because of their lower risk of causing extrapyramidal symptoms and TD. It is usually after months to years of therapy with dopamine receptor blockers, patients will experience involuntary choreiform, athetotic, or ballismic dyskinetic movements which define TD. These movements most commonly involve the mouth, tongue, facial muscles, axial dyskinesias, and extremities.
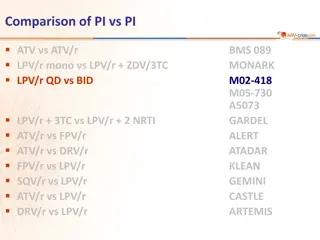
Typical risk factors associated with the development of TD include older age, pre- existing movement or neurodegenerative disorders, female sex, the presence of affective illness, and neuroleptic exposure of more than six months. The use of higher-potency, first-generation agents is also more likely to increase the risk of TD and extrapyramidal symptoms (EPS). However, among the SGAs currently available, those with more transient D2receptor blockade and lower D2affinity, such as quetiapine (Seroquel, AstraZeneca), are associated with the smallest risk, at least for EPS and probably TD. At a therapeutic dose, it is noteworthy that aripiprazole has one of the highest D2 receptor affinities
References Schwartz T, Raza S. Aripiprazole (Abilify) and Tardive Dyskinesia. Pharmacy and Therapeutics. 2008;33(1):32-34. Tarsy, MD, D. (2017). Tardive dyskinesia: Prevention and treatment. [online] Uptodate.com. Available at: https://www.uptodate.com/contents/tardive-dyskinesia-prevention-and- treatment?source=search_result&search=tardive%20dyskinesia&selectedTitle=2~150#H8 [Accessed 25 Jun. 2017]. Kang N-R, Kim M-D. Tardive Dyskinesia: Treatment with Aripiprazole. Clinical Psychopharmacology and Neuroscience. 2011;9(1):1-8. doi:10.9758/cpn.2011.9.1.1.