COMMUNICATION IN HEALTH CARE
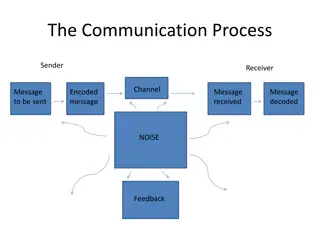
Addressing communication breakdowns in healthcare, this content explores the SBAR tool's effectiveness in promoting patient safety and preventing adverse events. It emphasizes the importance of enhanced communication among healthcare providers, patients, and caregivers to enhance care quality. The significance of National Patient Safety Goals and statistics from The Joint Commission on communication-related sentinel events are highlighted. Enablers and barriers to effective communication, as well as factors contributing to communication errors, are discussed.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
COMMUNICATION IN HEALTH CARE SBAR Tool
Learning Objectives 1. To identify the nature and causes of communication breakdown in health care. 2. To understand the SBAR tool and its effectiveness in preventing communication breakdown and promoting patient safety.
3. To develop skill in using SBAR. 4. To identify strategies for implementing SBAR. 5. To understand how SBAR should be used.
Patient Safety Primary Purpose Improved communication among health care providers and patient/caregivers will improve the quality and safety of the care the patient receives.
National Patient Safety Goal focused on improving the effectiveness of communication among caregivers.
The Joint Commission Sentinel event stats found that communication issues were the root cause of about 65% of the sentinel events reported between 1995- 2004. Many of these events resulted in patient death.
Enablers/Barriers Team Work to include, trust and respect, communication, leadership, inclusiveness. Culture to include, leadership, hierarchical structures, communications and systems approach Resources to include, staffing, equipment and supplies, environment. Responsibility to include, Organizational (e.g. structures and systems, managing change, corporate and individual program, staff safety, individual.
Communication Errors Contributing Factors Human Performance Limitations Interpersonal Dynamics Hierarchical structures Cultural Differences Gender Differences Disciplinary Differences Individual differences and Filters
Team Functioning and the Clinical Environment situational awareness learning environment communication processes/structures
Team Functioning and the clinical environment Situational Awareness Multiple information sources with multiple players Incomplete information Rapid changes with clinical scenarios Ineffective Communication Structures Hand-offs and transitions Team rounds Limited Time Ineffective response to errors
Consider the impact of: limited memory capacity stress fatigue multi-tasking
Consider also: 1. pecking order may prevent sharing 2. individuals not confident in own observations and recommendations 3. What does it mean to question 4. Culture & Gender influence communication content and style
Communication between Disciplines Additional Dynamics between providers to consider: 1. Medicine/Nursing Brief details vs. narrative or descriptive 2. OT-PT Order vs. Flexibility, Judgers vs. perceivers 3. Pharmacy focuses on observable data
We bring different filters to work. It is important to identify these differences and develop a shared structure to support effective communication
Communication errors are a team and system approach
SBAR APPROACH We need to create a culture that examines errors in light of interpersonal dynamics and communication structures
WHAT IS SBAR? The SBAR model will be used to facilitate accurate and thorough patient handoff communication between care providers. This will include a focused process in communication with Physicians in relation to clinical situations.
SBAR Always identify yourself and the patient at the beginning of an SBAR S=Situation the problem or concern B=Background the relevant clinical data A=Assessment relay your findings R=Recommendations action or request needed
Human Factor response concepts Appropriate Assertion Critical Language Situational Awareness: What are the red flags Create the learning environment including debriefing A COMMON DEBRIEF MODEL IS SBAR
Assertion: individuals speak up, and state their information with appropriate persistence until there is clear resolution
Assertion Barriers: Power Differences Lack of common mental model Don t want to look stupid Not sure when you are right Others??
Overcoming Barriers: Get the person s attention Express Concern State the Problem Propose an Action Reach Decision
Critical Language We have a serious problem, stop and listen to me C=I m Concerned U=I m Uncomfortable S=This is Unsafe
Situational Awareness Maintain the Big Picture Quality of Care Safety Think ahead and plan Discuss contingencies Tune into Red Flags
RED FLAGS Ambiguity Poor communication Confusion Doing something new under pressure Verbal Violence Doesn t feel right Boredom Task saturation Being rushed Deviating from established norms
Create a learning environment: DEBRIEFING After the event/situation ask: What did the team do well? What were the challenges? What will we do differently next time?
SBAR EXAMPLES Case SCENARIOS SEE HANDOUTS
Successful SBAR Implementation Support from Leadership Teamwork Training Use of Standardized/structured tools Errors are not considered clinical incompetence Team members respond to requests in positive collaborative manner
When to use SBAR Time sensitive or critical situations Treatment decisions requiring same page collaboration Phone call to MD s/team members Hand-offs/transitions in care When you need clarity
Reminders: Think out loud/sounding board Close the Loop with an action and accountability Be prepared with needed info before making a phone call
Expect a response to your request for help USE critical language Support each other using SBAR
NEXT STEPS 1. Take this information back to your facility 2. Share this information with the clinical staff 3. Determine the best way to implement SBAR in your facility
4. Share feedback at the April 8th Focus Group meeting 5. Be prepared to fully implement SBAR with your staff by the 28th of April 6. Call for assistance if additional information or education is needed for your facility.
QUESTIONS?? CONTACT Michelle Nelson Robin Moreno If additional information or assistance with education is needed. THANK YOU