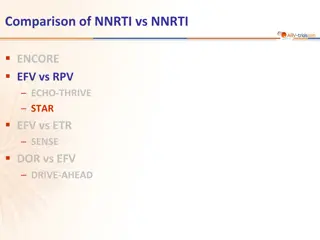
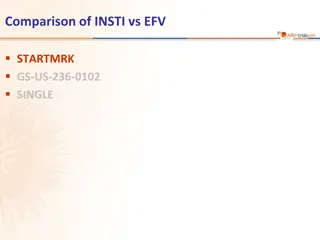
Comparison of INSTI vs INSTI in HIV Treatment Studies
This content provides a detailed comparison of Raltegravir taken once daily versus twice daily with TDF/FTC in various HIV treatment studies, including key findings, patient characteristics, treatment responses, and safety profiles at week 48.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Comparison of INSTI vs INSTI QDMRK Study SPRING-2 Study ONCEMRK Study GS-US-380-1489 Study GS-US-380-1490 Study
QDMRK Study: raltegravir QD vs BID, with TDF/FTC Design Randomisation* 1 : 1 Double-blind W48 W96 RAL 400 mg BID + RAL 800 mg QD placebo N = 389 > 18 years ARV-na ve TDF/FTC fdc QD HIV RNA > 5,000 c/mL Any CD4 cell count No resistance to TDF or FTC RAL 800 mg QD + RAL 400 mg BID placebo TDF/FTC fdc QD N = 386 *Randomisation was stratified by baseline HIV RNA (< or > 100,000 c/mL) and viral hepatitis co-infection status Objective Non inferiority of RAL QD: % HIV RNA < 50 c/mL by ITT, NC=F (lower margin of the 2-sided 95% CI for the difference = - 10%, 90% power) Eron JJ, Lancet Infect Dis 2011;11:907-15 QDMRK
QDMRK Study: raltegravir QD vs BID, with TDF/FTC Baseline characteristics and patient disposition RAL BID RAL QD Randomised and received treatment, N Median age, years Female White/Black/Other HIV RNA (log10c/mL), median HIV RNA > 100,000 c/mL CD4 cell count (/mm3), median CD4 < 200 per mm3 HBsAg+ or HCV Ab+ Discontinuation by W48 For lack of efficacy For adverse event Lost to follow-up Other reasons 388 38 18% 382 38 23% 70% / 15% / 16% 4.8 38% 278 26% 6% 25 (6.4%) N = 5 N = 2 N = 7 N = 11 72% / 13% / 15% 4.9 37% 285 23% 7% 42 (11.0%) N = 18 N = 3 N = 7 N = 14 Eron JJ, Lancet Infect Dis 2011;11:907-15 QDMRK
QDMRK Study: raltegravir QD vs BID, with TDF/FTC Response to treatment at week 48 HIV RNA < 50 c/mL RAL BID HIV RNA < 50 c/mL at W48 (NC=failure analysis) by baseline factors RAL QD % Primary analysis 100 91.0 Baseline RAL BID RAL QD 88.9 86.6 83.2 RNA < 5 log10c/mL RNA > 5 log10c/mL 91.9%* 84.2% 89.1%* 74.3% 75 CD4 > 200/mm3 CD4 < 200/mm3 91.6% 80.8% 87.0% 70.8% 50 HIV-1 B subtype Non-B subtype 90.3% 96.3% 88.5% 90.9% 25 * 95% CI for the difference = - 8.3 ; 2.7 N = 386 382 377 367 0 Mean CD4/mm3increase at W48 (observed-failure analysis): + 196 (RAL BID) vs + 210 (RAL QD) Per protocol, observed-failure* 95% CI for the difference = (- 9.0 ; 0.2) ITT NC = F 95% CI for the difference =( - 10.7 ; -0.8) * Exclusion of discontinuations due to intolerability or reasons unrelated to treatment Eron JJ, Lancet Infect Dis 2011;11:907-15 QDMRK
QDMRK Study: raltegravir QD vs BID, with TDF/FTC Safety at W48 RAL BID RAL QD Clinical adverse events Drug-related AE Serious drug-related AE Treatment discontinuation due to AE Laboratory adverse events Drug-related AE Treatment discontinuation due to AE Moderate to severe adverse events of any cause Diarrhoea Headache Depression Vomiting Grade 3 or 4 laboratory abnormality in > 2% of patients in either group Fasting LDL-cholesterol > 190 mg/dL (4.9 mmol/L) Creatine kinase ALT / AST 24.2% 0.5% 1.0% 26.4% 0.3% 1.0% 2.3% 0 48% 4% 4% 2% 3% 1.3% 0.3% 45% 4% 3% 3% 2% 2.0% 5.4% 1.4% 3.9% 3.4% / 3.4% 2.9% / 1.8% Eron JJ, Lancet Infect Dis 2011;11:907-15 QDMRK
QDMRK Study: raltegravir QD vs BID, with TDF/FTC Virologic failure: definition Non-response = never achieved 2 consecutive HIV RNA < 50 c/mL by week 24 or at time of premature study discontinuation or rebound = after an initial response, confirmed HIV RNA > 50 c/mL RAL BID N = 388 RAL QD N = 382 Emergence of resistance in virologic failure Protocol-defined virologic failure 35 (9%) 53 (14%) Non-response 14 22 Rebound 21 31 Assessed for emergence of resistance mutations * 16 30 No result available (technical issue) 2 2 Raltegravir resistance mutations + M184I/V 2/12 9/27 M184I/V alone 4/13 11/28 No resistance 8/14 8/28 * Genotyping was done only in patients with HIV RNA > 400 c/mL 2/2 (RAL BID) and 7/9 (RAL QD) patients who had emergence of RAL resistance had baseline HIV RNA > 100 000 c/mL Eron JJ, Lancet Infect Dis 2011;11:907-15 QDMRK
QDMRK Study: raltegravir QD vs BID, with TDF/FTC Pharmacokinetic Data Trough raltegravir concentrations were more than six times higher with twice-daily dosing than they were with once-daily dosing Although an association between trough RAL concentrations and efficacy was evident in the once-daily group, no clear threshold could be identified Eron JJ, Lancet Infect Dis 2011;11:907-15 QDMRK
QDMRK Study: raltegravir QD vs BID, with TDF/FTC Conclusion At 48 weeks of treatment, RAL QD was not non-inferior to RAL BID, in combination with TDF/FTC Virologic failure was more common with once-daily dosing especially in patients with baseline HIV RNA > 100 000 c/mL More patients in the once-daily group than in the twice-daily group had resistance emergence to both RAL and FTC at the time of virological failure Patients in the once-daily group with low pharmacokinetic values and high baseline viral loads were at particular risk of treatment failure Despite a high response rate, RAL at 800 mg QD cannot be recommended in place of twice-daily dosing for first-line antiretroviral therapy Eron JJ, Lancet Infect Dis 2011;11:907-15 QDMRK