Comprehensive Educational Presentation for Research Investigators
This presentation provides valuable information for individuals involved in Social, Behavioral & Educational Research, covering topics such as Investigator Responsibilities, Study Feasibility Evaluation, and Qualifications required for conducting research projects. It emphasizes the importance of thorough assessment before undertaking a study and outlines key obligations for investigators. The resources shared aim to support new and seasoned researchers in navigating research processes effectively.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
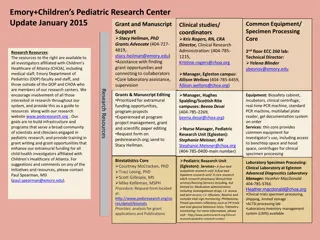
Presentation Transcript
This comprehensive, educational presentation for Social, Behavioral & Educational (SBE) Research is a resource tool provided by WMed Homer Stryker M.D. School of Medicine for participants in Investigator-initiated studies. It was specifically designed for investigators who are new to research or who have not been involved in research for some time to answer questions you may encounter as a research investigator. The WMed Human Research Protection Program (HRPP) and Institutional Review Board (IRB) Handbook outlining a more condensed version of Investigator Responsibilities (Section 19) is available on the HRPP website (provide link). In addition, a condensed version of Investigator Responsibilities is available on the HRPP website (provide link) If you have any other questions or concerns that are not answered in this slide presentation, please do not hesitate to call the Education-Quality Improvement Program (E-QIP) Team at: 269-337-4322 or 269-337-4323.
Definition The Principal Investigator (PI) is used to identify a researcher/individual who has full and final responsibility for the conduct of a research project. Social, Behavioral & Educational Research examples include: Epidemiology Database not a medical or clinical protected health information database Ethics Surveys, Questionnaires Studies that utilize medical student records which may also include records with personal information
Investigators must thoroughly evaluate a study trial/project before agreeing to conduct it. An investigator s willingness to conduct a research project depends on many factors, including the investigator s expertise and interest, perceived ability to meet recruitment goals, and whether sufficient support staff and other resources are available. This evaluation is often referred to as study/project feasibility. ICH (2016) ICH 6 Section 4.1 notes a number of investigator obligations: The investigator(s) should be qualified by education, training, and experience to assume responsibility for the proper conduct of the trial, should meet all the qualifications specified by the applicable regulatory requirement(s), and should provide evidence of such qualifications through up-to-date curriculum vitae and/or other relevant documentation requested by the IRB/IEC, and/or the regulatory authorities.
Does the investigator have the facilities and equipment available to perform the study? Does the investigator have adequate time to devote to study oversight and the work that he/she must perform? Does the investigator have adequate personnel available to assist and complete the required work? Have the PI and all study team members completed WMed CITI training requirements? Have all billing/budget/grant questions been clarified with the Director, Sponsored Programs Administration
In order to ensure the protection, rights and well-being of subjects, the PI is responsible, but not limited to: 1. Comply with the principles of the Belmont Report and adherence to all applicable regulatory requirements. 2. Comply with the guidelines as outlined in the required CITI Course modules. 3. Maintain a study team list and ensure that only appropriately qualified persons (to whom tasks may be assigned for study purposes) have had adequate training. 4. Provide adequate training for all study personnel and documentation of such: -CV, special certification(s) if applicable -Documentation (sign-in sheet) that the PI conducted a training session where the study team was trained on the protocol
5. Obtain written documentation of IRB approval, or exemption, of the study prior to initiating human subjects research. 6. Ensure that legally effective informed consent has been obtained using an adequate and appropriate consent process, and ensuring the consent process is documented appropriately unless the IRB has granted a waiver of informed consent or documentation of informed consent. WMed informed consent form templates are available on the WMed IRB website. Insert link 7. Ensure permission for the use and disclosure of protected health information is obtained in compliance with the HIPAA Privacy Rule if the research staff are within the Health Care Component or part of the Affiliated Covered Entity. 8. Ensure compliance with the conditions of IRB approval, which included following the procedures and using the exact materials within the IRB-approved application and protocol. In the case of exempt human subject research, monitor for changes that could alter the exemption determination and consulting with the IRB as necessary. .
9. Obtain IRB approval for any proposed protocol changes in research before implementing the change: Modifications and Amendments to the approved protocol (changes to the original submitted study must be reviewed and approved by the IRB before they are implemented). Changes may not be initiated from the protocol without IRB approval unless necessary to eliminate immediate harm to subjects. For any changes initiated to eliminate immediate harm to subjects, they must be reported after the event occurred. - Document and explain any/all deviation(s) All subject recruitment materials must be approved prior to use. Any revisions to surveys/questionnaires/demographics/ICFs, etc.
Adverse Events and Unanticipated Problems involving risks to subjects or others (the IRB must be notified immediately if any undue harm results from the study). Complaints regarding Human Subjects Research (the IRB must be notified immediately if any complaints, either from the subjects or the study staff, are made regarding the research study). Breach of Confidentiality (if any personal/confidential data has been inappropriately disclosed by any member of the study staff, the IRB must be notified immediately). Report deviations that may affect subject safety immediately to the IRB. e.g. dosing errors, failure to perform a safety measure, loss of identifiable data (stolen laptop).
10. Report noncompliance to the IRB. 11. Ensure adequate records are kept to document study procedures and adherence with the IRB-approved application and protocol, as well as ensuring the records are retained and accessible for the required retention period. 12. Register studies and provide updated information to ClinicalTrials.gov, when applicable. 13. Ensure that additional procedures are in place for investigator-initiated, multi-center studies. 14. Submit continuing review progress reports in a timely manner.
Although PIs may delegate certain research-related tasks to other members of the research team, they retain ultimate responsibility for the conduct of the study. The PI is the person responsible for the legal and ethical conduct of the study in accordance with the protocol, signed investigator agreements, and applicable regulations. The PI must be qualified by education, training, or experience to assume this responsibility. Investigators are responsible for certifying that research team members have completed WMed CITI training and any additional protocol-required training to ensure they are aware of the regulations governing human subjects research and understand and adhere to the IRB-approved research protocol. Compliance with these standards provides assurance that the rights, safety, and well-being of human subjects are protected and the integrity of the data collected.
Certain tasks may be delegated to qualified members of the research team, but the responsibility for ensuring tasks are performed in accordance with the protocol and regulations is the PI s, and cannot be delegated. The PI should ensure that a member of the research team to whom a task is delegated is qualified by education, training, and experience (and state licensure where relevant) to perform the delegated task(s). PIs must also ensure that adequate resources are available for the conduct of the study. The investigator should have sufficient time and adequate resources to properly and safely conduct the research project.
There is general consensus on the importance of informed consent in research. Most people have the expectation that they have the right to make decisions about what will and will not be done to them and about what personal information they will share with others. Informed consent is a process that begins with the recruitment and screening of a subject and continues throughout the subject s involvement in the research. It includes: Providing specific information about the research project to subjects in a way that is understandable to them. Answering questions to ensure that subjects understand the research and their role in it. The PI or designee is encouraged to use the teach-back method to confirm that the subject understands the information presented. If a survey instrument or an interview script contains questions that subjects are likely to find intrusive, they must be informed about the nature of the questions in advance. Studies about sexual behavior, childhood abuse, use of psychotropic medications, and other personal topics should include a disclosure in the consent form about the sensitive nature of the questions.
Giving subjects sufficient time to consider their decisions (this is particularly true if the study procedures involve more than minimal risk or will require subjects to disclose sensitive information). Obtaining the voluntary agreement of subjects to take part in the study. The agreement is only to enter the study as subjects may withdraw at any time, decline to answer specific questions, or complete specific tasks at any time during the research. Federal regulation at 45 CFR 46 (Protection of Human Subjects 2009) about informed consent list specific elements that are required including basic elements/additional elements if applicable.
Unless the IRB determines that a waiver of informed consent or waiver of a signed informed consent document is appropriate for a study or has determined a study to be exempt, an investigator is also responsible for ensuring: 1. Informed consent is obtained and documented using only current IRB approved consent form(s). 2. The subject receives a copy of the informed consent document for their personal records. 3. Informed consent is obtained prior to the conduct of any research procedures.
Consent documents with the IRB approval and expiration dates (that require a written signature) should be used to obtain written consent from subjects. All subjects must be given a copy of the consent form to keep for their personal records. PIs are responsible for ensuring the conduct of an adequate and appropriate consent process. When referring to Informed Consent , it is important to differentiate between the informed consent document and the informed consent process. Obtaining informed consent is a process and not just obtaining a signature on a form. PIs are required to ensure that the consent process is conducted and is appropriate for the research study and subject population.
PIs are also responsible for ensuring the consent process is documented appropriately. Unless the IRB has granted a waiver of informed consent or a waiver of informed consent documentation, the study team should have a process in place to document the consent process, and any assent process (in the case where minors or individuals with impaired decision-making capacity are enrolled) in research files for each subject.
In an academic institutional setting, students play an integral role as subjects in certain research situations (for example, research dealing with teaching methods, curricula, and other areas related to the scholarship of teaching and learning). An underlying principle of the regulations governing the involvement of human subjects in research is that the subject s participation is voluntary and based upon full and accurate information. Consistent with an overall concern that research subjects should not be coerced to participate, student and faculty researchers should take particular care to avoid the unintentional or subliminal coercion that may occur when potential subjects are also students. For this reason, faculty researchers, in particular, must avoid involving their own students as research subjects. Faculty who wish to involve their own students as subjects should be able to provide a good scientific reason, rather that convenience, for selecting those students as research subjects. The research project should be relevant to the topic of the class, and participation should be part of the learning experience for the students.
In instances where investigators can provide a good reason for involving their own students in their research, the IRB generally requires that someone other than the investigator (instructor) obtain informed consent and collect the data. When this is not possible, the IRB will consider other methods for obtaining consent and collecting data that would not reveal to the instructor whether or not a specific student participated in the research project until after final grades have been determined. The students should be informed of what these procedures are in the informed consent form. In addition, it is generally recommended that the investigator/professor provide a recruitment flyer or letter to a student pool, general student population or both so that the student may be the one who initiates contact with the investigator/ researcher.
All students have certain rights as a research subject. If a student feels he/she has been coerced to participate in a study, he/she should immediately inform the institution s compliance office and/or the IRB. Consent Form In accordance with the principles of free and informed consent, privacy, and confidentiality, and in consideration of the vulnerable nature of students as research subjects, students have the right to a consent form that addresses key points of the study. Assessing Risk Risk is the probability of harm or injury (physical, psychological, social, or economic) occurring as the result of participation in a research study. Research in the social, behavioral & educational sciences sometimes does pose risks to subjects. Risks are specific to time, situation, and culture. Common social, behavioral & educational science methodologies such as surveys, questionnaires, and interviews are considered generally low risk because they do not involve physically invasive procedures with associated risk of physical harm.
However, depending on the sensitivity of data being collected, there can be the potential of reputational harm especially if the research subjects are considered a vulnerable patient population. Risk Resulting from Study Questions/Surveys Particularly in SBE projects, subjects may feel stress caused by the research questions or procedures. Most psychological risks are minimal and transitory, but investigators must be aware of the potential for serious psychological harm. Breach of Confidentiality A breach of confidentiality is often the greatest risk to participants in social, behavioral & educational human subjects research. Reputations or employment may be damaged or jeopardized if confidentiality is not maintained. When possible disclosure of subject responses is the primary source of potential harm, collecting data anonymously may provide the best protection.
If, however, the study design makes the collection of identifiers necessary; for example a longitudinal study, safeguarding the data from unauthorized access can be accomplished in various ways, including: Removing all direct identifiers as soon as possible. Maintaining code lists and data files in separate secure locations. When research is conducted within the classroom setting and it is not anonymous, the PI/instructor should take steps to ensure that he/she is blinded to the identity of the participants at least until the grades are posted. It is recommended that the PI/investigator utilize a neutral third party or Honest Broker to verify document completion by each student, and to collect, store and de-identify questionnaires before delivering to the instructor/investigator.
The primary purpose of a Certificate of Confidentiality is to protect identifiable research information from compelled disclosure. Recruitment of Subjects Students have the right to be free from any coercion or bias that might result when a researcher is also evaluating them in a course. Therefore, the person recruiting the subjects should be someone other than an instructor of the students. This is to reduce any perception of coercion and to reduce the possibility of bias by the person evaluating the students resulting from knowing who is or isn t participating in the research project.
Obtaining Subjects Names Students have the right to privacy of personal information. The researcher may create a written form describing the kind of subjects being recruited and why, which can be: Distributed in class (it would be important for the researcher to be absent at the time of distribution to reduce any perception of coercion). Posted in a place where potential subjects will see it. Distributed via a class e-mail (students should be directed to respond to a third party or Honest Broker).
Research During Class Time Students have the right to have class time devoted to classroom activities appropriate to meeting the objectives for the scheduled course. If class time is to be used for research, the researcher must make a case to the IRB as to why the research is directly relevant to course content. A student can participate in the research activity without having his or her responses included in publishable data by withholding their consent or saying at the onset that their data may not be used.
How Can Coercion Be Avoided? Whenever possible, researchers should avoid involving their own students if another population of subjects is equally suited to the research question (e.g., another class section not taught by the researcher, recruitment by another instructor, or blinded/coded data collected by an associate so that subjects are not identified to the instructor). Students should be given an opportunity to decline participation without jeopardy. Unless the research question is directly related to class material, or the study process is being used as a teaching opportunity, such as in a research methods class, the use of class time to recruit subjects or class time used to complete study instruments is discouraged.
Complaints Student subjects must have access to reporting complaints regarding faculty when there are issues such as ethical concerns, coercion of student subjects, misguidance on research projects, or other issues that a student may find offensive or wrongful. Students can contact the appropriate department, the IRB office, the Office of Compliance, or the institution s ethics office to report and address their concerns.
Institutional Vulnerability Prospective subjects in research who are subject to the formal authority of others may have an institutional vulnerability. These individuals have the cognitive capacity to consent but may not be able to make a truly voluntary choice, and may be unduly influenced (or coerced) to participate when they otherwise might not have done so. Institutional vulnerability may arise when subjects are prisoners, enlistees in the military, employees, or college students when they are required to be research subjects for course credit or when such participation could affect their grades. In these situations, informed consent may be compromised because it is not truly voluntary. Further, these individuals may be subject to exploitation because of their subordinate status.
Investigators are required to file a COI disclosure prior to the submission of a protocol to the WMed IRB for review and are responsible for keeping these disclosures current. Additionally, investigators must comply with the WMed campus COI policies related to human subjects research, including disclosing potential conflicts of interest to the IRB and abiding by any management plans issued by the campus COI Committee (WMed Policy/Procedure Number GEN04, Conflicts of Interest and Commitment).
The FWA states that all human subjects research activities will be guided by the ethical principles outlined in the Belmont Report and that federally supported research activities comply with the Common rule. Investigators should become familiar with these principles and regulations to ensure that their research complies with them. Failure to comply with these principles can place both subjects and the institution at risk.
The federal Common Rule identifies six categories of human subjects research that may be eligible for exemption from IRB review. WMed IRB applies these six exemption categories only to studies determined to be no more than minimal risk and are not FDA-regulated. Human subjects research that qualifies as exempt under one of the federal categories must nonetheless satisfy WMed s standards for the protection of human research participants. If an investigator thinks his or her research falls into one of these exemption categories, he or she must still submit a protocol to an IRB. Only an IRB can determine whether the human subjects research is exempt. The IRB has the right not to exempt a protocol and to require full review by the convened IRB or expedited review by an IRB member, particularly if the research involves a sensitive population or sensitive topic.
Exempt Human Subjects Research If a study is determined to be exempt from IRB review, it is not subject to continuing review or other rules governing human research, such as rules on informed consent. However, the HHIPAA Privacy Rule applies to all exempt research that uses protected health information (PHI). HIPAA Privacy Rule requirements do not apply to exempt research using information that has been de-identified.
The Health Insurance Portability and Accountability Act Privacy Rule (HIPAA) is a federal law that generally prohibits health care providers (such as physicians or other health care practitioners, hospitals, nursing facilities and clinics) from using or disclosing protected health information (PHI) without written authorization from the patient. If an investigator intends to use or release to others (e.g., sponsors, other investigators, collaborators) any identifiable health information in connection with their research, that must indicated in the IRB application. All researchers who are part of WMed or an Affiliated Covered Entity (ACE) or collaborating with someone within the WMed or ACE and who are using or disclosing protected health information (PHI) must obtain written permission (i.e., an authorization) from subjects for the use of the PHI or must obtain a waiver or alteration of authorization from the IRB.
Prior to initiating a study, a PI must obtain written approval by the IRB to conduct human subjects research or a determination from the IRB that the study is exempt from IRB review. To be considered human subjects research , a project must meet both the federal definitions of research and human subjects. Research is defined under the Common Rule as a systematic investigation, including research development, testing and evaluation, designed to develop or contribute to generalizable knowledge. A Human Subject is defined under the Common Rule as a living individual about whom an investigator (whether professional or student) conducting research obtains: 1. Data through intervention or interaction with the individual. 2. Identifiable private information.
Research teams must adhere to the conditions of IRB approval, which includes the information provided in the IRB application and any supporting materials such as a formal study protocol. This means the research team should perform and/or distribute only the documents specified and approved by the IRB within the protocol.
If modifications to the IRB approved materials are necessary, a change of protocol must be submitted to and approved by the IRB prior to implementing the change. Failure to conduct the study according to the IRB-approved protocol is considered noncompliance. To change any aspect of a research study (no matter how minor the change may be), including revisions to an approved protocol, consent documents, recruitment materials, surveys/questionnaires, demographic pages, or HIPAA authorization forms, the changes must be submitted to the IRB for review and approval.
Federal regulations require IRBs to review and approve all research protocols at intervals appropriate to the degree of risk, but not less than once per year. As a courtesy, the IRB sends e-mail reminder notices to study teams, including PIs, prior to the expiration of approval date. However, investigators are responsible for monitoring their approval periods and submitting a Continuing Review Request Form for IRB review in a timely manner (i.e., within 30 days prior to the expiration date). If IRB approval of a protocol expires, research activities must cease until re-approval of the protocol is obtained unless the PI demonstrates that procedures are necessary to ensure subject safety.
When the research project is completed, investigators are expected to provide the WMed IRB with a Study Completion or Closure Form indicating that the protocol/project is closed.
Federal regulations and institutional policies require that investigators report to the IRB any unanticipated problems that pose risks to subjects or others that are related to the research. An unanticipated problem is a broad term that includes not only unfavorable outcomes that have occurred that were not expected, but also the development of potentially increased risks of harm occurring in the future. According to guidance developed by the Office for Human Research Protections (OHRP), an unanticipated problem is an incidence, experience, or outcome that meets all 3 of the following criteria:
1. The incidence, experience, or outcome is unexpected given the research procedures described in protocol-related documents (e.g., the study protocol, the consent documents) and the characteristics of the subject population being studied. An event may be considered unexpected if it exceeds the nature, severity, or frequency described in the study-related documents. 2. The incidence, experience, or outcome is related or probably related to participation in the research study. Probably related means the incidence, experience, or outcome is more likely than not to be caused by the research study procedures. 3. The occurrence of the incidence, experience, or outcome suggests that the research places subjects or others at a greater risk of harm (physical, psychological, economic, or social) than was previously known or recognized.
Federal regulations and institutional policies require that investigators report noncompliance with IRB approved documents or research regulations to the IRB. Noncompliance means any failure to follow: 1. Federal regulations, state laws or institutional policies relevant to human subjects research. 2. The requirements and determinations of the reviewing IRB.
State and federal regulations require study teams to maintain complete and accurate study records. Study records should be stored in a secure manner to protect the privacy of subjects and to reduce the risk of damage. Any or all of the study-related documents may be subject to, and should be available for, audit or inspection by a regulatory authority. Study records can be archived after completion, but must be maintained for a specified amount of time, depending on the requirements of the funding agency, sponsor, FDA or entity providing oversight. There may be other requirements that researchers must look into before disposing of research records.
Many clinical research studies involving human subjects must be registered on and have results posted to ClinicalTrials.gov as mandated by the Food and Drug Administration (FDA) and/or International Committee of Medical Journal Editors (ICMJE). The ICMJE requires registration of any interventional health outcome studies including Phase I trials - prior to subject enrollment. Failing to register trials covered by the ICMJE requirements in a timely manner can result in the rejection of publications based on the failure to register the trial.
When IRB review of a study is deferred to a non-WMed IRB, the PI and study team must still comply with relevant WMed IRB requirements and must also be familiar with the requirements of the IRB of record, which may differ from that required by WMed. These responsibilities include complying with the requirements of the reviewing IRB in addition to those of the PI s own institution and ensuring all institutional requirements are met. When WMed serves as the coordinating center for a study, some of the additional requirements the PI and study team are responsible for include: ensuring IRB approvals from all sites are in place before human subjects research occurs at those sites and promptly communicating protocol changes, new information, and unanticipated problems to all study sites and ensuring that any changes are implemented.
University of Wisconsin-Madison http://www.irb.wisc.edu/documents/Principal_Investigator_Responsibilities.pdf Galvez, Jackie, Susan L. Rose, Jennifer Hagemann, and Monica Aburto. Original module was authored by Cho, Maristela and Susan L. Rose. 2017 Students in Research CITI Program http://www.citiprogram.org O Donoghue, Kelley, 2012 Non-Compliance University of Rochester https://www.rochester.edu/ohsp/documents/education/pdf/seminarMaterials/Non_Compliance_ 18Sept12.pdf