Comprehensive Overview of Acute Kidney Injury
Definition, implications, epidemiology, risk factors, diagnosis, and management of Acute Kidney Injury (AKI). Understand the stages, causes, diagnostic tests, and key principles in treating patients with AKI. Learn about who is at risk and the high morbidity associated with this condition.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Internal Medicine Academic Half Day Acute Kidney Injury Asad Merchant M.D. FRCP (C)
Disclosure None 3/16/2025
Objectives Understand the definition, implications, epidemiology, and risk factors of Acute Kidney Injury (AKI) Develop an approach to the diagnosis of the cause of AKI (case based) Appreciate the diagnostic tests available Understand the principles of management of a patient with AKI
A K I 3 letters that ll make your attending cry! Prophetic rap verse from a nephrology fellow who shall remain unnamed 3/16/2025
Acute Kidney Injury Very common High morbidity and mortality in hospitalized patients Increases risk of CKD, mortality
Definition KDIGO 1, 2, 3 AKIN 1, RIFLE Time line
Definition of AKI A1: AKI is defined as any of the following (not graded): Increase in SCr by 0.3 mg/dl ( 26.5 mol/l) within 48 hours; or Increase in SCr to 1.5 times baseline, which is known or presumed to have occurred within the prior 7 days; or Urine volume <0.5 ml/kg/hour for 6 hours. Kellum, John A, and Norbert Lameire. Diagnosis, Evaluation, and Management of Acute Kidney Injury: A KDIGO Summary (Part 1). Critical Care 17.1 (2013): 204. PMC. Web. 2 Oct. 2018.
Stages of AKI KDIGO AKI Work Group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012;17:1 138.
Who gets it Elderly CKD Vasculopaths DMII Chronic Diseases Liver, CHF, CAD Deconditioned/ malnutritioned On potential nephrotoxins Hsu, Chien-Ning et al. Incidence, Outcomes, and Risk Factors of Community-Acquired and Hospital-Acquired Acute Kidney Injury: A Retrospective Cohort Study. Ed. Frank Liu. Medicine 95.19 (2016): e3674. PMC. Web. 2 Oct. 2018.
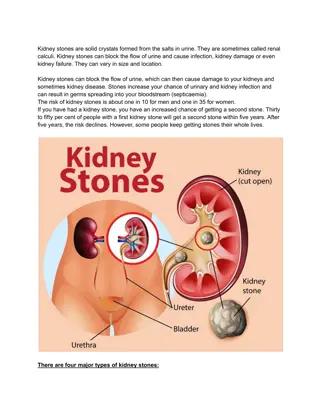
Approach to AKI Decreased GFR or decreased Urine output Pre renal Intra renal Post renal . . . . . . . . .
Tests, monitoring and management Urinalysis Urine lytes, osm Foley rule in obstruction Urine output Ultrasound of kidneys rule out obstruction
Case 1 Tis the season 68 year old man with COPD, HTN, BPH and DMII On Metformin, Perindopril, Indapimide and Spiriva Presents with SOB, fever, cough, rhinorhhea No flu shot! BP 96/50, requiring 4L O2, WOB increased Hb 95, WBC 11.3, Na 131, K 5.5, Cr 180, lactate 6, bicarbonate - 20 Deteriorates in ER, intubated and taken to ICU
Next steps? AKI differential diagnosis? Investigations: Foley Urinalysis Urine lytes Ultrasound kidneys Management?
No U/O with foley catheter insertion Urine Osm 350 Urine Na 95 mmol/L Urine K 26 mmol/L Urine Cl 46 mmol/L Urine Cr 7 mmol/L FENa = 1.8%
Acute Tubular Necrosis Receives fluids and antibiotics Metformin, ACEi, diuretic held Low K+ diet Oxygen and ventilation requirements worsen Still oliguric/ anuric creatinine 350 K+ = 6.2 What next?
Furosemide For volume overload, and hyperkalemia Need higher dose in renal failure Furosemide stress test a prognostic risk stratification tool 1 mg/kg dose (1.5mg/kg if lasix non na ve) High spec and sens (>80%) if u/o < 200ml/ 2hr Chawla, Lakhmir S et al. Development and Standardization of a Furosemide Stress Test to Predict the Severity of Acute Kidney Injury. Critical Care 17.5 (2013): R207. PMC. Web. 2 Oct. 2018.
When to dialyze ? Acid base status refractory to medical mgmt Electrolytes (K+) same as above Intoxications (poisons) Overload Uremia Pericarditis/ Encephalopathy Anticipatory If anuric then get central access earlier
Early vs Late dialysis Controversy in Critical care Nephrology 2 major trials (AKIKI and ELAIN) had somewhat differing outcomes regarding benefit from early initiation. At this point, no good evidence from early initiation of dialysis beyond clinical signs Canada STARRT AKI trial results pending Gaudry S, Hajage D, et al. Initiation strategies for renal- replacement therapy in the intensive care unit. N Engl J Med. 2016; 375(2):122-33. Zarbock A, et al. Effect of early vs delayed initiation of renal replacement therapy on mortality in critically ill patients with acute kidney injury: the ELAIN randomized clinical trial. JAMA. 2016; 315(20):2190 9. 3/16/2025
Resolution Furosemide 160mg iv given Urine output 50 100cc/hr Started on standing dose of furosemide Metolazone added for synergy Creatinine improves, K+ < 5 Eventually begins passing 2 4 L/ day Post ATN diuresis - diuretics stopped
Case 2 Rock and Hard Place CAD, DMII, CKD, CHF Ischemic CMP On ASA, Bisoprolol, Telmisartan, lasix 80 po bid, Insulin O/E: BP 88 systolic, JVP 6cm ASA, crackles b/l midway up lung, pitting ankle edema Creatinine 275 uM 2 weeks ago 130 uM Urine output 20cc/hr Urine bland, urine lytes low Na, K, Urine osm 470
What is the problem Nohria A, Lewis E, Stevenson LW. Medical management of advanced heart failure. JAMA 2002;287:628 40. 3/16/2025
Lasix high dose He starts urinating loses 1 kg/ day BP starts to improve Creatinine starts to improve Is it magic? Nope Cardio Renal Syndrome Type 1 Goes home with creatinine of 140
Pathophysiology Claudio Ronco et al. JACC 2012;60:1031-1042 American College of Cardiology Foundation
Case 2 continued 1 month later, back at the general BP 80, creatinine 300 Ok, lets do this all over Lasix high dose creatinine 400, BP 70 systolic Oh Oh!
CCU to the rescue Goes to the CCU Gets started on nitrates, inotropes Improved cardiac output, decreased activation of the neurohormonal axis Improved creatinine and diuresis Fix the heart, fix the kidney Patient goes home with a creatinine of 150
Case 3 72 year male ++ alcohol, smoking, obese, diabetic Presented with abdominal distension, peripheral edema, nausea U/S showed cirrhosis and ascites AST > ALT (2x), GGT high Admitted to hospital for w/u, and diuresis (lasix, spironolactone Day 2 had increased pain, and fever
Spontaneous Bacterial Peritonitis Became mildly encephalopathic, started on lactulose Day 3: creatinine 82 146 Hepato Renal Syndrome
Hepatorenal Syndrome Hepatorenal Syndrome - Scientific Figure on ResearchGate. Available from: https://www.researchgate.net/Pathophysiology-of-hepatorenal-syndrome-a- the-development-of-splanchnic-vasodilatation_fig1_266909007 [accessed 2 Oct, 2018]
Hepatorenal Syndrome Kiser, Tyree. (2014). Hepatorenal Syndrome. International Journal of Clinical Medicine. 5. 102-110. 10.4236/ijcm.2014.53018.
Treatment Treat EARLY extent of creatinine rise influences chance of reversal Treat precipitating cause Stop diuretics Volume expansion with Albumin Also has ligand and inflammatory mediator binding properties Vasoconstrictors Levophed Terlipressin specific portal circulation vasoconstrictor Midodrine/ Octreotide Sanyal, A. J. et al. Reversal of Hepatorenal Syndrome Type 1 with Terlipressin plus Albumin vs. Placebo plus Albumin in a Pooled Analysis of the OT 0401 and REVERSE Randomised Clinical Studies. Alimentary Pharmacology & Therapeutics 45.11 (2017): 1390 1402. PMC. Web. 2 Oct. 2018.
Transjugular Intrahepatic Portosystemic Stent Shunt (TIPS) Dialysis Only as a bridging therapy Liver transplant reversible AKI in ~ 83% LKTx Consider if pt on dialysis 8 12 weeks Wait and see Utako, Piyapon et al. Clinical Outcomes after Liver Transplantation for Hepatorenal Syndrome: A Systematic Review and Meta-Analysis. BioMed Research International 2018 (2018): 5362810. PMC. Web. 2 Oct. 2018.
Case 4 Blood and Sweat 27 year old male presents with malaise, fever, nausea, rash, abdominal pain, swelling in feet In ER, BP 180/95, chest clear, peripheral edema BW Hb 89, WBC 14, PLT 166 Creat 450 Na 128, K 4.5 U/O over 24hrs 750cc
Anything else on history? Sexual, infectious, travel, drugs, family history, other constitutional/ autoimmune symptoms Investigations? Management?
Urinalysis Urinalysis 3+ blood, 3+ Protein
Microscopy 3/16/2025
What tests to order Urineprotein, Urine Albumin/Creatinine Ratio Autoimmune panel ANA, Complement, ENA Infectious panel Blood Cx, hepatitis serology, HIV, syphillis, parvovirus B19 Rheum Factor, cryoglobulin, immunoglobulins ANCAs, anti GBM serology SPEP, serum free light chains Malignancy screen (age appropriate) Don t forget to rule out renal vein thrombosis
Diagnosis Rapidly Progressive Glomerulonephrtis (RPGN) Cause?
Approach to GN Lots of ways to break it down Best way to begin is by urinalysis and pathophysiology intersect Proliferative hematuria with dysmorphia and cast formation vs non proliferative bland sediment After that, different people have different approaches Best to keep it simple, important thing is not to miss the dangerous pathological entities Having an approach helps to ensure you order the right test, and hopefully be judicious in your tests
Nephrotic range proteinuria Edema Hypoalbuminemia Glomerular hematuria AKI HTN sub nephrotic proteinuria Clinical Syndrome(Nephrotic vs Nephritic) Proliferative Non- Proliferative Minimal Change Disease Primary Secondary Henoch Schonlien Purpura Membranous Nephropathy IgA Nephropathy Vasculitis - ANCA Vasculitis - ANCA Good Pastures Syndrome FSGS Anti GBM disease Cryoglobulinemia Hep C/ Hep B/ HIV Amyloidosis C3 Glomerulopathy Post-Infectious (e.g. Endocarditis/ Shunt) Secondary Alport s Lupus Nephritis DMII/ I Fibrillary/ Immunotactoid Myeloma Fabry s Disease * CKD 4/ 5 eg. HTN
Glomerular hematuria AKI HTN sub nephrotic proteinuria Clinical Syndrome(Nephrotic vs Nephritic) Proliferative Primary Secondary Henoch Schonlien Purpura IgA Nephropathy Vasculitis - ANCA Vasculitis - ANCA Good Pastures Syndrome Anti GBM disease Cryoglobulinemia Hep C/ Hep B/ HIV C3 Glomerulopathy Post-Infectious (e.g. Endocarditis/ Shunt) Alport s Lupus Nephritis Fibrillary/ Immunotactoid Myeloma Fabry s Disease
Viral serology: ANA: Complements: RF: Cryogulobulin: Protein Electrophoresis: Immunoglobulin panel: pANCA: cANCA: GBM:
Viral serology: Negative ANA: Negative Complements: Normal RF: Negative Cryoglobulin: Negative Protein Electrophoresis: Normal Immunoglobulin panel: Normal pANCA - >8 cANCA: Negative GBM: Negative
Biopsy? Diagnosis Prognosis If it will impact management Risks Bleeding! Contraindicated in patients with coagulopathy, anticoagulation, HTN, ESRD, infection overlying site
Necrotizing Crescentic Glomerulonephritis Bilal Musharaf. Glomerular Diasease and role of immunofluorescence in diagnosis. https://www.slideshare.net/bilalbanday/glomerular-diseases/12 Accessed Oct 2, 2018
Microscopic Polyangitis Start with steroids Pulse with 1g iv x 3 days followed by 1mg/kg of prednisone daily Steroid sparing immunosuppresion Cyclophosphamide alkylating agent Rituximab Plasmapheresis? Trial pending Stone, J et al. Rituximab vs Cyclophosphomide for AAV. N Engl J Med 2010; 363:221-232 Walsh, Michael et al. Plasma Exchange and Glucocorticoid Dosing in the Treatment of Anti- Neutrophil Cytoplasm Antibody Associated Vasculitis (PEXIVAS): Protocol for a Randomized Controlled Trial. Trials 14 (2013): 73. PMC. Web. 2 Oct. 2018.