Coventry and Warwickshire
Framework focusing on Clinical and Care Professional Leadership in Coventry and Warwickshire, emphasizing elements like shared learning, quality, safety, governance, networking, communication, and leadership development to enhance healthcare services.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Coventry and Warwickshire Clinical and Care Professional Leadership Framework
Coventry and Warwickshire ICS Coventry and Warwickshire ICS Local Authorities: 2 District and Borough Councils: 4 Acute Trusts: 4 Primary Care Networks: 19 Places: 4 (Coventry, Warwickshire North, Rugby and South Warwickshire) Population: Estimate 950,000, growth steeper in Coventry 18.8% (2009-2019) Warks 8% same time period Finance: 1.8 Billion in Public Funds, 4% efficiency ask, committed 90m in Capital Total Workforce: 47,526 NHS Providers 20,690 Adult Social Care 23,500 Primary Care 2939 CCG 397 Total Vacancies: 1384
Clinical and Care Professional Leadership Framework Clinical and Care Professional Leadership Framework Leadership Development Philosophy of Care Our Clinical and Care Professional Framework is built on seven elements. 1. 2. 3. 4. 5. 6. 7. Philosophy of Care Shared Learning Quality and Safety Clinical Governance Clinical Networking Comms and Engagement Leadership Development Comms and Engagement Shared Learning Each element has interdependencies across various workstreams and is dependent upon specialist input from across the system. Clinical Networking Quality and Safety It responds to the ICS strategic aims and priorities as well as encompassing the five principles of CCPL at its core. Clinical Governance
Framework Elements Framework Elements Clinical and Care Professional Networking: A strong clinical and care network ensures that all ICS members are included, heard, and represented. It is intrinsic to strengthening all other elements of the framework. Philosophy of Care: A system Philosophy of Care that will support decision making regarding all future service change. Shared Learning and Collaboration: Joint working is vital for system development and productivity. We build on what is already in place, review, and implement best practice. Comms and Engagement: Communication is key to gaining increased input from all levels of the system. The sharing of knowledge ensures that all decisions are made are informed. Engagement ensures the inclusion and representation of ICS members as well as continuing the principle of co-design. Quality and Safety: The link between CCPL and Quality is key. We have set this in our designs especially for Governance and Shared Learning. Leadership Development: Leadership development is the core of Clinical and Care Professional Leadership. Developing, nurturing, and growing your own talent gives increased opportunity to ICS members, improving job retention and in turn retaining the knowledge and relationships already existing within the system. Investing in our staff is vital to our system and will be supported by initiatives such as talent spotting, mentorship, and development programmes. Governance: Clinical and Care Professional governance enforces strong structural designs. Ensuring that the position within the ICS is correct and widely known is crucial for interaction, assurance, and accountability.
Our approach to Clinical and Care Professional Leadership Our system strongly believes that Clinical and Care Professional Leadership (CCPL) needs to be a core foundation of the system and how we act, engage, and make decisions in the future. Due to its multidimensional nature, it is critical to involve and strengthen the relationship between various workstreams. Though not limited to, early indicators identified the following: 1. Digital and Business Intelligence Data-driven/evidence-based decisions. 2. Governance Data sharing, decision making and embedding CCPL across the system. 3. People and Organisational Development Mentorship and inequalities. 4. Comms and Engagement Engagement around clinical priorities with a particular focus on patient outcome. 5. Quality and Safety System leadership behaviours in place to ensure this is paramount and robust processes well embedded with all clinical and care professionals With the complexity of this work and the required Readiness to Operate Statement (RoS) activities, our approach focuses on designing and working to a framework. The framework consists of areas to develop (including the must do s), how we will build these, and the evidence that we will provide NHSE/I aligned to each activity. The framework has a series of initial documents that need to be produced; many of these are new for the system and, as such, will not be complete by July 22. Instead, all documentation will be marked as evolutionary , meaning that these will continue to expand post-July. For us, the ICS Transition isn t just about ticking boxes but creating meaningful plans for the system that are created with full input and are agreed upon and owned by all system partners.
The Five Principles of Clinical and Care Professional Leadership 1. Integrating clinical and care professionals in decision making at every level of the ICS 2. Creating a culture of shared learning, collaboration and innovation, working alongside patients and local communities The Five Principles of Clinical and Care Professional Leadership 3. Ensuring clinical and care professional leaders have appropriate resources to carry out their system role(s) 4. Providing dedicated leadership development for all clinical and care professional leaders 5. Identifying, recruiting and creating a pipeline of clinical and care professional leaders
1. Integrating clinical and care professionals in decision making at every level of the ICS How is this defined: Ensure that the full range of clinical and professional leaders from diverse backgrounds are integrated into system decision-making at all levels, supporting this with a flow of communications and opportunities for dialogue. What this means to us and why are we doing it? Ensure that all voices and perspectives are values and contribute to all levels of decision making to support transformation and shared learning to reflect the breadth of our workforce. An inclusive leadership will strengthen outcomes. We do this because we champion equality and value diversity. When we exclude we limit our possibilities. How we demonstrate it: We started by designing and implementing a Clinical Executive Group (CEG). Membership was an important consideration and was designed to ensure a wide range of representation. Members of the CEG bring representation of expertise/profession but not the representative of that group of any organisation. As voting board members, the CMO and CNO will be the voices to represent into the ICS Executive Group and the ICB. Members of the CEG flow communications through their professional groupings e.g. AHPs, along with flows through organisations and places. Using EDI champions and asking ourselves open questions about the diversity of representation and styles of communication (valuing neurodiversity for example) is embedded in this work. Committed to the establishment of place based clinical forums as place development progresses, as well as working with the Geographical Care Collaboratives to co-design clinical requirements. Use of staff and professional teaching and forums at organisation. Multi professional EAG pathways based, professional networks for best practice and learning. Design and commence planning/scheduling of quarterly system wide inclusive forums/Town halls events. These will utilise online functions to facilitate maximum involvement. Work with the Digital Transformation Board and Communications & Engagement to explore a Teams platform/web based forum for all interested staff to share information and scope ideas. Design a Clinical and Care Professional Leadership Development workstream which will include mentorship and development of future leaders with a key focus on improving and expanding upon equality, equity, and diversity of our workforce to reflect the population we serve.
2. Creating a culture of shared learning, collaboration and innovation, working alongside patients and local communities How is this defined: Nurture a culture that systematically embraces shared learning, supporting clinical and care professional leaders to collaborate and innovate with a wide range of partners, including patients and local communities. What this means to us and why are we doing it? Culture of developing improvement ideas from the those closest to the delivery of health and care. Valuing all staff, patient experience and public perception and wanting to learn and change in an open culture. National evidence shows this is essential for safety, care and transformation. How we demonstrate it: The culture for this exists and will continue to be promoted through ICS, provider organisations, LA, PCNs and the community and voluntary sector. Clinical leaders continue to meet with university leads to develop innovation through formal research and new ground up projects including mental health collaborative working. Utilising the improvement methodologies embedded within organisations across the system e.g. QSIR and UHCWi (partnership with Virginia mason). Continue to develop relationships with sectors outside of health and care to support innovative thinking. Partnering with our Local Authorities to share Community Champions in our system are a voice reflecting their community experiences and add regular robust and honest challenge to existing and developing work (Improving Lives of Older People recent even as latest example)
3. Ensuring clinical and care professional leaders have appropriate resources to carry out their system role(s) How is this defined: Support clinical and care professional leaders throughout the system to be involved and invested in ICS planning and delivery, with appropriate protected time, support and infrastructure to carry out this work. What this means to us and why are we doing it? All levels ethos exists for inclusive board to ward approach and ability. Allocation of time to enable successful delivery on clinical strategy. Diverse clinical and care professional leadership team supporting decision making across the ICS. System goals and principles embedded and enacted at all levels and a culture of shared accountability and positive achievement in delivery of our objectives. Because we want a workforce that understands Stewardship of shared system resources and has the time and support infrastructure to develop and deliver our ICS plan. How we demonstrate it: ICB support sought from NEMs and trust NEDs to take real pulse checks of staff on walk rounds as well as staff surveys and act on findings. We have agreed to make a commitment to ensuring that Clinical and Care Professionals are appropriately resourced and supported to carry out their system roles. We are in the process of reviewing resource allocation with the intention to present a resource model, and subsequent financial requirements, to the ICS Executive. We are reviewing our current, and potentially required, ICS Lead posts. With our system we have roles such as an ICS Chief Pharmacist and ICS Chief AHP, Healthcare Scientist Lead etc. We will be evaluating how we continue these posts, if any additional leads are required, where and how these are funded etc. We will look to bring together/share and build on nursing directorate and medical directorate at ICS and blur old boundaries. This is strengthened by the collaboration between the CCPL and Quality workstreams, the CMO and CNO being CEG members, and the governance links between the committees and groups. It is recognised that clinical practitioners in some settings have paid time for engagement, research etc. but not in others (e.g. GP, Community Pharmacy, lower grade hospital staff etc.). As with many other ICS s, we will undertake a benchmarking approaches to employment and pay for clinical and care professional leaders exercise. The will look at multiple elements such as, employment models, approach to rates of pay, definition of sessional lengths etc. Detailed further on slides 35-37
4. Providing dedicated leadership development for all clinical and care professional leaders How is this defined: Create a support offer for clinical and care professional leaders at all levels of the system, one which enables them to learn and develop alongside nonclinical leaders (e.g. managers and other non-clinical professionals in local government and the VCSE sector), and provides training and development opportunities that recognise the different kind of leadership skills required when working effectively across organisational and professional boundaries and at the different levels of the system (particularly at place). What this means to us and why are we doing it? Ensuring an equity of access to education and development for all irrespective of speciality, skillset, background, and level within the system. At its simplest this is built on communities, PCN, Place, Provider and System levels of support and education. We want a workforce that finds joy and satisfaction and onward challenge to benefit patients and grow a thriving workforce. How we demonstrate it: Embedded in the Virginia Mason work, availability of Masters, NHS leadership courses (Nye Bevan etc) through ICS and organisations. Development of joint teaching and education e.g., GPs inputting into system Physician Associate and FCP teaching and less formal communities of practice with more formal shared learning at organisational medical and nursing teaching. PLT for GPs to continue with secondary, community and voluntary sector input in agenda shaping and delivery of education and listening exercises. CCG team of educational leads to transfer into the ICS and consideration of the brief widening from Primary Care education to system wide being considered. Full use is made of HEE support and schemes for fellowships and mentoring as well as the NHS Elect offer and other training and action learning sets at Place and for PHM (cross organisational). Explore cross sector working. Continue to develop reverse and peer mentoring work with EDI team. We are keen to explore leadership training based on system values and local and national definitions of system leadership and CMO has committed to developing supportive learning around Stewardship and Compassionate Leadership. CCPL team work closely with People Directorate to co-develop strategy for integrated recruitment and retention with support offer being vital to this.
5. Identifying, recruiting and creating a pipeline of clinical and care professional leaders How is this defined: Adopt a transparent approach to identifying and recruiting leaders which promotes equity of opportunity and creates a professionally and demographically diverse talent pipeline that reflects the community served and ensures that appointments are based on ability and skillset to perform the intended function. What this means to us and why are we doing it? Work with universities to ensure pipeline of health and care workers. Look to recruit to recruit from local communities working to embed our self as anchor organisations and PCNs that value local sustainable growth. How we demonstrate it: Championed by the ICS Chair and organisational Chairs through ICS, Place and Organisation. Staff surveys, touch points to understand our level of inclusion to constantly shape and modify all we have in place. Equity of opportunity: An organisation that seeks to understand what it is like to work and belong here using narrative as well as metrics. Staff forums and Place based Clinical Forum to be used to identify and develop local leaders. Continuation of Fellowship programmes. Recruitment practices: Commitment to follow innovative interview processes that recognise our unconscious bias and do not skew recruitment (q in advance, diverse panels, more junior posts having input in interview process/panels). Use of universities locally to identify talent needed to perform functions with appropriate skillset and ability to continue our collaborative approach to developing undergraduate and post graduate programs health and care programs with Coventry University to ensure our local workforce is correctly skilled. Work with Coventry University to input into training to create the correctly skilled workforce. Universities are actively driving work to bring more diverse students onto programs which we will support and learn from.
Philosophy of Care Philosophy of Care Due to the ever-changing nature of clinical and care priorities and pressures, a definitive clinical strategy cannot easily be put down on paper at this stage and the system recognises this is an evolutionary process. A clinical strategy was developed in 2018 by harnessing the knowledge from within our system and working in partnership with other professionals across health and social care. It was widely consulted with engagement undertaken and views sought from our patients, the public, our partners, and our staff, including a clinical summit for Coventry and Warwickshire. Whilst acknowledged that it would be an iterative document, the clinical strategy set out the core foundations of how the system would work clinically and ensure that decisions are made on a clinical basis with the patients needs at the forefront. The previous clinical strategy was intended to act as a mechanism to ensure that Coventry and Warwickshire system- wide transformational programmes focused on proposals that provide the best fit with the principles set out on the following slide. It is acknowledged that as we transition a new team may be the catalyst for taking this forward. To cover the interim transition period, we agreed a principle that is at the core of our ICS: "We will work together for our population prioritising care over individual organisations." The framework provides a guide for the new team to build upon. Post-transition, and when the time is right, the previous clinical strategy, principles for planning, redesigning and making decisions about future Service Change (following slide), and the Philosophy of Care will be developed into a refreshed ICS Clinical Strategy. The individual aspects detailed throughout this presentation will contribute to the refresh and redesign of an ICS Clinical Strategy. Clinical and Care Professional Leadership will be a fundamental part of the new strategy as we change our thinking, ways of working, and collaboration across the system.
Previous principles for planning, redesigning and making decisions about future Service Change Previous principles for planning, redesigning and making decisions about future Service Change Ensures there is robust evidence underpinning both the clinical case for change and the proposed clinical model (e.g. RightCare and NICE guidance). Focuses on prevention activities, keeping people well, reducing demand and pressure within the system. Takes a Person-Centred Approach. Provides affordable solutions to utilise available funding as effectively as possible. Ensures services are integrated between primary and secondary care. Ensures care is provided closer to home wherever possible. Ensures that variation across the Coventry and Warwickshire system is minimised and does not impact upon equity of access to services. Ensures services are sustainable, efficient, and adaptable over time. Ensures services are safe through a systematic approach to maintaining and improving the quality of patient care across the Coventry and Warwickshire health and care system.
Shared Learning and Collaboration Shared Learning and Collaboration Shared learning and collaboration should be habitual and natural within the system to ensure the best possible outcomes and care for our citizens. Within our system we have a strong nature of sharing learning and collaborating across professions, organisations, place, and even neighbouring ICSs. In line with various other elements of the framework we aim to build on the good that is in place and continually improve this synergetic way of working. Examples: Coventry and Warwickshire Local Authorities are part of a West Midlands wide 3 year evaluation of strength-based practice with the University of Birmingham. This evaluation supported by the Adults Principal Social Worker (PSW) Network will seek to learn from the different models and approaches taken by local authorities to embed strengths-based practice. This will support local authorities to better understand how they can approach such transformation and increase the likelihood of sustainable implementation within their local context. This full evaluation is being undertaken been 2020 and 2023. COVID-19 brought challenges to all, not least of all the health and social care providers across the country. All care providers had to manage challenges most had never experienced before. Care providers across the city demonstrated amazing resilience and commitment to the people they support during the pandemic. Staff had to make significant changes within their day-to-day practices at work as well as in their personal life. The Joint Coventry City Council and Coventry and Warwickshire Clinical Commissioning Group (CRCCG) Quality Assurance Team, adapted their working practices in line with government guidance and provided an extensive range of support to providers across the city in response to changing government guidance on how to manage COVID-19, from Personal Protective Equipment (PPE), self isolation and care home admissions. The CRCCG use a range of quality improvement campaigns, which are central to contract and quality assurance activities for the people of Coventry. The quality improvement campaigns look to ensure good care outcomes for commissioned services. Unfortunately, due to the COVID-19 pandemic all campaigns were put on hold and these will be recommenced as soon as possible. These programmes have included React to Red a joint health and social care awareness and educational campaign and accreditation scheme that was launched in 2014 across the care market in Coventry. The campaign is designed to increase education to help prevent avoidable pressure ulcers. Falls are one of the top three reasons for hospital admissions for people over 65 and can result in some severe injuries or disabilities. These can be frightening, affecting a person s confidence in their mobility. The React to Falls campaign was launched in January 2020. The campaign includes free training, tools and educational materials and local care providers will be able to gain accreditation. Local Maternity and Neonatal Service (LMNS) - The Coventry and Warwickshire LMNS Board has been established to provide oversight to the quality and safety of maternity and neonatal services, and oversee the delivery of transformation and continuous improvement to make maternity and neonatal care safer, more personalised and clearly designed. The Board takes a system-wide approach to service improvement and transformation (as reflected in a LMNS plan) involving service users and local communities, as well as relevant senior clinicians, commissioners, operational managers and primary care. This will involve shared clinical and operational governance, the co-production of care pathways, a clinically and financially sustainable model of care for maternity and neonatal services, as well as policies, procedures, guidelines and protocols, across the LMNS. Mortality Oversight Group (MOG) -The Coventry and Warwickshire MOG is a system-wide oversight group which brings together partners from across the health and social care economy to monitor mortality trends, evaluate learning, look at best practice thus informing commissioners regarding improvements in patient care in order to prevent avoidable deaths and reduce premature mortality. Learning from mortality is used to drive service improvement and offer assurance to our patients, stakeholders and Boards that the causes and contributory factors of patient deaths are jointly considered and appropriately responded to in an open and transparent manner. The MOG s county-wide approach to learning from death has been established with the aim of ensuring a standardised high quality, consistent reviews, and enable a robust process for escalation, dissemination and implementation of learning.
Shared Learning and Collaboration Shared Learning and Collaboration Getting to Outstanding (End of Life Care) The Coventry and Warwickshire system is linked to the Getting to Outstanding programme to support development of the system strategic intention to offer safe, high quality and personalised end of life and palliative care to our population. To date the leadership and governance structures have been established, stakeholder analysis completed and engagement plan in progress. The draft strategic plan timeline is October 2022, and a lived experience reference group will be established to inform the plan. Hospices continue to lead their development as a group locally, supported by facilitation of the Local Government Association (LGA), and an action plan created and monitored. A system Memorandum of Understanding has been agreed between Hospices Working Together to work towards a single point of access for palliative and end of life care services. Emergency response collaboration: The importance of open, efficient, and adaptive collaboration is most prevalent when an emergency response is required. Emergency responses are good examples of where the system works collectively, irrespective of organisational boundaries, and provides a rapid response to a critical situation. These are usually time critical and pressured situations whereby the system demonstrates its ability to collaborate and colleagues willing to go above and beyond. Examples: Dermatology: Quality concern raised about practices at a local centre regarding an particular area of skin cancer management. Trust Quality process followed and widened to include system partners as part of a thorough review of practice including engagement of national experts and Royal society of Dermatologists who advised on the scope of the investigation and audit and provided independent advice and reporting. This was overseen by the Trust CMO but in regular collaboration with CCG Chair, CCG CNO, System Quality Group and CMOs from our ICS. Pharmacy Vaccine: Pharmacist leaders had been meeting regularly since mid 2019 as part of the Integrated Pharmacy and Medicines Optimisation Board. This meeting became enormously valuable during the pandemic but particularly around the vaccine programme. UHCW gave the worlds first vaccine and was able to share learning and training tools e.g. bespoke videos to support the mass vaccination centres, with significant mutual support during a fast paced programme of work that was delivered across all sectors of the profession. Pharmacy CMDU: December 2021 there was an ask for systems to implement covid treatments for community patients within the acute sector in a 10 day window. Existing pharmacy leadership relationships supported working at such a pace. The model developed rapidly into a secondary care/primary care model working with pharmacy, secondary care consultants and GPs to deliver by a true hybrid model. This model is seen as an exemplar in the way GPs, secondary care consultants and pharmacy provide novel medicines to high risk patients.
Quality and Safety Quality and Safety Quality and safety are intrinsic to all that the Clinical and Care Professional Leadership programme does. From a governance perspective there are clear lines between the Clinical Forum into the System Quality Group and Safeguarding. All members of the Clinical Executive Group such as the CNO and Principle Social Worker etc. have a clear focus on quality and safety that will be shared collectively at the board. This allows quality and safety to be discussed from different perspectives as well as providing a link back to their professional infrastructures. Examples: Coventry and Warwickshire both have effective multi-agency processes in place to identify potential Safeguarding Adult Reviews and Serious Case Reviews for children. Membership is drawn from a very wide range of agencies with social care, police, voluntary sector, probation, education and the full range of NHS provider and commissioning organisations. This wide range of professionals expertise is used to consider referrals and contribute to formal reviews. The process is genuinely collaborative, open and honest with sound analysis which identifies good practice and lessons to be learnt. Key information is then communicated across all agencies through case summaries, briefings and learning events. Coventry and Warwickshire Local Authorities are part of a West Midlands wide approach to practice reviews and practice quality assurance. Two Principal Social Workers from other authorities spend two days in the host authority undertaking the practice review, this practice review focus on strength-based practice approaches and the practice conditions in place to support the application in practice. Due to COVID-19, the Peer Challenge Process re-focused to a Pause and Learn approach and Practice Reviews also incorporated learning from the pandemic. In total 29 reviews have been held over the course of the last 5 years. These reviews have been integrated into the Local Authority Peer Challenge process (Weblink ) Leave no doubt empowering your life choices Following the outcome of a learning event from a complex case, a number of areas of concern were raised along with particular areas of development for the CCG with regards to the topic areas: Mental capacity. Advanced decision to refuse treatment (ARDT). Clinically assisted nutrition and hydration (CANAH) decision. Lasting power of attorney for health. Advanced Decision to Refuse Treatment (ADRT) and Lasting Power of Attorney (LPA) were discussed at the CCG Clinical Executive Group and recommendations from this group were to detail how we as a CCG, can raise awareness of this very important area with our patients, public, stakeholders and clinicians with an aim to enable and normalise conversations surrounding the above areas. It was noted that more patient and primary care education and awareness raising was needed to ensure that patients are aware of the importance of such discussions should they suddenly be taken ill, injured or need end of life care in the future and/or a decision needed to be made on their behalf of future of treatments. A Coventry and Warwickshire wide bus campaign covered various geographical areas on 30 bus rears, along with digital content and staff messaging; all campaign materials were created in partnership with the complaints team, patients, clinical leads and a national charity (Compassion in Dying). System review of unexpected perinatal patient death A system-wide review of the care and treatment provided for a perinatal patient prior to her unexpected death was commissioned with the aim to identify any cross-system learning and actions required to help prevent similar incidents occurring in the future. A multidisciplinary panel was convened to review documents provided by those services involved in the patient s pathway, and meet with the patient s partner. The final report has been tabled at the Local Maternity and Neonatal System (LMNS) Board to implement the recommendations and monitor actions. In addition, the patient s partner has shared his story/experience of local healthcare services across the pathway to support system learning
Clinical Executive Group Clinical Executive Group ICS Structure: The Clinical Executive Group feeds directly into the ICS Executive Group and from here up to the ICB where the CMO (chair of the CEG) is a voting board member. As well as clear lines and purpose, this ensures that the CEG carries the influence required to help support and guide the ICS on clinical elements. Membership: The CEG will be a small group of clinical professionals that represent their profession as opposed to their organisation or place. This helps keep thinking and decision making at a wider-ICS level. It will be chaired by the CMO with a deputy chair from another profession. In keeping with principle one of the CCPL Integrating clinical and care professionals in decision making at every level of the ICS the core membership of the CEG was discussed at length to ensure inclusivity and full representation of clinical and care professionals. As a result the below membership has been agreed. This membership is agreed from a role/representation perspective with the acknowledgement that current post holders may change as we transition into an ICS. Chief Medical Officer Chief Nursing Officer ICS Chief Pharmacist Primary Care Clinical Lead (GP, locum, pharmacist etc.) +/- Hospital Dr (CMO) if the System CMO is a GP ICS Chief Allied Health Professional Local Authority Healthcare Lead (Social Work/Clinical practitioner) representation ICS Chief Health Care Scientist The link of the CNO between the CEG, System Quality Group, and Quality & Assurance Committee will strengthen the wider-system view on all things clinical, quality, and safety related. The Clinical Executive Group will: Co-design and delivery of the CCPL programme framework. Drive the organisational development and cultural transformation required across the system to support delivery of the ICS s vision and strategic priorities. Help set direction and advise the ICB. Hold to account the Clinical Forum and ensure that initiatives discussed at, and actions from, the Clinical Forum are undertaken in a timely manner and with sufficient resource. Be an acknowledged place for people to gain advice and guidance. Development of workforce. The Clinical Executive Group reports to the ICS Executive Group and ICB on progress, for assurance and for key decisions to be made as appropriate.
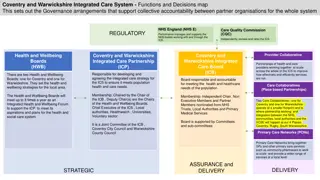
Clinical and Care Professional Governance within the ICS Clinical and Care Professional Governance within the ICS
Clinical Forum Clinical Forum ICS Structure: The Clinical Forum is a consultative forum that has indirect lines to the System Quality Group and direct reporting lines into the Clinical Executive Group. Membership: The membership has been constituted based on ensuring adequate representation of clinical groups by profession, place and organisation. Local Professional Network Leadership Pharmacy, Dental, Optometry etc. NHSE/I Representative(s) University Representative(s) Local Workforce Advisory Board Representative(s) CCG Clinical Leads Medical and Nursing Local Authority Public Health and Social Care Leads Primary Care Provider Clinicians 1 per place Chair CMO Place-based Leads Provider Clinical Leads Medical, Nursing, and Allied Healthcare Professionals, Healthcare Scientists and Pharmacists The Clinical Forum will: 1. Identify priority populations with opportunities for improvement in health with an ambition to promote equity of access and outcomes in healthcare. Support the development of Expert Advisory Groups (EAG)/Clinical Workstreams or work with existing groups to develop them as sub- groups of the Clinical Forum. Receive recommendations (option appraisals/ impact assessment) from the EAGs/ Clinical workstreams: a. Act as a sounding board to those presenting the recommendations providing additional clinical scrutiny. Review, challenge and advise on the content of the recommendations b. Identify key interdependencies with other recommendations/ work programmes that could affect this or other programmes of work c. Request impact assessments for the recommendations from enabling workstreams. 4. Receive regular reports from each EAG/ Clinical workstream on progress with transformation: a. At a minimum this will include an annual report. These shall be timetabled so the Clinical Forum receives reports from each group at different times b. Escalation of any concerns about progress as soon as these have been identified. Collate barriers and challenges to progress faced by EAGs/ Clinical workstreams. Facilitate discussions with enabling workstreams (workforce, finance, digital, research & innovation) influence their work programme and prioritisation to address these barriers/ challenges. Collate common themes regarding pathways from recommendations provided by EAGs/ Clinical workstreams. Facilitate discussions with relevant HCP groups (Population Health and Prevention, Primary Care, Planned Care, Urgent and Emergency Care) to influence their work programme and prioritisation to address these common themes. 2. 3. 5. 6. 7. Act as an advisory group for health and care professionals across C&W, taking representation from each health and care professional discipline.
Clinical Forum The Clinical Forum is a hive of multidisciplinary expertise across all organisations, places, community and primary care. The forum has representation from and access to specialist knowledge from a wide range of services and disciplines. Currently, the Clinical Forum is a consultative body providing a centralised location for the system to request independent clinical advice. With an open agenda, members or other system groups can add items for discussion at any point. A number of Expert Advisory Groups (EAGs) support the wider system on issues regarding the development and delivery of population-specific services. The Clinical Forum acts as a sounding board for the EAGs, providing additional clinical scrutiny and approving final recommendation papers. Outside of this, the Clinical Forum is not an authoritative body. However, as the ICS transitions, the Clinical Forum will need to transition alongside this to meet the new challenges, adapt to the new ways of working, and strengthen collaboration to work fully as an ICS. The Clinical Forum will transition into Place-based Clinical Forums to suit the new ways of working whilst continuing to meet as a system Clinical Forum on a quarterly basis.
Clinical Forum Development: Clinical Forum Development: Collect Collect Collate Collate - - Create Create Starting with an unfacilitated discussion allowed for an open, honest, no-judgement conversation without the pressure, or potentially perceived prohibitions, of external involvement. Open discussion NHS Elect facilitated multiple CCPL workshops at the Clinical Forum. The use of external facilitation allowed for a structured and productive discussion that resulted in crucial foundations for change. Facilitated discussion We shared the Key Lines Of Enquiry (KLOEs - the national guiding principles for planning in the form of thirteen questions) with the Clinical Forum to see common themes, strengths, weaknesses, and where/how we can improve. KLOE research Example flow of sessions: The NHS Elect facilitator fed back that they were really impressed by the openness and honesty of forum members contributions. A really rich conversation with a genuine intent for moving things on. Explore Optimising time spent together Collective understanding of what we are here to do- what good looks like Discuss Building on work so far How we work together as a system leadership team to implement our plans Revisit CCPL 5 Principles Individual and collective actions We reviewed the outputs from all three development elements and designed a forward look of how to change the Clinical Forum into a new ICS vehicle for Clinical and Care Professional Leadership transformation. Next Steps
Clinical Forum Development Clinical Forum Development Rebrand and relaunch: It has been agreed to rebrand and relaunch the Clinical Forum. The name will change as part of the rebranding to ensure a more inclusive title that will resonate with non-clinical colleagues. As we transition into an ICS it is a optimal time to refresh and revitalise the current Clinical Forum. This will heavily focus on communications and engagement with the CCPL principles of frequent and open system-wide clinical and care interaction and expand, strengthen and communicate a new clinical and care engagement network across the system . Whilst implementing expanded engagement opportunities and increased communications, rebranding and relaunching the Clinical Forum in its new form will reignite current members passion as well as bringing new membership to the table (discussed further below). To ensure effectiveness we will work with the Communications and Engagement team who will provide support and guidance as well as strengthening the comms and advertising element of the relaunch. Expanding the radius: The Clinical Forum already has wide representation, however as part of the relaunch the membership will be extended further. By opening up the Clinical Forum to a wider group of health and care professionals it allows system members to get exposure to System Thinking that they may not have experienced. This developmental aspect will be further strengthened by allowing more junior members to volunteer to take part in initiatives discussed at the Clinical Forum which they can then use towards their qualifications and career development. Clinical Forum This increased exposure is a first step towards the Clinical and Care Professional Leadership programme. The CCPL programme will be looked at in more depth alongside the People and Organisational Development workstreams discussed further in slides (XX). Current reach The Clinical Forum will remain an open consultative forum. One of the key strengths to this group is the wide reach across the system and ability to share learning. As part of the relaunch it will also be looked at as to bringing in external speakers on a more frequent basis and encouraging ICS partners to attend and present. Expanded radius
Clinical Forum Levels: The Clinical Forum(s) will adapt from its current static central position into more wide-spread, adaptive models throughout the system. System: The Clinical Forum will maintain a system function, however this will take the form of a quarterly event. Its position and function across the ICS at System, Place, and Care Collaboratives is being worked through and will develop further over time as each element matures. The quarterly System Clinical Forums will be large and fully inclusive events. They will provide an opportunity for horizon-scanning and wider-shared learning. The principles of the relaunch and rebrand, as well as extended radius is intended to continue throughout the various models. System Care Collaboratives: Our system has two Geographical Care Collaboratives ; Coventry GCC and Warwickshire GCC. Care A Care Collaborative programme is in progress with a three stage, multi-year development plan. The Clinical and Care Professional Leadership programme will work with the Care Collaborative programme to understand the requirements and support the co-design and implementation of agreed models. Collaboratives Place: The Clinical Forum will transition into Place- based forums. This model better fits with delivering care closer to home, population health, and future Place delivery models. Place
Clinical and Care Professional Networking Clinical and Care Professional Networking Clinical and Care Professional networking is intrinsic the CCPL Principle; Embed clinical and professional leadership into system governance . It focuses heavily on assessing existing groups, comms/engagement routes, stakeholder outreach, meeting set-ups (including membership) etc. As part of the ICS Transition, the Governance workstream undertook a system-wide mapping exercise. The exercise reviewed all current committees, sub-committees, consultative forums, boards, and sub-groups. It reviewed aspects such as membership, purpose, reporting, authority and accountability etc. It was stated in the clinical strategy and agreed by the Chief System Transformation Officer that all transformation programmes should have a Clinical and Care Professional SRO. It is being reviewed to identify any gaps in this model and ensure that Clinical and Care Professional SRO s provide updates to the Clinical Forum. From a CCPL perspective the Governance mapping exercise allows us to answer and depict questions such as If you were going to engage with Phlebotomy, how would you? to ensure clear routes for clinical and care professional governance to flow through the system. Additionally, it provides the opportunity to build a network for clinical transformation as well as for CCPL providing foundational connections for; Communications network Engagement network Leadership development network Shared learning network
Communications and Engagement Communications and Engagement Increase awareness of system and structures As the ICS transitions and the structures change, it will be key to ensure that members at all levels of the system are aware of the governance and routes that have been agreed. Developing materials to provide an overview of the system development, structures, newly established Clinical and Care Executive and it s purpose, will help people know where to go and how to get there in regards to advise, guidance, support and approval etc. We will work with Comms and Engagement to create the material in a range of shareable formats and share case studies to highlight the impact of integration. Develop mechanisms for connecting Work with the Digital workstream to explore opportunities for the use of digital platforms and initiatives to connect colleagues such as Clinical and Care Professionals MS Teams, WhatsApp Groups etc. With the mechanisms in place, the focus will be on engagement activities such as Clinical and Care Professionals summits, open question sessions etc. We will explore ideas around popular new-age mediums such as blogs and podcasts etc. Demonstrate visible leadership and enable sharing of best practice Build on the shared learning and best practice by looking at how internal content such as case studies, presentations, Q&A s etc. from clinical and care professional leaders including VCFSE, APHs and others, as well as external content could be made widely accessible. Support with skills of engagement, coproduction and working with people and communities With the development of the CCPL leadership development programme/offer, we will work with Comms and Engagement and People/OD to ensure that newly embedded training, mentorship, and development opportunities are widely advertised and accessible. In support of the ICB Engagement Strategies involving communities, voluntary, community and social enterprise sector , we will work with Comms and Engagement to strengthen engagement opportunities between CCPL and our public.
Clinical and Care Professional Leadership Plan Clinical and Care Professional Leadership Plan Clinical and Care Professional Leadership development is a key aspect to ensuring that the current and future leaders of tomorrow have the necessary skills to bring strength and unity to the system. At present, there is not a full system programme for development in place. Instead, developmental programmes are confined within organisations. The level of programmes, success, and uptake is unknown. In response to the CCPL principle 1 of Integrating clinical and care professionals in decision making at every level of the ICS , and principle 4 of Providing dedicated leadership development for all clinical and care professional leaders , the CCPL workstream are discussing the development of a mentorship programme as part of the Clinical and Care Professional Leadership Plan. As part of the CCPL Framework, a series of mapping exercises will take place. 1. Map what mentorship, talent spotting, and leadership development programmes exist within each organisation. 2. Review and harness the good from individual organisations to join up and develop a system offer. 3. Embed a programme at system level. HEE/ CCG HEE/ CCG L.A CWPT L.A CWPT PLACE & PCN GEH Mapping System PLACE & PCN PLACE & PCN GEH SWFT GEH UHCW SWFT UHCW SWFT
Clinical and Care Professional Leadership Plan Clinical and Care Professional Leadership Plan Identify Identify the future leaders of tomorrow. Improve talent spotting and help the system learn how to identify future leaders. Teach Once the graduates have become the new leaders, after time they will progress into the mentors of the next wave of future leaders. Finishing the cycle, graduates will eventually help to identify the next wave of future leaders. Identify Teach Learn Learn Enable future leaders to learn the skills required for leadership at an ICS level. Design and implement mentorship programmes to allow candidates to shadow leaders and learn on the job. Lead Lead After completion of the programme the candidates will go on to become influential and innovative leaders within the ICS.
Clinical and Care Professional Leadership Plan Clinical and Care Professional Leadership Plan Further to the ICS transition requirement to Embed clinical and care professional leadership into system governance , the clinical and care professional leadership workstream will explore the wider organisation development work required. Leadership Development: The aim is to build a full leadership development programme consisting of elements such as; Education/training Mentorship Talent spotting Leadership exposure opportunities As previously mentioned, this will include exploring all of the local practices and programmes, expansion of interaction with universities, review and collation of external development opportunities such as masters, NHS leadership courses, HEE support and schemes etc. Engagement with the People Directorate has commenced where will work closely to assess areas that require additional work. Workforce: With the learning piece of the programme covered above, the programme will also include the more workforce related elements. This is to ensure that current and future leaders are brought into the system in the most effective, efficient, and inclusive way, as well as keeping the excellent workforce that we have. To develop this further we are keen to explore in more depth: Workforce planning and identification of risk. Recruitment and retention. Succession planning. Asking what is system leadership and the characteristics? and how it can be embedded into job descriptions to ensure that as a system we recruit the right candidates. This will involve the utilisation of the ICB Leadership Competency Framework once agreed. In support of this, the CCPL will work with the People Directorate to co-develop a strategy for recruitment and retention with support offer being vital to this. As this develops, additional work will be undertaken with the Communications and Engagement workstream to help get the message out across the ICS.
Resource Review Resource Review In response to the Clinical and Care Professional Leadership principle 3 Ensuring clinical and care professional leaders have appropriate resources to carry out their system role(s) , we are undertaking a full resource review. The review consists of three separate aspects: 1. ICS Chief Speciality Leads 2. Benchmarking the approaches to employment and pay for Clinical and Care Professional Leaders 3. CCPL resource provision ICS Chief Speciality Leads Review The ICS Chief Speciality Leads are valuable assets to the systems wider working. These important roles provide leadership, representation and support to the wider programme as well as providing accountability and assurance to the system. As our system transitions into a new way of working, strong leadership, system, and people development will be key to becoming a thriving ICS . Within our system we already have various ICS Speciality Leads in position such as ICS Chief Pharmacist, ICS Chief AHP etc. As well as reviewing our current posts to identify the contractual set up and how we continue these, we will be reviewing where there may be a requirement and appetite for implementing additional lead posts. If any additional leads are required, it will need to be identified as to how and where these are funded etc. Benchmarking approaches to employment and pay for Clinical and Care Professional Leaders It is recognised that across most systems the approach to paid time for engagement and research etc. varies considerably. In response to this most systems are reviewing their clinical and care professional arrangements. Many systems have stated a commitment to ensuring that clinical and care professional leaders are from a range of professional backgrounds. Undertaking a transformation to this is a significant task that spans across all organisations, system, place, Local authorities etc. For this reason, it will start with an explorative exercise. Gloucestershire ICS have commenced an excellent exercise to benchmark the various approaches across multiple systems. Variations include approaches to describing roles (e.g. job descriptions), models for employment (direct employment or with current employer), approaches to rates of pay, approaches to funding time (e.g. sessional rate , how long are sessions? Or another approach), etc. We will build plans to benchmark the various models within our ICS. Once the benchmarking process is completed, we will begin to explore (internally) which models work best, what can be standardised, can we create a single model or a hybrid approach? As more ICS s engage in this work, we will share our learning and thoughts as this develops into a regional/national collaboration.
CCPL Resource Provision: The CCPL Network Manager is responsible for supporting the ICS SROs to design, develop, and deliver the ICS model. They will review all groups across the system to identify any gaps in CCPL representation and aim to rectify. They will look at interaction across the system and, through a functions and decisions map style process, look to establish an effective CCPL network. At present the CMO position does not have a dedicated team of resource to support the design and delivery of the CCPL programme. The Director of Nursing and ICS Chief AHP have been pivotal to supporting the CMO with the wide-spread elements that contribute to the design of our framework. However, it is acknowledged that going forward it needs to be adequately resourced. A resource review is underway, one element is the CCPL delivery team. An ideal team has been designed which will be scoped further throughout the process. Administration support is vital to the continued and effective running of the CCPL programme. Management of the Clinical Executive Group and Clinical Forum will be core to the role. However, whilst the CCPL programme is in its development and establishment stage, administration support for the CMO will be key to managing the multiple elements of the programme. It is appreciated that funding is finite and so multiple options will be explored such as; Temporary 3-6 months secondment and then review Shared resourcing Review how similar resource could be shared across other directorates The Leadership Development Lead is responsible for working with People/OD to create and implement a Clinical and Care Professional Leadership Plan. The systems aim is to have a fully developed leadership programme for clinical and care professionals at all levels. This will include, mentorship, talent spotting, educational support and training. The options from the review will be collated and built into a wider resource proposal for the ICS. Network Manager The Engagement Lead will focus on the CCPL principle of frequent and open system- wide clinical interaction. This includes engagement opportunities such as quarterly summit s and open question sessions with the CMO/CNO etc. They will expand, strengthen and communicate a new clinical engagement network across the system. This includes the use of improved digital initiatives as well as reviewing current communications in place. Transformation Manager Administration Support The Clinical Strategy Lead will support the strategy development. CMO The strategy will either be a Clinical Strategy or a Clinical and Care Professional Leadership Strategy. These strategies are very different and will depend upon the systems requirements. Leadership Development Lead Clinical Strategy Lead The Transformation Manager will be responsible for supporting the CMO to bring together the various elements as the CCPL work is developed into an active programme. Engagement Lead The Transformation Manager will help oversee the forementioned workstreams, build a workplan, implement and manage reporting and assurance to the ICB etc.