Critical Events in Ventilation and Oxygenation Management
Explore two challenging cases of respiratory complications in surgical patients: one involving an asthmatic individual presenting for appendectomy and the other a smoker with a humerus fracture. Learn about critical preoperative considerations, approaches to managing ventilation difficulties, and differential diagnoses for respiratory issues in these scenarios.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Critical events in ventilation and oxygenation Samuel Yang, MD
Case #1: The Asthmatic 45 year old man presenting for appendectomy due to acute appendicitis Reports history of asthma No other medical history No prior surgeries or anesthetics Elevated WBC otherwise normal labs What preoperative information do you want? Has never been hospitalized with an asthma exacerbation Uses a rescue inhaler about once per month Does not use a long acting controller or steroids Auscultation reveals diffuse, mild expiratory wheezing Airway exam normal
Case #1: The Asthmatic How will you prepare the patient preoperatively? Active bronchospasm should be treated preoperatively with a beta-2 agonist (albuterol) Emotional stress/anxiety can provoke an asthma exacerbation. May consider anxiolysis with a benzodiazepine How will you induce the patient? What are you concerns regarding the appendicitis? Asthma? Rapid sequence induction given acute abdomen Adequate depth of anesthetic prior to airway manipulation
Case #1 You perform a rapid sequence induction. On the first attempt of direct laryngoscopy, you have a grade 1 view of the vocal cords and easily pass a 7.0 endotracheal tube. The circuit is connected and you attempt manual breaths. Ventilation is difficult. Capnography demonstrates minimal CO2 return. What is your differential? Given the patient s history this is MOST likely bronchospasm Don t forget the possibility of an esophageal intubation! Could this be anaphylaxis?
Case #1 What are your next steps? (Have a system!) Notify the team (good communication is key) High flow 100% O2 if not already Deepen the anesthetic Rule out other problems with the endotracheal tube such as: Esophageal intubation (breath sounds might not be helpful in severe bronchospasm. May need to confirm placement with direct laryngoscopy Kinked endotracheal tube Mainstem intubation Administer beta-2 agonist Consider epinephrine (low dose), corticosteroids, ketamine Consider arterial blood gas
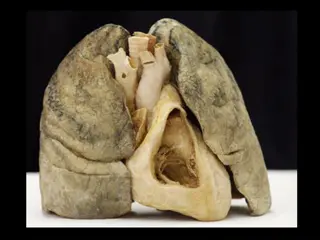
Case #2 67 year old man presents for operative fixation of a humerus fracture following a scooter accident. Long time smoker with a chronic cough No other past medical or surgical history, but seeks little medical care, no other injuries Diminished breath sounds throughout but no wheezing Room air saturation 93% Given an albuterol nebulizer prior to surgery Smooth IV induction and a straightforward intubation is performed. He is placed on volume control with Vt 500, RR 12, PEEP 5; maintained with sevoflurane. One hour into surgery your ventilator alarms for high airway pressure and you notice tidal volumes are low. Vital signs are stable.
Case #2: High peak airway pressure What is your differential diagnosis? Bronchospasm Mainstem intubation Mucus plug Auto-PEEP Pneumothorax Kinked ETT
Case #2: High peak airway pressure How will you manage and evaluate the patient? Start with 100% O2 at a high flow Auscultate the lungs (bronchospasm, pneumothorax, mainstem intubation) Check the tube and circuit (kink in ETT or circuit) Disconnect the circuit and suction the ETT (mucus plugging, air trapping) Your evaluation reveals diminished breath sounds on the left. What now? Mainstem intubation versus pneumothorax High index of suspicion for PTX due to recent trauma and possible COPD Check the tube. Has it migrated?
Case #2: High peak airway pressure As you are checking tube placement, the blood pressure returns as 74/48 and the heart rate is 112. What is your diagnosis? What is your next step in management? Needle decompression with a 14g or 16g angiocatheter in the 2nd intercostal space, mid clavicular line Chest tube after needle decompression
Case #3 76 year old woman with known moderate COPD undergoing cholecystectomy. During the course of the surgery the patient develops hypotension, diminishing tidal volumes and increase peak inspiratory pressures. SpO2 is normal. What is your differential? Auto-PEEP Pneumothorax Anaphylaxis with bronchospasm
Case #3 How will you evaluate and manage the patient? What s your system? Auscultation reveals bilateral breath sounds without wheezing. You disconnect the circuit to suction the endotracheal tube. When you reconnect, inspiratory pressures have improved; hypotension resolves. What is your final diagnosis?
Case #3: Auto-PEEP What is Auto-PEEP? So many names: intrinsic PEEP or air trapping Condition of incomplete emptying of alveoli at the end of exhalation Causes of Auto-PEEP Ventilation-associated factors: High volumes, rapid rate, short expiratory time Disease-associated factors: Airway obstruction (asthma and COPD)
Case #3: Consequences of Auto-PEEP Cardiac performance Elevated levels of Auto-PEEP can decrease cardiac output by decreasing venous return, reducing ventricular compliance, and increasing right ventricular outflow impedance Barotrauma and pneumothorax Increased work of breathing Flat diaphragm Lungs on the flat portion of pressure volume curve, i.e. more pressure needed for a given tidal volume
Case #3: Management of Auto-PEEP Patients with asthma and/or COPD need thoughtful ventilator management In the event of hemodynamically significant auto PEEP, disconnecting the circuit and allowing spontaneous exhalation can help relieve auto-PEEP Fix reversible causes: treat bronchospasm Decrease tidal volume, respiratory rate Increase expiratory time (I:E ratio) Apply external PEEP to prevent small airway collapse (not so much that expiration becomes more difficult)
Acute respiratory deterioration peak inspiratory pressure (PIP) PIP No change in PIP Plateau pressure unchanged Plateau pressure compliance: abdominal distension, PTX, atelectasis, ARDS, Auto-PEEP, edema Airway obstruction: bronchospasm, secretions, kinked tube Air leak Low fresh gas Pulmonary embolus
Case #4 45 year old woman presents for total abdominal hysterectomy due to menorrhagia. Past medical history is significant for acid reflux and diabetes. She is induced and intubated uneventfully. 45 minutes into the procedure her SpO2 drops suddenly from 98% to the 80s. What are your immediate next steps? Notify the team High flow 100% O2. Check the gas analyzer are you delivering the desired FiO2? Check other vital signs. Is there a pulse? Is there ETCO2? Hand ventilate to check compliance and check for leaks Auscultate breath sounds and check the ETT Suction the ETT
Case #4: Hypoxemia What is the differential diagnosis for hypoxemia? Low FiO2 Hypoventilation Ventilation/Perfusion mismatch (V/Q) Diffusion abnormality Increased metabolic O2 demand Hemoglobinopathy (methemoglobinemia, carboxyhemoglobinemia though SpO2 should be normal in the latter) Artifact
Case #4: Hypoxemia Low FiO2 Potential causes: O2 source failure or pipeline crossover of gases Action: Check gas analyzer. Turn on auxiliary O2 tank or switch to Ambubag with portable O2 tank. Hypoventilation Potential causes: Circuit leak, low fresh gas, obstructed ETT, ventilator asynchrony Normal A-a gradient Action: Evaluate from patient to anesthesia machine and correct identified abnormalities
Case #4: Hypoxemia V/Q mismatch Imbalance of ventilation and lung perfusion Refers to conditions between two extremes: Dead space ventilation: Ventilation without perfusion Intrapulmonary shunt: Perfusion without ventilation Examples of causes: Mainstem intubation, mucus plug (leading to distal airway collapse), pleural effusion, pulmonary edema, ARDS, pneumonia, atelectasis, pneumothorax, hypotension, embolism How would you work through these possibilities?
Case #4: Hypoxemia Diffusion abnormality Typically seen in chronic lung disease, e.g. pulmonary fibrosis Unlikely cause of the acute change Increased metabolic O2 Delivery of O2 is outpaced by metabolic consumption Sepsis, malignant hyperthermia, thyrotoxicosis, neuroleptic malignant syndrome Treat the underlying cause. Supportive care with high FiO2 delivery
Case #4: Hypoxemia Hemoglobinopathies Methemoglobinemia SpO2 ~85% Classically in anesthesia seen occurring after local anesthetic use Treat with methylene blue Carboxyhemoglobinemia Would not see SpO2 changes, but low PaO2 on blood gas 100% O2 delivery Artifact Check a blood gas to confirm true hypoxemia