Dental Malpractice Risk Management Strategies
Dive into the complex world of dental malpractice with expert insights on risk management, legal concepts, common mistakes, and case examples. Learn how to prevent malpractice issues in dentistry through informed consent, pharmacology awareness, and effective recordkeeping. Explore the ethical considerations and practical tips essential for dental professionals to navigate malpractice challenges successfully.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
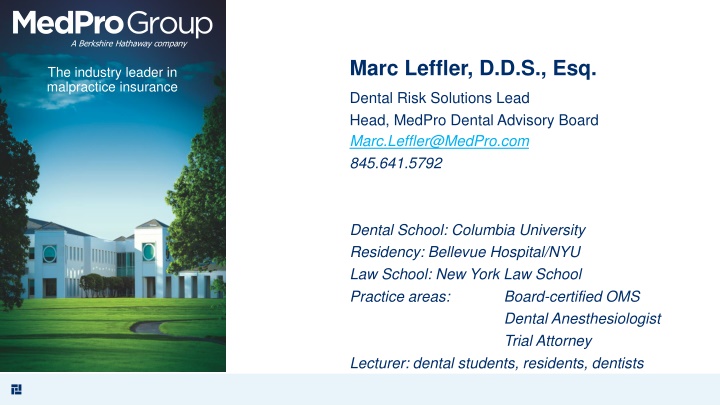
A Berkshire Hathaway company Marc Leffler, D.D.S., Esq. The industry leader in malpractice insurance Dental Risk Solutions Lead Head, MedPro Dental Advisory Board Marc.Leffler@MedPro.com 845.641.5792 Dental School: Columbia University Residency: Bellevue Hospital/NYU Law School: New York Law School Practice areas: Board-certified OMS Dental Anesthesiologist Trial Attorney Lecturer: dental students, residents, dentists
DENTAL MALPRACTICE: WHAT IT IS AND HOW TO PREVENT IT; AN APPROACH BASED IN RISK MANAGEMENT Punjabi Dental Society Montebello, CA July 23, 2023 2
Topic Overview A Case Example to Start - - Before you know the law, just like juries in some states Let's Joust, or on second thought, let's not General Legal Concepts (50 States + DC = 51 different sets of concepts) with "Anatomy" of a Dental Malpractice Lawsuit CA Law Why Insure? Definitions: Dental Malpractice; Informed Consent & Lack Lack of Informed Consent (LOIC) without negligence Pharmacology: Know What You're Giving Dentistry's role in the opioid crisis Medicine Concepts and Health History Recordkeeping CA Law How About Some Quasi-Cross-Examination? Big Ticket Items in Dental Malpractice Frequency vs. Severity Closed Case Studies Risk Management Takeaways The Ethics Behind "Do No Harm" (Work Within Your Abilities) Referrals in the World of a New Employee 3
LET'S START WITH A CASE: SWALLOWED/ASPIRATED OBJECTS - - THE BASICS OF A GROWING TREND An object is swallowed when it leaves the back of the oral cavity and makes its way into the GI tract: esophagus, stomach, small intestine, large intestine (colon), rectum. - removal may be by endoscopy, colonoscopy, surgery, or fecal passage An object is aspirated when it leaves the back of the oral cavity and makes its way into the respiratory tree: glottis, trachea, bronchi, lungs. - removal may be by bronchoscopy or surgery Common objects swallowed/aspirated - burs (drills), endodontic (root canal) files, implants and attachments, implant drivers, impression materials, pieces of fillings, crowns, orthodontic brackets 4
COMMON MISTAKES TO GET THERE Failing to protect against traveling behind the oral cavity almost always doable Rubber dam, threaded or wrapped floss, gripping instrument ("90 cent solution"), gauze drape, suction Failing to maintain dental instruments Friction grip on handpieces, too many sterilizations, substandard quality, improperly bent Failing to position patient upright when possible Gravity helps or hurts Failing to plan for reflex loss under sedation or GA Failing to use assistant Must be properly trained Suctioning 5
HOW TO DEFEND SWALLOW/ASPIRATION CASE First, let's try to figure out why the upswing, and end it before it happens! Now, can we defend it? (Hint: hardly, if ever!) Potential argument: entirely unforeseen events - earthquake, construction debris BUT STILL, most can be protected against anyway - - that's the purpose of preventive steps. 6
Swallow/Aspiration Case Study #1 A 20 year-old woman in need of a composite restoration presented to her dentist toward the end of a college vacation period. At the start of the preparation of the tooth, performed with local anesthesia and N2O/O2, the bur came loose from the handpiece, and was lost from the sight of the dentist and the assistant who had been using a high-speed suction. After the profuse coughing stopped, the restoration was resumed and completed, which took some 30 minutes more. Once the procedure was completed, the patient was told to go to a hospital emergency department for evaluation, which she did. A radiograph showed the bur to be located near the junction of the stomach and duodenum. The treating physician told the patient that she should pass the bur within 2-3 days at the latest. On the 5th day, she began to have severe abdominal pain, so she returned to the hospital, where a CT revealed that the bur had pierced through the wall of the colon. A laparotomy to remove the bur and close the defect was performed. She missed nearly 4 weeks of the following semester, so she elected to skip the semester altogether. A scar persists. Any valid theories for negligence? 7
Swallow/Aspiration Negligence/Damages Theories 1. 2. 3. 4. No or inadequate protection against swallowing/aspiration!!! Inattentiveness of assistant? Friction grip maintenance or improper tightening? Would endoscopy have been possible with more timely referral? Some questions: Were actions of MD in the ED appropriate? Is the dentist on the hook for that? Is the dentist liable for the abdominal scar? Is the dentist liable for the missed semester? 8
A-Jousting We Will Go! And I don't mean a medieval horse game! Huge driver of claims. Why is dentistry so different from medicine in this regard? Perhaps dental school at least a generation or two ago is the answer. 9
NOW, THE LAW Usually subject to interpretation, far more so than dentistry and medicine 10
California Law of Malpractice Statute of limitations: 3 years from date of injury, or 1 year from discovery of the injury. (CA Code of Civil Procedure 340.5) Extensions for minors, ongoing treatment, fraud/deceit. Definition of malpractice: a departure from the standard of care which directly causes injury. All 3 elements proven by plaintiff (patient) or case ends. "What a reasonably prudent dentist ." Lack of Informed Consent failing to make patient an educated consumer Malpractice insurance Not statutorily required If you need reasons to insure - - - protection of assets, sleep, ethics. MICRA cap of non-economic damages [pain and suffering, emotional distress, loss of enjoyment of life, loss of society, disfigurement] (2023): $350,000 (prior since 1975 $250,000), up to $750,000 incrementally over 10 years. For wrongful death: $500,000 up to $1,000,000 over 10 years. This does not include directly related "economic" damages (prior and later), lost earnings, medical/dental costs, health insurance recoveries (if applicable) 11
CA Informed Consent (CA Code Regs tit. 9 sect. 784.29) Prior to the start of a test, surgery, procedure, or "other care", the patient shall be informed, in terms understandable to that patient, as would a "reasonable" practitioner, of: Risks of proposed intervention Nature and description of proposed procedure Alternatives to proposed procedure, with its risks Patient's role in the process Risks, Benefits and Prognosis if patient refuses Eliciting patient's decision The doctor "should" record the circumstances of the patient's consent Note alone? Signed "consent form"? (A process, not a piece of paper, but memorialization helps.) Failure to comply: subject to discipline and malpractice 12
Informed Consent Exclusions (CA) Formal 1. 2. "Simple and Common" Exception: Risks are remote "Emergency Exception": Life-threatening situation (the law presumes consent) BUT reasonable effort to contact family member/representative and no knowledge of DNR Informal and commentary "Extremely remote possibilities" But a 1-3% chance is not "extremely remote", Martin v. Richards (WI [!], 1995) DDU (UK Defense Union) says in 2018 that IAN injuries occur in 6% of third molar removals DDU says in 2018 that permanent lingual nerve injuries occur in 0.5% of third molar removals Journal of Oral Medicine and Oral Surgery (2023): lingual nerve injury 0.5%-8.9% of third molar removals Journal of Oral and Maxillofacial Research (2014): IAN injury 0.35%-8.4% after third molar removals Information unrelated to the diagnosis provided Detailed technical information not likely to be understood 13
Purpose of Informed Consent, and Ramifications of Lack Purpose: Make the patient an educated consumer; let them fully understand what they are getting into, with respect to procedure and anesthesia/sedation/analgesia Generally not a delegable duty Basics: Provide the required information in language understandable to the patient (or guardian) A language (English, Spanish, Chinese, etc.) fully understood by the patient A level of language appropriate for the patient (6th grade education vs. a Ph.D.) No professional vernacular, i.e. numbness rather than paresthesia Lack of informed consent = tortious battery ("unwanted touching") = a basis for malpractice Usual malpractice: a departure from the standard of care which causes damage LOIC-based malpractice includes even a properly-performed procedure which leads to damage, simply because patient not adequately advised beforehand 14
"Anatomy" of a Lawsuit Complaint (Timely per statute of limitations? Adequate COA stated?) Answer (Timely or risk default-don t delay; denials to preserve rights later) Discovery (No trial by ambush ) Motions (To dismiss; to get further discovery; to limit issues for trial) Depositions (Yes, this is a test!) Parties, experts?, witnesses On-the-spot challenge? Let's discuss preparation and question types Mediation? Settlement discussions? Trial (A jury of whose peers?) Jury voir dire: to speak the truth Verdict (To truly say ) Judgment entered Appeal (Mistakes along the way? By whom?) 15
How is Malpractice or LOIC Proven by Plaintiff? Through Expert Testimony, by way of Opinions Ask 10 dentists the same question and you ll get 10 different opinions. Experts for plaintiff and defendant always have differing opinions. Who/what is an expert? CA Evidence Code sect. 720(a) "One with special knowledge, skill, experience, training or education on the subject to which the testimony relates" Must be founded in accepted, not junk , science. Jurors are generally lay people. There is no published, admissible Standard of Care, at least in most courts Learned treatises and journal articles/studies generally excluded to prove position. But usually ok on cross-examination. Association publications excluded. But usually ok on cross-examination. Jurors may seek no outside information from people, journals, internet, broadcast media, etc. So, who is correct? Whoever the jury believes. 16
PHARMACOLOGY 17
THE (MOST) RELEVANT DRUGS Local anesthetics Lido, carbo, septo, Epi has physiologic effects, both desired and undesired Is 4% solution ok for mandibular block? Analgesics Nitrous oxide (also weak anesthetic, as a supplement) NSAIDs Acetaminophen Narcotics Acetaminophen w/ codeine, Hydrocodone, Oxycodone Sedative-hypnotics Benzodiazepines (Xanax, Valium, Versed) Antibiotics Which one and why? Benefits and side effects? The trend against them, but Premedication (IE, prosthetic valves, certain congenital heart disease, heart transplants) So, follow up on "yes" answers to heart disease and other "yes" answers 18
The Role of Dentistry in the Opioid Crisis A 2018 retrospective large group study regarding 2015, performed at the Stanford University School of Medicine and published in JAMA Internal Medicine, reported alarming results relating to dentists and dentistry: (1) 5.8% of studied patients, age 16-25, who received their initial prescription of opioids from their dentist were diagnosed with opioid abuse during the 12 months following that initial prescription; (2) of those studied in this age population who received opioid prescriptions, 30% of those received them from their dentist; and (3) the median number of narcotic pills received from their dentist by patients in the study who became addicted was 20. The study eliminated all people who had received any opioid prescriptions, or who had been diagnosed with opioid abuse, within the year prior to receiving opioids from a dentist, in order to try to focus in on the issue studied. 19
Opioid Case Study: The Set-Up Case #2 Patient background 18 year old male recent (1 week ago) high school graduate (June) Admitted to trade school in carpentry program in September Patient wanted any needed dentistry performed before trade school start Clinical condition Episodically symptomatic soft tissue impacted tooth #17 Gingiva inflamed and tender Dentist prescribes 7-day course of Amoxicillin Patient re-appointed for extraction upon completion of antibiotics Date of treatment With local anesthesia, conservative soft tissue incision made with tooth elevated out, and sutured Patient requested prescription for "Tylenol with codeine"; dentist did not anticipate significant post- op pain, given the ease of extraction, but gave 20 tablets, 1-2 q4h prn pain, "against [his] better judgment". Amoxicillin continued for 3 additional days. 20
Opioid Case Study: The Post-Op Period Day after extraction Patient called office to complain of "writhing in pain"; dentist says take pain meds and local measures Third post-op day Presents to office with pain of 10 on a scale of 10, having used all pain meds No clinically apparent basis for that degree of pain; patient asks for stronger pain meds Dentist prescribes hydrocodone, 15 tablets, 1 q4h prn pain Repeated contacts to dentist Daily calls to office with severe pain complaints At suture removal visit, site looked to be healing well, but patient continued to complain severely Dentist prescribes oxycodone, 20 tablets, 1 q4h prn pain 3 days later, patient called, having finished his meds and asking for refill Dentist knew this meant patient was taking more than prescribed, but gave refill anyway Dentist refilled oxycodone 4 more times over next 5 weeks 21
Opioid Case Study: The Problem Manifests At 6+ weeks post-op, patient's father calls office Following arrest for driving under the influence of narcotics, patient was court-ordered to be admitted to rehab facility Patient remained in facility for 3 months so unable to begin trade school Patient re-admitted to facility after physical altercation at home with younger sister Patient never began trade school Father appointed guardian to handle patient's legal matters, and sued dentist Claims of malpractice: negligent prescribing of narcotics at surgical visit without demonstrated need; continuing to prescribe more and stronger narcotics at subsequent visits Claims of damages: narcotic addiction with inability to function without them; pain and suffering; treatment facility costs; and lost earnings as a carpenter 22
Opioid Case Study: How It Turned Out Result Claim for lost earnings dismissed Court: admission to any program does not necessarily mean later graduation Speculation may not serve as a basis to prove any element of any case No expert support to defend repeated prescribing of narcotics without demonstrated basis for need Pre-trial settlement Pain and suffering, addiction, rehab costs Sanctions by State Dental Board 6 month suspension Fine Mandatory continuing education re narcotic prescribing 23
Opioid Case Study: Risk Takeaways Complete understanding of pharmacology of opioids and all other prescribed meds Mechanisms of action Deposition is a test! Understanding of non-opioids for pain relief Appreciation of benefits of non-opioids Unwillingness to abide by "demands" of patients While a patient can dictate what they refuse, they cannot dictate what you must do. You are responsible for your actions, even if you felt "forced into" them by patient or employer Understanding of and abiding by applicable laws governing the prescribing of narcotics and recordkeeping Impacts of lawsuits and Board complaints 24
How to Avoid Opioids When Possible University Departments of Pharmacology and Dentistry Ongoing Joint Study Unpublished, as far as I know Using various dental pain models (toothache, extraction, RCT, perio surgery) Most efficacious meds: Ibuprofen 200 mg + Acetaminophen 500 mg Superior to all opioids studied for pain relief Not available to patients with anticoagulation, GI distress, liver disease 25
Reversal Agents Narcan/Naloxone for narcotics Flumazenil for benzodiazepines BUT 26
Remember Half-Life? It can spell TROUBLE! Half-Life: The time it takes for the amount of active drug in the body to reduce by half. 4-5 half-lives for elimination Versed half-life = 1.5-2.5 hours Flumazenil half-life = 7-15 minutes initial, 20-30 minutes subsequent Fentanyl half-life = 3-7 hours Narcan half-life = 30-80 minutes SO, YOU'RE NOT OUT OF THE WOODS BY FAR UPON REVERSAL! STRICT AND LENGTHY MONITORING/SUPPORT AFTER REVERSAL! 27
MEDICINE: THE TEETH ARE CONNECTED TO THE BODY 28
COMMON (not all!) MEDICAL ISSUES AFFECTING DENTISTRY & MALPRACTICE LITIGATION Anticoagulated patients (atrial fibrillation, deep vein thrombosis, valve surgery) Coumadin (Warfarin) v. Direct anticoagulants (Eliquis, Plavix) v. Platelet disorders (qualitative/quantitative) v. NSAID PT/PTT/INR/bleeding time Delayed bleeding v. immediate bleeding Diabetes Is NPO (fasting) ok? Hypertension Epi in local or no? Coronary artery disease Epi in local or no? Arrhythmias Epi in local or no? COPD Chronic renal disease Compromised immune system Corticosteroids Boost needed? Bisphosphonates 29
MEDICAL HISTORY TAKING AND FORMS Study the form(s) being used, especially if working in multiple offices Don't assume all forms are "yes/no"-configured consistently Follow-up is critical, and not just with "yes" responses Don't assume all forms address the issues relevant to the specific patient and/or procedure Consider social history issues Don't overlook allergies Cross-allergenicity Consider age-related issues Bisphosphonates, AFib Compare with prior forms and notes if available Notes such as "medical history reviewed" can have severe litigation effects Seeking input from others, medical clearance referrals, reviewing reference materials Connotes sophistication and diligence, not inexperience Let patients in on it 30
What Are Dental Records? Your best friend or worst enemy! Chart entries, both written and electronic Documents completed by the patient (history, HIPAA acknowledgement, insurance documents, clinical questionnaires, etc.) Radiographs Models Treatment plans Consent forms Billing statements Insurance filings, going and coming 32
The Worst Words a Defense Attorney Ever Heard in Court Judge: "Ladies and Gentlemen of the jury, if it wasn't written it didn't really happen"! 33
But You Can't Record Everything So what are the general rules of thumb? Judge/jury/patient might someday be reading your notes Accurate Complete ENOUGH DETAIL SO THAT A TRAINED DENTIST CAN FIGURE OUT WHAT WAS DONE, BASED SOLELY UPON THE WRITTEN NOTES! Contemporaneous Legible if handwritten Tailored, if electronic; not just a template (Let's play that out in a moment) Use abbreviations only if generally accepted Document communications with patient and other providers Business, not personal Conclusions about dentistry/conditions ok Personal judgments inappropriate What about texting and email? 34
MAINTENANCE OF DENTAL RECORDS Every State has different specific rules as to how long dental records must be maintained. ------------------------------- 22 CCR sect. 72543 Complete records shall be kept by a dentist for a period of not less than seven (7) years from the patient's last treatment. In the case of a minor, records shall be maintained until the person becomes 19 years of age, or until 7 years after treatment was completed, whichever is longer. 22 CCR sects. 123100-123149.5 Dental records are the property of the provider or facility that prepares them, but the dentist is required to allow the patient to see and receive copies. 35
And if Records Are Not Kept Long Enough or Complete Enough? Malpractice suit Possible default (case lost!); spoliation of records (case lost maybe!); jury charge; court sanctions; unfavorable/suspicious jury response Disciplinary Complaint Suspensions, revocations, fines, mandatory coursework, supervised practice, demonstration of corrective measures 36
Issues with Electronic Records Templates Example of template in use: healthy 24 y.o. woman for ext FBI #17 on 3/12/19; returns with paresthesia c/o 3/19/19 4/8/19: late entry for 3/12/19; discussed risks of pain, discomfort, IAN inj. with patient and guardian if applicable; lido/septo l.a.; flap reflected, 702 fissure to section M/D/P roots; Rx Amox 500 or Clinda 150, Ibuprofen, Norco 5/325 (By visiting OMFS who did ext) 5/2/19: 30 MOD (By GP practice owner) 5/2/19: Rev MH, oral exam, stressed OH, imp for mouth guard (By GP owner/RDH) 5/3/19: late entry for 3/19/19: pt presents for dry socket 17; irrigate, flush, DS paste; experiencing some numbness; told pt this is normal, can take up to a year to resolve (By GP owner) LET'S DO SOME QUASI-CROSS-EXAMINATION! 37
Frequency vs. Severity Behind the Carrier Scenes Categorization of Dental Malpractice Cases Frequency: how often a case type arises as a source of a malpractice claim Severity: how much money a successful plaintiff is paid for various case types 39
High Frequency Cases *Swallowing/Aspiration *Paresthesia Third molars: inferior alveolar, lingual/chorda tympani Implants: inferior alveolar Mandibular blocks: inferior alveolar, lingual/chorda tympani RCT Implant loss Technique, radiograph assessment, bone inadequacy, medical conditions Crown and bridge (margins, occlusion, contours, esthetics) Wrong tooth treatment Endodontic file separation without disclosure Infection Choice of antibiotic; side effects of antibiotic Sinus issues Upper molar extraction: roots anatomically within Tuberosity fracture Graft materials after Schneiderian Membrane tear during lift RCT Implants 40
High Severity Cases Failure to diagnose malignant lesions Trigeminal Neuralgia BRONJ/MRONJ *Paresthesia Lingual/chorda tympani, then inferior alveolar Ably holding up on deposition/cross-exam very important on anatomy-based cases *Swallowing/Aspiration Severity based upon where it goes and how it's removed (remember the bur through colon wall?) As compared with self-passage, endoscopy, or bronchoscopy * = high frequency and (potentially) high severity 41
Closed Case Study #3 Asymptomatic deep vertical FBI #32 in 30 y.o. male professional trumpet player. Perio defect distal #31. Referred from GP to OMFS for evaluation. PA shows M root within 2-3 mm of IAC; apex of D root not captured. Discussion of RBA by assistant is thorough: patient advised of risk of paresthesia, possibly permanent, but no more on that subject or its effects. Patient provided with consent form ; states did not bring reading glasses but signs. No specific risks written. Surgery with local anesthesia is uneventful: sectioned, and roots atraumatically removed with proper technique . Patient numb over course of V3 at 1-week visit (mapping done but not documented); slightly less numb at 1-month visit (mapping done but no comparative frame of reference); no subjective changes monthly; referred to nerve repair OMFS at 6 months. 43
Claims in the Lawsuit Lack of informed consent (delegated, no glasses, no embouchure warning, inadequate PA for explanation, no alternative of coronectomy, or nothing) recall: even if no negligence Negligence (inadequate radiograph PA vs. Pan vs. CBCT vs. nothing, no coronectomy/defer extraction, late referral/no mapping documentation) No claim of surgical error But there is a claim for unnecessary surgery (double dip with lack of informed consent) Damages (lost sensation - - pain and suffering; lost earnings as trumpeter) 44
Closed Case Study #4 38 y.o. female presents with fluctuant buccal swelling adjacent to deeply decayed tooth #4. Patient opts for extraction over RCT, etc. Dentist extracts tooth routinely and prescribes Flagyl. On third post-op day, patient calls office to report fever and persistent swelling. Receptionist independently advises patient this is expected, so not to worry. Patient presents on day 6 with continued symptoms. Dentist prescribes Clindamycin and local measures. Oral symptoms abate, but patient develops bloody stool 5 days later, and calls dentist, who says stick with it for another 5 days . Patient admitted for perforated colon due to PMC; undergoes partial colectomy. Any valid theories for negligence? 45
Negligence Theories 1. 2. 3. 4. 5. Delay extraction until infection resolves? I&D with C&S? Is Flagyl appropriate as empirical? Receptionist giving medical advice. Vicarious liability. Causation? Is Clinda appropriate as empirical without C&S? Should Clinda have been stopped with GI symptom onset? 46
Closed Case Study #5 50 y.o. male with disclosed PMH of HTN (controlled on meds) only, presents for single implant in area of #30, where tooth had been lost 2 years prior. Periodontist takes PA which captures entire site, and which demonstrates IAC 15.5 mm from crest. 13mm implant chosen. Following administration of local, patient becomes jittery and starts to move around, with odd opening/closing movements of jaw as osteotomy proceeds. Patient has grand mal seizure and immediately bites down on operating handpiece, pushing bur through lower lip. Procedure abandoned, appropriate medical care provided (transported), lip sutured at hospital but scarring persists, implant never placed. Any valid theories for negligence? Thoughts on cause of seizure? 47
Negligence Theories 1. 2. 3. 4. Adequacy of radiograph causation? Bite block? Finger rest? Failure to ID prodromal stage? 48
Some Medical Risk Management Takeaways Medical clearance with a patient s physician or surgeon should always be considered in a patient who is, or may be, medically compromised no matter the dental procedure being performed. Additional checks and balances: even with medical clearance, don't do what you feel uncomfortable doing. While a patient can dictate what they refuse, they cannot dictate what you must do. Patient safety, not necessarily patient desire, carries the day. 50