Dermatomycosis: Causes, Transmission, and Treatment
Dermatomycosis, a contagious skin disease caused by fungi, affects both humans and animals. Learn about the etiology, hosts, transmission, and manifestations in animals and humans. Understand the importance of early detection and treatment to prevent spread and complications.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
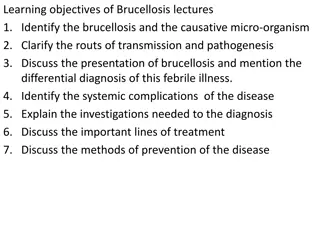
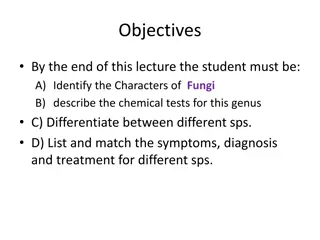
Presentation Transcript
Dermatomycosis A dermatomycosis is a highly contagious skin disease caused by fungi. It affects both people and animals. Other names for a dermatomycosis are tinea, ringworm, jock itch, and athlete s foot. Zoophilic fungi: live on animals other than people, but can be transferred to people. Etiology: Two genera of zoophilic fungi: Microsporum and Trichophyton Are responsible for nearly all cases of dermatomycosis that are zoonotic. The spores of these fungi are able to survive in the environment, in protected areas, for 18 months or more. They rely on keratin, a protein found in the outer layer of the skin, hair, feathers, nails, and hooves. 1
Hosts Dermatomycosis in animals is called ringworm. Cats, dogs, cows, horses, sheep, and rodents are the most common sources of zoonotic dermatomycoses. The following zoophilic fungi: Microsporum canis is carried by cats and dogs and causes the most common form of ringworm in these animals. It is transmissible to people Trichophyton mentagrophytes causes ringworm in rodents, cats, dogs, horses, cattle, and pigs. It is transmissible to people Trichophyton equinum is found on horses and rarely on people Trichophyton verrucosum is carried primarily by cattle, but can be found on people, horses, and sheep Microsporum nanum causes ringworm in pigs. It is rarely found on people. 2
Transmission 1. Not every person or animal that comes in contact with these fungi will develop clinical disease. 2. Some animals and people will be carriers while remaining asymptomatic. 3. Young animals and children are most often affected because their immune systems are not fully developed. 4. The same is true for people with suppressed immune systems, such as people with HIV/AIDS, those receiving chemotherapy, and organ transplant recipients. 5. Animal dermatomycosis is transmitted by direct contact with an infected animal or with items contaminated with fungal spores. 6. Grooming equipment, brushes, blankets, bedding, carpeting, furniture, air filters, shed hair, or any other item that comes in contact with an infected animal can become contaminated with spores. 7. Spores can survive in any place. 8. The incubation period varies in animals and people but is usually a few days to a few weeks. 3
Dermatomycosis in animals Young animals are most likely to develop ringworm lesions. The lesions typically seen with ringworm usually begin with: o scaly patches containing broken hairs. o The areas may become inflamed and turn red, swollen, and crusty. o In some animals, the lesions are not well-defined and may be more diffuse. o In these cases, the animal shows areas of alopecia that may become ulcerated if the animal licks or scratches the site. o Itching is not a common problem with ringworm. 4
Dermatomycosis in humans It is important to remember that animals are a minor source of dermatomycosis in people. In healthy people, lesions stay on the keratinized layers of skin and hairs, but in people with suppressed immune systems, the infection can go deeper and become systemic. Fungal skin infections in people are named by where they are found on the body: Tinea corporis is seen on the skin. The lesions appear as small, red spots that grow into large rings on the arms, legs, or chest. 5
Tinea pedis is also known as athletes foot. The lesions usually begin between the toes, where the skin is moist. They become red and itchy and have a wet surface. If the fungus spreads to the toenails, it becomes tinea unguium. The toenails become thick and crumbly. Scratching the area can spread the infection to hands and fingernails. Tinea cruris, also known as jock itch, is caused by fungus growing in the moist, warm area of the groin. The lesions are found most often in men who frequently wear athletic equipment. Tinea capitis, also known as ringworm, is found on the head. The lesions begin as itchy, red areas where eventually the hair is destroyed, leaving bald patches. Ringworm is the most common dermatomycosis in children. 6
Diagnosis Beyond the clinical signs, there are three methods used to diagnose dermatomycosis: The Woods lamp is a special black light that emits filtered ultraviolet light. When exposed to a Woods lamp, many but not all fungi will fluoresce bright blue-green. A lack of fluorescence does not indicate that no fungus is present. Hair is pulled from the outer edges of the lesion, where the fungi are still active. The hairs are placed on a microscope slide in a KOH (potassium hydroxide) solution to make the spores more visible. They are then examined under a microscope for the presence of spores on the hair shaft. This method of diagnosis is useful up to 70% of the time. For identification of the specific fungus causing the dermatomycosis, hair from the edge of the lesion must be cultured on specialized media in a specific environment. Growth can take up to several weeks, and each fungus grows in uniquely appearing colonies on the media. 7
Prevention o Begin treatment immediately on any animal that develops lesions. o Maintain hygienic living conditions for animals. o Reduce crowding as much as possible to avoid direct contact. o When infected animals are present, clean all bedding,toys, carpeting, furniture, kennels, stalls, barns, or anywhere the animal has been. o Wear gloves when handling potentially or obviously infected animals. o Since fungi prefer moist areas for growth, keep kennels, barns, and other living quarters as dry as possible. 8