Different Types of Meningitis and Their Causes
Learn about bacterial meningitis, viral meningitis, fungal meningitis, parasitic meningitis, and amebic meningitis - their causes, symptoms, and treatment options. Discover how each type can affect the nervous system and brain.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
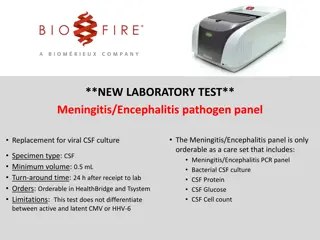
Presentation Transcript
BACTERIAL MENINGITIS BY: NABEELA KALEEM STUDENT OF: ALBANY COLLEGE OF PHARMACY AND HEALTH SCIENCES
WHAT IS MENINGITIS? Meningitis is an infectious disease in which the protective membranes surrounding the spinal cord and brain become inflamed. Meningitis can be caused by a variety of factors, which is important to identify, since the cause of the disease determines the treatment of choice.
TYPES OF MENINGITIS Bacterial Viral Fungal Parasitic Amebic Non-infectious
BACTERIAL MENINGITIS Caused by bacteria and requires immediate medical attention. This type is one of the most serious and can be deadly. There are vaccines which may be used to help prevent certain types of bacterial meningitis. The way bacterial meningitis is spread is dependent of on the bacteria. It is usually from person to person contact and may even spread by food. Delayed treatment can cause permanent damage/ death.
VIRAL MENINGITIS This type of meningitis is less severe than bacterial although it may become serious if not taken care of properly. People that have an otherwise healthy immune system may overcome this type of meningitis on their own. There are influenza, measles, mumps and chicken pox vaccines which may help against viral meningitis. The virus that causes viral meningitis is contagious and can be spread to other people through close contact, but most people who contract the virus will not develop meningitis.
FUNGAL MENINGITIS This type of meningitis is rare although has a higher prevalence in people with certain types of medical conditions such as diabetes, cancer or HIV. People can get this type of meningitis by inhaling fungal spores from the environment.
PARASITIC MENINGITIS Parasitic meningitis is less common then viral or bacterial meningitis. That being said there are various parasites that can attack the nervous system or the brain in many ways.
AMEBIC MENINGITIS Naegleria fowleris is a free-living microscopic ameba that lives in warm water and soil. Although primary amebic meningoencephalitis (PAM) is very rare, if infected can cause a devastating infection of the brain known as meningococcal disease.
NON-INFECTIOUS MENINGITIS Other things that can cause meningitis include head injury, certain drugs, certain cancers, systemic lupus erythematosus (lupus) and brain surgery.
SYMPTOMS/CAUSES Signs & symptoms in people older than 2 - Sudden high fever - Stiff neck - Severe Headache, different from normal - Headache with nausea/ vomiting - Sensitivity to light - Confusion or difficulty concentrating - Seizures - Sleepiness or difficulty waking - No appetite or thirst - Skin rashes Newborn Signs and symptoms - High fever - Stiffness in the body and neck - Constant crying - Excessive sleepiness or irritability - Difficulty waking from sleep - Inactivity or sluggishness - Not waking to eat - Poor feeding - Vomiting - A bulge spot on top of the babies head
RISK FACTORS Skipping vaccines (adult or childhood vaccination schedule) Age Viral: anyone less than 5 years old Bacterial: anyone less than 20 years old Living in a community setting Pregnancy: Increases the chance of listeriosis which can cause meningitis, still birth or premature delivery Compromised Immune system: AIDs, alcoholism, diabetes, immunosuppressant drugs & removal of the spleen.
COMPLICATIONS The longer the person has the disease without appropriate treatment the more neurological consequences the patient can face such as: Hearing loss Memory loss Learning disability Brain damage Gait problems Seizures Kidney failure Shock Death
PREVENTION Coughing, sneezing, kissing, sharing utensils, a toothbrush or a cigarette may spread the bacteria or viruses responsible for causing meningitis. It is important to take precaution due to those reasons. Preventative actions, such as the following, can be taken: Wash your hands (especially before eating and after using the bathroom) Practice good hygiene (do not share drinks, foods, straws, eating utensils and/or makeup supplies with others) Stay healthy (get rest and maintain a healthy diet) Cover your mouth (when coughing or sneezing) Take extra precaution when pregnant (reduce risk of contracting listeriosis by cooking meat, avoid cheese made from unpasteurized milk)
VACCINATION There are many vaccines that are used to prevent bacterial meningitis: Haemophilus influenza type b (Hib) vaccine Pneumococcal conjugate vaccine (PCV13) Pneumococcal polysaccharide vaccine (PPSV23) Meningococcal conjugate vaccine
MANAGEMENT OF BACTERIAL MENINGITIS
INITIAL MANAGEMENT STEPS Antimicrobial therapy should begin as early as possible, as progression to a more severe disease reduces the patients likelihood of a full recovery. To confirm diagnosis it is important to obtain a blood culture and lumbar puncture. A lumbar puncture is not advised in special populations, such as patients that are immunocompromised, have had a seizure within the last week, have papilledema, and/or a neurological abnormality. A CT scan can be preformed instead in these patients.
EMPIRIC THERAPY Agents used for bacterial meningitis include: Cephalosporins Vancomycin Rifampin Carbapenems Flouroquinolones The agent chosen depends on the patients age, other conditions and should assume antimicrobial resistance. Due to widespread resistance to penicillins and sulfonamides, these newer agents should be used.
RECOMMENDATIONS FOR EMPIRIC THERAPY BASED ON AGE Age Antimicrobial Therapy <1 month Ampicillin plus cefotaxime or ampicillin plus an aminoglycoside 1-23 months Vancomycin plus a third generation cephalosporin 2-50 years Vancomycin plus a third generation cephalosporin >50 years Vancomycin plus ampicillin plus a third generation cephalosporin
EMPIRIC THERAPY + DEXAMETHASONE THERAPY Adjunctive Dexamethasone is used to reduce subarachanoid space inflammatory response. The subarachanoid response plays a big part in morbidity and mortality that is caused by bacterial meningitis. In may be counterproductive to use dexamethasone in patients who are on CSF vancomycin as it may decrease its efficacy. Although the addition of rifampin to the above combination may prove to be effective in patients with suspected pneumococcal meningitis. Patients should be monitored for adverse effects.
WHICH PATIENTS SHOULD RECEIVE DEXAMETHASONE? Neonates: There is only one randomized trial that shows the efficacy of this medication on neonates. The mortality was 22% in the treated group vs 28% in the control group. A follow up examination up to the age of 2 years showed neurological consequences or CNS complications 30% in the treated group vs 39% in the control group. Despite this data, currently there is insufficient information to make a recommendation for this population.
WHICH PATIENTS SHOULD RECEIVE DEXAMETHASONE? (CONT) Infants & Children: There are 15 published trials in this age population, 3 of which are retrospective and the rest are prospective. With all of them being randomized except 1. The first retrospective study involved children with pneumococcal meningitis showed that the use of dexamethasone was associated with hearing loss and neurological complications A recent study showed children that received dexamethasone had higher rates of intubation. It is important to note that most of these studies gave dexamethasone to the patients after antimicrobial therapy and could have caused a decrease in efficacy. The use of the 7-valent pneumococcal conjugate vaccine has significantly dropped the rates of pneumococcal meningitis in children. Currently it is uncertain to determine the efficacy of dexamethasone use in children and infants without further trials.
WHICH PATIENTS SHOULD RECEIVE DEXAMETHASONE? (CONT.) Adults There are 5 published studies of adjunctive dexamethasone in adults with bacterial meningitis. 4 of the 5 trials were inconclusive however 1 of the the trials that were published recently provided important information on the use of this medication on adults. The trial not only showed lower death rates, it also had a lower percentage of unfavorable outcomes. On the basis of this evidence the use of adjunctive dexamethasone is recommended in adults. Recommended dosage: 0.15mg/kg administered every 6 hours for 2-4 days, 10-20 minutes PRIOR to antimicrobial therapy in those suspected or proven with pneumococcal meningitis. Patients that have already received antimicrobial therapy should not take dexamethasone as it does not improve outcomes. Dexamethasone should only be continued if the CSF Gram stain reveals gram-positive diplococci or if blood and CSF cultures are positive for S. pneumonia.
DIAGNOSIS Bacterial etiology may take up to 2 days, there are other methods of diagnosing patients: Gram stain: fast, inexpensive, 60-90 percent accurate (false positives possible, however). Polymerase chain reaction (PCR): can be used to exclude diagnosis and can even be used to determine etiology. Latex agglutination: quick and simple but not recommended for routine use. Limulus lysate assay: sensitive but also not recommended for routine use; also not widely available. Lactate concentration: nonspecific, so it is not recommended either. Procalcitonin concentration: this is useful but not widely available, so it is not recommended. PCR is the most recommended test, as it is more sensitive than viral culture as well as faster than cell culture.
MANAGEMENT Empiric therapy must be initiated and must not be delayed due to pending diagnostic tests. Once a positive CSF gram stain result is obtained, targeted antimicrobial therapy can be initiated in adults. Children continue to receive empiric therapy (vancomycin plus either ceftriaxone or cefotaxime) until blood cultures confirm the diagnosis. If a gram stain is negative, the patient should continue to receive empiric therapy. IV therapy is recommended to ensure that there is adequate concentrations of the drug in the CSF.
MANAGEMENT (CONTD) Modifications can be made to therapy once the pathogen is identified. Patient response determines the duration of therapy, but there are some general guidelines to follow: Neisseria meningitidis or H. Infuenzae: 7 days S. Pneumoniae: 10-14 days Streptococcus agalactiae: 14 to 21 days Aerobic gram-negative bacilli: 21 days Listeria monocytogenes: 21 days or longer If the patient does not respond clinically in 48 hours after initiating therapy, they should be monitored by repeated CSF analysis. Certain patients may be eligible for outpatient therapy, as long as they are closely followed and do not have a fever for 1-2 days.
ANTIMICROBIAL AGENTS Cephalosporins Vancomycin Rifampin Carbapenems Flouroquinolones
ANTIMICROBIAL AGENTS: CEPHALOSPORINS For childhood bacterial meningitis, pneumococcal and meningococcal meningitis that are penicillin-resistant, a 3rdgeneration cephalosporin, Cefotaxime or Ceftriaxone, is recommended . For psuedomonas meningitis, Ceftazidime (Ceptaz) is recommended Another cephalosporin that has shown to be effective is Cefepime (Maxipime) in infants and children as well as patients with bacterial meningitis caused by enterobacter species and pseudomonas aeruginosa.
ANTIMICROBIAL AGENTS: VANCOMYCIN Generally vancomycin is not recommended in patients with bacterial meningitis due to an increase in concerns for penicillin or cephalosporin resistance. Vancomycin should not be used alone; it may be used in combination with a third generation cephalosporin. An intrathecal route may be considered in patients that are not responsive to parenteral administration.
ANTIMICROBIAL AGENTS: RIFAMPIN Rifampin is only recommended in patients that have a delayed response to a pathogen. Rifampin is not to be used alone but in combination with a third-generation cephalosporin with or without vancomycin treatment when dealing with pneumococcal meningitis caused by penicillin or cephalosporin resistant strains.
ANTIMICROBIAL AGENTS: CARBAPENEMS Carbapenems have shown to be successful in treating patients with bacterial meningitis although the set back is that they have potential in causing seizures. Imipenem is more likely to cause a seizure then Meropenem, and can be used as an alternative to cefotaxime and ceftriaxone. Meropenem is also useful in treating meningitis caused by certain gram- negative bacilli.
ANTIMICROBIAL AGENT: FLUOROQUINOLES Fluoroquinolones should be used in patients that are unresponsive, or those that are unable to receive standard therapy, and in those patients that are infected with gram-negative bacilli resistant to many agents. Gatifloxicin and moxifloxacin may be useful but are only as alternative agents. Trovafloxacin is no longer used due to potential liver toxicity side effects.
REFERENCES 1. Cdc.gov. 2021. Meningitis | Home | CDC. [online] Available at: <https://www.cdc.gov/meningitis/index.html> [Accessed 25 Jan 2021]. 2. Mayo Clinic. 2021. Meningitis - Symptoms and causes. [online] Available at: <https://www.mayoclinic.org/diseases-conditions/meningitis/symptoms-causes/syc-20350508> [Accessed 25 Jan 2021]. 3. Smith, L., 2021. Management of Bacterial Meningitis: New Guidelines from the IDSA. [online] Aafp.org. Available at: <https://www.aafp.org/afp/2005/0515/p2003.html> [Accessed 25 Jan 2021]. 4. Vancomycin. In: In Depth Answers [database on the Internet]. Greenwood Village (CO): IBM Corporation; 2017 [cited 2021 Jan 25]. Available from: www.micromedexsolutions.com. Subscription required to view. 5. Clinical Pharmacology [database on the Internet]. Tampa (FL): Gold Standard; 2009 [updated 7 Sept 2008; cited 25 Jan 2021]. Available from: www.clinicalpharmacology.com