Disorders of renal system
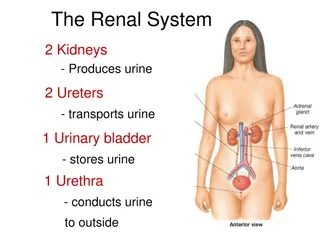
The renal system plays a crucial role in the body's filtration and excretion processes. Learn about the structure and function of the kidneys, including glomerular filtration, tubular reabsorption, and common disorders such as glomerulonephritis. Discover how glomerular changes can manifest in different ways, and understand the significance of hematuria with RBC casts in diagnosing renal issues.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Disorders of renal system Notes about renal system:
25 % of cardiac output goes to kidneys. Kidney is a multilobular structure, composed of up to 18 lobules, each lobule composed of nephrons. Each nephron has a glomerulus that filtrates the blood and a system of tubular structures that selectively reabsorbs and secrets materials. Most absorption occurs tubules and some of it occurs in distal convoluted tubules. Diluting or concentrating countercurrent mechanism in loop of henle which is situated in renal cortex and partly in renal medulla. in proximal convoluted of urine occurs by
The glomerulus: consists of compact tuft of capillaries encased in a thin double layer capsule called Bowman s capsule. The filtration apparatus enclosed by a parietal layer of bowman capsule. Molecules having molecular weight larger than 66,000 can't pass through to the Bowman space. Albumin M.wt is about 66,000. Less than 150 mg/day of proteins found in urine, majority of it formed in tubular epithelium called Tamm- Horsfall glycoprotein (THP).
Disorders of glomerular function: Glomerulonephritis: inflammatory process that involves glomerular structures. Cellular changes in glomerular disease: glomerular disease have been named according to tissue appearance: 1. Proliferative: hypercellular inflammatory process involves infilterating of WBCS and proliferation of glomerular cells. 2. Membranous: abnormal membrane due to antigen-antibody complexes. 3. Sclerotic (fibrosis, connective tissues, collagen): increase in the amount of extracellular material in mesengial, subendothelial or subepithelial tissue of glomerulus. thickening of basement
Glomerular changes can be: Diffuse: involving all parts of glomeruli. Focal: in which only some glomeruli are affected and others are essentially normal Segmental: involving only certain segment of each glomerulus Mesengial: affecting only mesengial cells.
Manifestations of glomerular disease: Hematouria with RBCs casts: the RBCs are intact in urine and after centrifuge they sediment. It differs from hemoglobinurea in that after centrifuge there won't be sedimentation of RBCs. Not all hematouria indicate glomerular damage, because it may be associated with extraglomerular bleeding as in external genitalia disorders, menstrual cycle, bladder injury due to crystals or parasites. The hematouria indicate glomerular damage once we detect RBCs casts, which was formed as: RBCs and proteins pass through the damaged glomeruli and with tamm-horseful they form the casts which are found in urine. The majority of the proteins of the casts are the proteins which passed to renal tubules from glomerulus.
Nephrotic syndrome: It is not a specific glomerular disease, but a constellation of clinical findings that result from an increase in permeability and loss of plasma proteins in urine. The glomerular membrane act as a size specific barrier through which the glomerular filtrate must pass. An increase in permeability allows proteins to escape from the plasma into the glomerular filtrate. There is a compromised permselectivity due to this change, plasma proteins are found in urine in considerable amounts, may be more than (2.5 g/day). The normal value is 150 mg/day or less.
Causes of nephrotic syndrome: 1. 2. 3. 4. 5. 6. 7. 8. 9. Associated with various forms of glomerulonephritis. Systemic disease, such as: D.M. Amyloidosis. Systemic lupus erythrematous.. Renal vein thrombosis. Polyarteritis nodosa. Transplantation rejection Toxins Severe preeclampsia, in some pregnant women Syphilis, malaria and sub-acute endocarditis. Cancer.
Manifestations of nephrotic syndrome: 1. Edema: due to loss of proteins decrease colloidal osmotic compartment. Also, retention due to compensatory increase in aldosterone and stimulation of sympathetic nervous system. 2. Dyspnea: due to pulmonary edema. 3. Patient is vulnerable to infection due to loss of Immunoglobulins and complements pressure sodium of and vascular water
4- Many binding proteins also are lost in the urine. Consequently; the plasma levels of many ions (iron, copper, zinc), hormones (thyroid and sex hormones) may be low because of decreased binding proteins. Many drugs require protein binding for transport. Hypoalbuminemia reduces the number of available protein- binding sites, thereby producing a potential increase in the amount of free (active) drug that is available toxicity may develop. 5- Hypercoagubility: albumin loss in urine albumin compensatory stimulation to the liver to synthesize alpha 2 macroglobulin viscosity rouleaux formation ESR. Alpha 2 macroglobulin is a large protein, larger than fibrinogen, it is M.wt is about (800,000- 1 million).
Pyelonephritis: Pyelonephritis refers to an inflammation of the kidney parenchyma and renal pelvis. There are two forms of pyelonephritis: acute and chronic
Acute pyelonephritis: It represents bacterial infection of the upper urinary tract specifically the kidney parenchyma and renal pelvis. Gram negative bacteria include: Escherichia coli, proteus, Klebsiella, Enterobacter and pseudomonas species; are the most common causative agents. Gram positive includes: Staphylococcus species and Streptococcus faecalis may also cause pyelonephritis, but they are uncommon. There are two routes by which bacteria can gain access to the kidney:
1. From the lower urinary tract ( Ascending infection). 2. Through blood stream (Hematogenous spread). Ascending infection from the lower urinary tract is the most important and common route by which bacteria reach the kidney. Factors contribute to the development of the ascending infections: 1. Outflow obstruction 2. Catheterization and urinary instrumentation 3. Pregnancy 4. Neurogenic bladder.
Factors contribute to the development of hematogenous spread: 1. Septicemia 2. Infective endocarditis 3. Debilitated, chronically ill persons 4. Immunosuppressive therapy.
Manifestations of pyelonephritis: 1. Chill, fever, headache, back pain, tenderness and general malaise. 2. Symptoms of bladder irritation, such as dysuria frequency and urgency. 3. If there is a necrotizing papillae this will implicate sepsis renal failure.
Chronic pyelonephritis: It represents a progressive process. There is scarring and deformation of the renal pelvis, along with atrophy and thinning of the overlying cortex. The disorder involves recurrent or persistent bacterial infection superimposed on urinary tract obstruction, renal reflex or both. Obstruction can be bilateral, caused by urethral obstruction Reflex is the most common cause of chronic pyelonephritis Manifestations of chronic pyelonephritis: 1. Polyuria and nocturia 2. Mild proteinuria
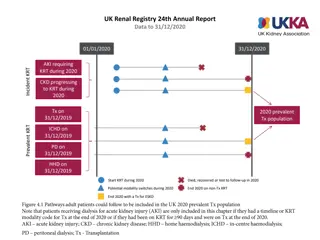
Renal failure: It is of two types : acute (ARF) and chronic (CRF). Acute renal failure: It represents a rapid decline in renal function, so there will be increase in blood levels of nitrogenous wastes and impaired fluid and electrolytes balance Very dramatic decrease in GFR decrease excretion of nitrogenous wastes accumulation of these wastes in (accumulation of nitrogenous nitrogen, uric acid, and creatinine. blood wastes; azotemia urea
Types of acute renal failure: 1. Prerenal acute renal failure 2. Intrarenal acute renal failure 3. Postrenal acute renal failure.
Causes of acute renal failure: Prerenal failure: It is the most common type. Normal kidney can tolerate decreased blood flow before failure occurs. The causes can be: 1- Hypovolemia: like in case of: A. Hemorrhage B. Dehydration C. Excessive loss of fluids from GIT. D. Burns (excessive burns). 2- Decreased vascular filling, like in: A. Anaphylactic shock B. Septic shock
3- Heart failure and cardiogenic shock. 4- Decreased renal perfusion due to vasoactive mediators and diagnostic agents that stimulate intense intrarenal vasoconstriction: A. Drugs B. Bacterial endotoxins C. Radiocontrast agents as those used for cardiac catheterization, cyclosporine (immunosuppressant transplant rejection.) D. Epinephrine E. High dose of dopamine F. An angiotensin- converting enzyme (ACE inhibitors) when combined with diuretics. drug used to prevent
Intrarenal failure: The damage can be either in glomerular cells, tubular cells or interstitium, so the causes can be: A. Acute tubular necrosis B. Prolonged renal ischemia (complication of the prerenal problems). C. Exposure to nephrotoxic drugs D. Heavy metals and organic solvents E. Intratubular obstruction
2- Acute renal disease: A. Acute glomerulonephritis B. Pyelonephritis C. Interstitium nephritis 3- Sepsis: septicemia causes ischemia of the kidney tissue by provoking systemic vasodiltation and internal hypotension. 4- Nephrotoxic agents cause renal injury by inducing varying combinations of renal vasoconstriction, direct tubular damage or intratubular obstruction. Pharmacologic agents that are directly toxic to the renal tubules include: A. Aminoglycosides antibiotics B. Cancer chemotherapeutic drugs as (cisplatin) C. Radiocontrast agents.
Postrenal ARF: Can be caused by: Obstruction of urine flow from the kidney The obstruction can occur in the ureter (calculi or strictures. Bladder (tumor or neurogenic bladder). Urethra as in prostatic hyperplasia and urethritis. The prostatic hyperplasia is the most common cause because the outflow from both ureters must be occluded to produce renal failure.
Manifestations of acute renal failure: 1. Decreased GFR with increase in creatinine and RBC casts in case of glomerulonephritis. Proteinuria (nonselective) Changes in electrolytes balance: sodium/water retention and potassium retention. Metabolic acidosis: due to accumulation of organic acids and this result in respiratory alkalosis as a compensatory mechanism The earliest manifestation is the inability to concentrate urine despite increase in sodium in urine which as result of tubular cells damage. Anorexia, nausea and vomiting Confusion, stupor and convulsions Hypocalcemia and hyperphosphatemia 2. 3. 4. 5. 6. 7. 8.
Hypocalcemia :is due to impaired reabsorption of calcium in the kidney tubules and also may be due to the inability of the kidney to activate vitamin D. Hyperphosphatemia: in renal failure , sustained hyperphosphatemia results in sustained hyperparathyroidisim. The hyperparathyroidisim enhance renal phosphate excretion but also enhance bone resorption, releasing more phosphate into the serum. As renal failure progresses and the ability of the kidney to excrete phosphate continues to diminish, the action of PTH on the bone can exacerbate the already present hyperphosphatemia. Although, there is hypocalcemia, tetany won t occur because the free part of calcium is increased due to acidosis 9- Anemia: due to the toxic effect of urea (intravascular hemolysis), also erythropoiten decrease 10- Generalized bleeding (toxic effect), most dangerous in GIT massive bleeding. 11- Resistance to inflammation will decrease.