ECMO and CRRT Usage Cases and Technical Aspects
The presentation by Dr. Matthew L. Paden explores common indications for concomitant ECMO/CRRT, recent changes in ECMO configurations, and technical aspects of combining ECMO and CRRT. It discusses the importance of fluid management and urine output in neonates on ECMO. The content includes insights on managing pulmonary hypertension and edema in neonates, alongside guidelines from ELSO on fluid volume management.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
ECMO and CRRT Matthew L. Paden, MD Assistant Professor of Pediatric Critical Care Director, Pediatric ECMO
Disclosures Funded by NIH/FDA for CRRT/ECMO device development Everything in ECMO is off label use I m a believer Children s Healthcare of Atlanta | Emory University 2
Objectives Discuss usage cases for concomitant ECMO/CRRT Description of recent common changes in ECMO configurations Discuss technical aspects of concomitant ECMO/CRRT Children s Healthcare of Atlanta | Emory University 3
Common indications Survey of ELSO centers Fluid overload (43%) AKI (35%) Prevention of fluid overload (16%) Electrolyte abnormalities (4%) Fleming GM, et al. ASAIO J 2012. 58(4):407-14. Children s Healthcare of Atlanta | Emory University 4
ECMO and Urine Output 30 consecutive neonates meeting ECMO criteria 18 VV ECMO, 12 conventional management Only looked at first 108 hours Patients who went onto ECMO had: Greater fluid overload Lower UOP Higher BUN Higher creatinine Roy BJ, Cornish JD, Clark RH. Pediatrics 1995;95(4):573-8 Children s Healthcare of Atlanta | Emory University
ECMO and Urine Output Children s Healthcare of Atlanta | Emory University
Neonates on ECMO UCLA 17 consecutive neonates on VA ECMO Hypothesis Pulmonary HTN goes away quickly Pulmonary edema secondary to Starling forces keeps you on ECMO All got diuretics to maintain 3 cc/kg/hour Kelley RE, et al. Journal of Pediatric Surgery, Vol 26(9);1991:1016-1022 Children s Healthcare of Atlanta | Emory University
Neonates on ECMO Results As weight reduces, ECMO flow reduces 120 10.0% 111 cc/kg 9.0% 9.1% 100 Weight Gain (percent) 97 cc/kg 8.0% ECMO Flow (cc/kg) 7.0% 80 73 cc/kg 6.0% 60 5.0% 5.4% 4.0% 30 cc/kg 40 3.8% 3.0% 2.0% 20 2.0% 1.0% 0 0.0% 25% 50% 75% 100% Duration of ECMO Kelley RE, et al. Journal of Pediatric Surgery, Vol 26(9);1991:1016-1022 Children s Healthcare of Atlanta | Emory University
ELSO Guidelines The goal of fluid management is to return the extracellular fluid volume to normal (dry weight) and maintain it there. spontaneous or pharmacologic diuresis should be instituted until patient is close to dry weight and edema has cleared. This will enhance recovery from heart or lung failure and decrease the time on ECLS. As with all critically ill patients, full caloric and protein nutritional support is essential. Children s Healthcare of Atlanta | Emory University 9
ELSO Guidelines The hourly fluid balance goal should be set and maintained until normal extracellular fluid volume is reached (no systemic edema, within 5% of dry weight). Renal replacement therapy use to enhance fluid removal allowing adequate nutritional support is often performed. Despite the literature surrounding fluid overload (>10%) as a risk factor for death, review of the ELSO registry also finds that use of renal replacement therapy is also a risk factor for poor outcome. Even if acute renal failure occurs with ECLS, resolution in survivors occurs in >90% of patients without need for long-term dialysis. Children s Healthcare of Atlanta | Emory University 10
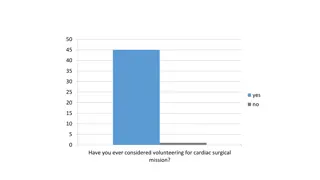
Preventing Fluid Overload How many of you would start CRRT on an ECMO patient with a normal creatinine and no fluid overload? Children s Healthcare of Atlanta | Emory University 11
AKI and ECMO Neonates - 25% (Askenazi 2011) ELSO registry ~8000 non-cardiac neonates Creatinine > 1.5 or RRT Congenital diaphragmatic hernia - 71% (Gadepalli 2011) Congenital hearts - 72% (Smith 2009) Pediatric respiratory - 63% (ELSO DB 2011) Adult cardiac 81% (RIFLE)/85% (AKIN) Note limitations of single center / ELSO database / Different definitions of AKI Children s Healthcare of Atlanta | Emory University 12
CHOA Ped Respiratory ECMO 6/2010-1/2012 Emergency airway for foreign body Cancer APML RSV retroperitoneal hemorrhage Goodpasteur s syndrome Pertussis x 2 Influenza H1N1 Asthma x 2 RSV Cancer ALL Smoke inhalation Wegener s granulomatosis x 2 Near drowning Post-partum ARDS Chronic granulomatous disease Hemophagic lymphohistiocytosis RSV + MRSA Cancer AML Septic shock x 2 Multiple organ failure Pulmonary embolus x 2 Children s Healthcare of Atlanta | Emory University 13
Concomitant ECMO/CRRT Renal Outcomes University of Michigan 35 CRRT/ECMO patients 15 survivors (43%) 14/15 (93%) with full renal recovery at D/C Wegeners ultimately transplanted Children s Healthcare of Atlanta 154 CRRT/ECMO patients - 68 survivors (44%) 65/68 (96%) with full renal recovery at D/C 1 nosocomial enterococcus sepsis at transfer normal 1 month later 2 primary renal disease (Wegeners/polyangiitis) Cr 13.7/6.5 One ultimately transplanted / one with elevated Cr, no RRT Children s Healthcare of Atlanta | Emory University 14
ECMO as a platform Enhances cardiorespiratory stability Reduction of inotropes/vasoactive agents Provides adequate vascular access to allow additional organ support therapies CRRT, plasma exchange, etc. Buys time to allow new approaches/therapies to work Antibiotics, reduction of immunosuppression Concept of organ rest Reduces inflammatory response from lung injury Children s Healthcare of Atlanta | Emory University
New equipment PMP Oxygenators Smaller prime volume Shorter blood path Less pressure drop across the membrane Centrifugal pumps New levitating impeller based designs Continuous flow - afterload dependent Eliminates risk of raceway rupture Risk of negative pressure generation Children s Healthcare of Atlanta | Emory University 16
Change in ECMO Equipment 2002 (Lawson et al. JECT 2004;36:16) 95% roller head, 5% centrifugal 97% silicone, 0% PMP 2008 (Lawson et al. JECT 2008;40:166) 82.5% roller head, 17.5% centrifugal 67% silicone, 14% PMP 2011 (P Rycus, personal communication) 44% roller head, 56% centrifugal 35% silicone, 65% PMP Children s Healthcare of Atlanta | Emory University 17
ECMO pumps Traditional design Roller head pump Complex Positive pressure venous limb ECMO 2.0 Centrifugal pump Simplified Negative pressure Children s Healthcare of Atlanta | Emory University venous limb 18
Traditional design Children s Healthcare of Atlanta | Emory University 19
ECMO 2.0 Children s Healthcare of Atlanta | Emory University 20
CVVH/ECMO In-line Schematic IV pumps Regulate UF production Deliver RF Urometer to measure UF production Inexpensive Inaccurate Children s Healthcare of Atlanta | Emory University
Pediatric ECMO / In-line CRRT Warning IV pumps Sucosky et al., J Med Devices (2), 2008 Your I/O s are not accurate Delivers less replacement fluid than ordered. 10 kg child with 300 mL/hour UF rate negative 288 mL per day (28 ml/kg) 45 kg adolescent with 2000 ml/hour UF rate negative 1.9 L/day (42 ml/kg) Children s Healthcare of Atlanta | Emory University
ECMO/CRRT Traditional Design Schematic POSITIVE VENOUS PRESSURE IV pump/urometer based system hemofilter membrane oxygenator roller pump Commercial CRRT system ECMO bladder Children s Healthcare of Atlanta | Emory University
ECMO 2.0/CRRT Schematic NEGATIVE VENOUS PRESSURE Kidney International. 2009;76:1289 1292. Children s Healthcare of Atlanta | Emory University 24
Managing pressure No CRRT device is FDA approved/designed for use with ECMO Pressure alarms are common Too negative/positive drain pressures Too negative/positive return pressures No uniform solution currently exists Changing/removing alarm parameters Adding flow restriction via tubing/clamps Altering circuit entry points A need exists for a CRRT device designed for use with other extracorporeal devices Children s Healthcare of Atlanta | Emory University 25