Effective Documentation for Healthcare Communication
This content emphasizes the importance of documentation in effective healthcare communication. It covers topics such as the purpose of medical records, mechanics of documentation, and its role in professional liability cases. The significance of accurate and timely charting, professionalism, and the role of medical records in clinical practice are highlighted.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Documentation as an Effective Communication Tool Rebecca Schultz, Director, Risk Management Covenant HealthCare
Disclosures None
Acknowledgement Special thanks to the Risk Management and Patient Safety Institute for their knowledge and willingness to share materials that were used in preparing this program.
Objectives Explore the Purpose of the Medical Record Discuss Uses of Documentation Define Important Mechanics of Documentation Explain How the Medical Record is Used in a Medical Professional Liability Case Review Cases
Hows Your Documentation? Is your charting: Timely? Process oriented? Objective? Concise? How s your spelling & grammar? Do your notes say what you think they mean? Will others understand? The lab test indicated abnormal lover function. Found patient unresponsive. Prayed for him anyway. Skin moist and dry.
Professionalism Documentation and record keeping is a fundamental part of clinical practice. It demonstrates the clinician s accountability and records their professional practice. All documentation will be scrutinized.
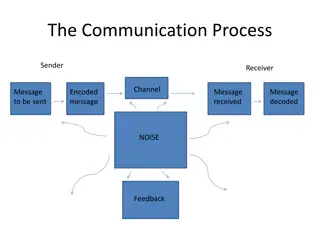
The Medical Record The medical record is meant to be: A complete, accurate, up-to-date documentation of the medical history, condition, and treatment of each patient. The primary means of communication for the healthcare delivery team. Patient centered.
The Medical Record Considered to be an accurate reflection of care provided to the patient, as such it provides data for: Regulatory and accreditation bodies Legal record of the care Quality Reimbursement Risk Management
Why Document? Planning tool Communicate to providers the course of patient s treatment Record changes in condition and response to treatment Provides data Calculation or reimbursement Quality/risk management Protect legal interests
What to Document? Clinically Pertinent Information Assessment Interventions Communications
What to Document? Admission assessment/Assessment of patient s overall condition/Physical & psychosocial status Plan of care/Alteration in plan of care Interventions based upon assessment data Precautionary measures Participation in care rendered by another Patient/Family education & interactions Discharge instructions
Who Should Document? Ordinarily, it is expected that the person who renders the care or treatment documents the information in the medical record.
Mechanics of Documentation Know and follow your organizational and departmental policies Patient centered
Non-Patient Centered Documentation 0730 - Phoned report RN. RN verbalized understanding. 0700 Attempted to call report floor won t take report at this time. 0540 I was off the floor with another patient who needed an emergent CT when I discovered the reach team had been called. 0130 Back from bleeding scan with other patient.
Mechanics of Documentation Know and follow your organizational and departmental policies Patient centered Timely Accurate
Inaccurate Apparently there was some computer error resulting in her being on only Lovenox 30mg daily instead of full dose Lovenox which would be 60 mg every 12 hours.
Mechanics of Documentation Know and follow your organizational and departmental policies Avoid vague terms Patient centered Timely Accurate Brief Objective Chronological Complete
Examples of Vagueness Apparently slept all night Wound drainage is better Patient found in a pool of blood Tolerated diet fair Patient has acceptable ABG s Diprivan mostly effective at 20 mcs Patient complains of chest pain/heartburn/indigestion, antacid given per orders, patient reassured probably just heartburn
Mechanics of Documentation Know and follow your organizational and departmental policies Avoid vague terms Authorized abbreviations Patient centered Timely Accurate Brief Objective Chronological Complete
Abbreviations 01/01/2011 1800: ATM patient c/o B pain w movement and was given medications per order 1CE and stated GUD relief. AAR will reassess @TEOTD and repeat meds AA if needed and AEAP. 01/01/2011 1800: At the moment patient complains of back pain with movement and was given medications per order once and stated good relief. At any rate will reassess at the end of the day and repeat meds again also if needed and as early as possible.
Mechanics of Documentation Know and follow your organizational and departmental policies Avoid vague terms Authorized abbreviations Never chart in advance Patient centered Proper spelling/grammar Timely Avoid jargon Accurate Don t use the medical record as a battleground to air out grudges Brief Objective Chronological Complete
Battlegrounds At the moment patient complains of back pain with movement and was given medications per order once and stated good relief. At any rate will reassess at the end of the day and repeat meds again also if needed and as early as possible. PT was by herself and was attempting to get the patient up for the first time this admission. The RN was not notified of the plan and nor was the patient wearing a gait belt.
Mechanics of Documentation Know and follow your organizational and departmental policies Avoid vague terms Authorized abbreviations Never chart in advance Patient centered Proper spelling/grammar Timely Avoid jargon Accurate Don t use the medical record as a battleground to air out grudges Brief Objective Chronological If it wasn t charted, it wasn t done Complete
Documenting Communication with the Physician Notify the physician promptly regarding a change in the patient s condition and chart: Date Time notified Method of communication What was communicated & all instructions Interventions initiated & patient s response to interventions
Electronic Medical Record Pros Cons All entries dated and timed Open charts Entries readily available for all Privacy of patient information Legibility Copy and pasting forward Easier to collect data Lack of documentation Missing fields Configuration to meet the end users needs Legal Medical Record Issues
What do Attorneys Look For? Lapses in care Inconsistencies and discrepancies Evidence of patient s overall condition and response to treatment Treatments/Procedures performed Medications ordered and given Inappropriate care
A well documented medical record defends itself and the clinician who created it.