Embolism During Pregnancy: Causes, Diagnosis, and Treatment
Embolism during pregnancy, including pulmonary embolism, is a significant concern affecting maternal mortality rates. The leading causes of maternal mortality related to non-cardiovascular diseases, cardiovascular diseases, infection or sepsis, hemorrhage, cardiomyopathy, thrombotic pulmonary embolism, hypertensive disorders of pregnancy, cerebrovascular accidents, amniotic fluid embolism, and anesthesia complications. Proper diagnosis of pulmonary embolism is critical, as overdiagnosis can lead to unnecessary treatments. The risk factors and management of pulmonary embolism, as well as ACOG guidelines for diagnosis, are discussed. Treatment options include LMWH in early pregnancy, unfractionated heparin near delivery and in renal failure, and thrombolytic drugs for hemodynamically unstable cases. It is emphasized to avoid warfarin in pregnant patients due to its teratogenic effects. Venous air embolism, though rare, can also pose a risk during pregnancy.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Robert Nichols, DO Embolism during Pregnancy
Embolism Pulmonary Embolism Venous Air Embolism Amniotic Fluid embolism
Embolism One of the leading causes of maternal mortality Non-cardiovascular diseases, 15.3%. Cardiovascular diseases, 14.7%. Infection or sepsis, 12.7%. Hemorrhage, 11.3%. Cardiomyopathy, 10.8%. Thrombotic pulmonary embolism, 9.0%. Hypertensive disorders of pregnancy, 7.6%. Cerebrovascular accidents, 6.5%. Amniotic fluid embolism, 5.7%. Anesthesia complications, 0.2%. www.cdc.gov/reproductivehealth/maternalinfanthealth/pmss.html
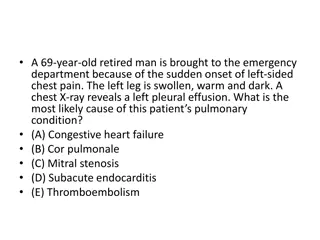
Pulmonary Embolism Difficult diagnosis and management 2 patients at risk Overdiagnosis results in unnecessary and often dangerous treatments to both patients Usual imaging modalities must be considered with developing fetus
Pulmonary Embolism Higher risk 2/2 Virchows triad Hypercoagulability Vascular damage Venous stasis DVT occurs approximately 3x more frequently than PE DVT occurs on left leg in 85% of cases Likely due to compression of iliac vein by iliac artery and gravid uterus Isolated pelvic DVT is also much more common in parturients
ACOG guidelines to diagnosis Pulmonary Embolism Diagnosis often difficult D-Dimer unreliable in pregnant patients Risk of radiation exposure in pregnancy must be considered
Treatment LMWH is treatment of choice in early pregnancy Can be given as outpatient Do not cross placenta and are is not secreted in breastmilk 1mg/kg q12 IV unfractionated heparin preferred near delivery and in renal failure Able to reverse urgently if needed Also does not cross placenta or go into breastmilk Bolus 80u/kg followed by 18u/kg/h, titrated to achieve therapeutic aPTT If SC initial dose is 17,500 units then titrated to aPTT Thrombolytic drugs appropriate in hemodynamically unstable or hypoxic Fetal loss vs. maternal death Warfarin teratogenic and generally contraindicated in pregnant patient
Venous Air Embolism Entrapment of air or medical gases into venous system causing symptoms and signs of pulmonary vessel obstruction 1% of maternal deaths Incidence varies WIDELY depending on the source Depends on surgical position, diagnostic tools
Pathophysiology Vascular access and gradient between injury site and right heart must be present for VAE to occur Determined by rate, volume, duration, patient position, type of gas Pulmonary vessels can filter most air emboli from venous circulation Larger emboli can cause a variety of symptoms
Risk Factors VAE Trendelenburg position Placental abruption Placenta previa Exteriorization of uterus Manual placental extraction Severe preeclampsia Antepartum hemorrhage hypovolemia
Diagnosis Know clinical signs and symptoms May manifest as chest tightness or short breath with or without hypotension or decreased oxygen saturation in conscious patients Variety of diagnositic tools
Treatment Inform Surgeon Adequate hydration Prevent further gas entry Flood surgical field Remove origin of gas entry Increase right atrial pressure and trap air in right atrium Reverse Trendelenburg when possible Left lateral recumbent position Discontinue N2O and ventilate with 100% oxygen Attempt to aspirate air through central line when appropriate Resuscitate Fluid administration Inotropes, vasopressor, pulmonary vasodilators CPR if necessary Hyperbaric oxygen when appropriate
Amniotic fluid embolism 5.7% of pregnancy related deaths in United States in 2011-12 Poorly understood Diagnosis traditionally made at autopsy when fetal squamous cells are found in pulmonary circulation Diagnosis of exclusion Mortality of AFE approaches 80% 50% die within the first hour of onset of symotoms
AFE Pathophysiology Theorized that amniotic fluid and cells enter circulation and trigger anaphylactic reaction Fetal material not always found in patients with AFE and fetal material found in patients who did not trigger anaphylaxis Currently believed that fluid or some other substance enters maternal circulation and triggers anaphylactic reaction OR activates complement cascade OR both. Occurs in 2 phases 1. pulmonary artery vasospasm with pulmonary hypertension and elevated right ventricular pressure which causes hypoxia. Hypoxia causes myocardial and pulmonary capillary damage, left heart failure and ARDS. 2. Those who survive phase 1 have hemorrhagic phase with massive hemorrhage with uterine atony and DIC; however, fatal consumptive coagulopathy may be the initial presentation
AFE risk factors Multiparity Advanced maternal age Male fetus Trauma Abruption Previa Non-Hispanic black women have more than 2x risk of AFE Women with cerebrovascular disease have 25x risk Cardiac disease have 70x risk!
Treatment Supportive Early resuscitation Pulmonary edema common fluid input and output must be closely monitored Left heart failure treated with ionotropes Case reports show successful outcomes with hemodialysis with plasmapheresis and ECMO with intra-aortic balloon pump DIC treated with blood components. Consider activated factor VIIa for severe hemorrhage 2 cases report success with bilateral uterine artery embolization
References Panting-Kemp A, Geller SE, Nguyen T, Simonson L, NuwayhidB, Castro L. Maternal deaths in an urban perinatal network, 1992-1998. Am J Obstet Gynecol. 2000;183:1207-1212. Chan WS, Ray JG, Murray S, CoadyGE, Coates G, Ginsberg JS. Suspected pulmonary embolism in pregnancy: clinical presentation, results of lung scanning, and subsequent maternal and pediatric outcomes. Arch Intern Med. 2002;162:1170-1175. Einstein AJ, HenzlovaMJ, RajagopalanS. Estimating risk of cancer associated with radiation exposure from 64-slice computed tomography coronary angiography. JAMA. 2007;298:317-323 http://www.acog.org/~/media/Districts/District%20VIII/PulmonaryEmbolismPregnancy.pdf?dmc=1&ts=20140525T0200225053 Kim, Chang Seok et al. Venous Air Embolism during Surgery, Especially Cesarean Delivery. Journal of Korean Medical Science23.5 (2008): 753 761.PMC. Web. 28 Mar. 2016. Lim Y, Loo CC, Chia V, Fun W. Recombinant factor VIIaafter amniotic fluid embolism and disseminated intravascular coagulopathy. Int J GynaecolObstet. 2004 Nov. 87(2):178-9. Kaneko Y, OgiharaT, Tajima H, MochimaruF. Continuous hemodiafiltrationfor disseminated intravascular coagulation and shock due to amniotic fluid embolism: report of a dramatic response.Intern Med. 2001 Sep. 40(9):945-7. Hsieh YY, Chang CC, Li PC, Tsai HD, Tsai CH. Successful application of extracorporeal membrane oxygenation and intra-aortic balloon counterpulsationas lifesaving therapy for a patient with amniotic fluid embolism. Am J ObstetGynecol. 2000 Aug. 183(2):496-7. Goldszmidt E, Davies S. Two cases of hemorrhage secondary to amniotic fluid embolus managed with uterine artery embolization.Can J Anaesth. 2003 Nov. 50(9):917-21. Clark SL. Amniotic fluid embolism. Clin ObstetGynecol. 2010 Jun. 53(2):322-8. Fong A, Chau CT, Pan D, et al. Amniotic fluid embolism: antepartum, intrapartum and demographic factors. J Matern Fetal Neonatal Med. 2014 Jun 30. 1-6. Stein PD, Matta F, YaekoubAY. Incidence of amniotic fluid embolism: relation to cesarean section and to age. J Womens Health (Larchmt). 2009 Mar. 18(3):327-9.