Embrace and Innovate Using GP Teaching Capacity Flexibly
A session focusing on reflecting, cogitating, and innovating approaches to Glasgow's GP teaching challenges. Explores solutions such as maximizing existing teaching capacity, recruitment drives, and teaching innovations like virtual tutorials. Discusses the impact of expanding student numbers and increasing GP teaching time on medical school placements and curriculum coverage.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Embrace and Innovate! Using GP teaching capacity flexibly and sustainably Dr Zoe Noonan Prof Lindsey Pope
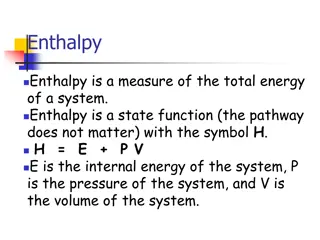
Aims of this session Reflect, cogitate, and innovate! Consider how we have approached this at Glasgow Outline challenges in national GP teaching capacity TRIZ
The good Expanding student numbers Increasing GP teaching time GP placement time can be one of the highlights of medical school. More doctors (more GP s) GP role models offer 1:1 teaching and inspire students into specialty. GP teachers are flexible and adaptable, expert generalists . GP s can deliver pan- specialty and vertical teaching themes.
Challenges to teaching capacity Year 3 at Glasgow: student numbers, (tutor numbers), teaching time (hours) 400 300 200 100 0 2018/19 2019/20 2020/21 2021/22 2022/23 Students GP tutors Teaching time
The bad Expanding student numbers Increasing GP teaching time More work! Administrational issues GPs are a finite resource; is capacity saturated? Logistical challenges for teaching (space) Erosion of quality of teaching More medical schools (competition for placements) Placement time halved ( double bubble of students) Competition from other (MDT) learners Curriculum coverage (dumping ground)
Solutions: maximizing existing teaching capacity Recruitment drive use of social media Personal contact Flexibility with placement days/timings (? Inequitable student experiences) Review of funding National working group (Primary Care Teaching Capacity Group) ? Use of GP trainees for near peer teaching (and role of other MDT members)
Solutions: teaching innovations (so far) Virtual tutorials Virtual (zoom) telephone triage (Agata Dunsmore at Edinburgh) Simulated surgery (?hololens in the future) Online content Isabel platform, bespoke resources Use of Composite Narrative Animation (SMERC grant) to consider psychological wellbeing tutorials delivered by GPs. How much authentic practice-based teaching is enough , what are the alternatives?
Liberating structures:TRIZ Better solutions can be found when diverse range of voices are heard and considered Simple rules that make it easy to include and unleash everyone in shaping the future Help build the organisation you (and other GPs) will want to be a part of Need space for innovation need to get creative destruction TRIZ (from a Russian engineering process) http://www.liberatingstructures.com/6- making-space-with-triz/
Every act of creation is first an act of destruction Pablo Picasso
Terrible result from primary care How can we ensure that there is no positive lifestyle change in our patients? Everything must FAIL e.g.relational/policy/finance No shared decision making - just tell them what to do, remove personal accountability through paternalism Be fatalistic you re doomed Make sure patient never sees their practice team In what way is there a resemblance between what we have just created and what we are currently doing? Be honest. What action would you stop doing to try and change this? Be radical Stopping doing something means you can start doing something else.
Prompts for the Process Individual: How can I reliably ensure there is not enough teaching capacity in general practice? Group: Compare responses Is there anything that we are currently doing that resembles in any shape or form the things on your list? How can you/we stop doing these things? What is your first move? Be as concrete as you can Who else is needed to stop doing this activity?
Reflections on the process What are you going to stop doing or do differently? What did you notice about the process or the pattern of relating with each other? Was this any different to a traditional workshop? Did it help you see the familiar in a different light?
Thank you #UofGWorldChangers @UofGlasgow
References Medical students at Scottish Universities: EQIA. Scottish Government 2019. Accessible at https://www.gov.scot/publications/increasing-number-scotland-domiciled-eu-students- studying-medicine-scottish-universities/pages/3/ The expansion of medical student numbers in the United Kingdom. Medical Schools Council position paper. MSC, 2021. Accessible at https://www.medschools.ac.uk/media/2899/the-expansion-of-medical-student-numbers-in-the-united-kingdom-msc-position-paper-october-2021.pdf The state of medical education and practice in the UK. The workforce report 2022. GMC, 2022. Accessible at https://www.gmc-uk.org/workforce2022 Undergraduate medical education: recommendataions. Scottish Government 2019. Accessible at https://www.gov.scot/publications/undergraduate-medical-education-scotland- enabling-more-general-practice-based-teaching/pages/11/ Cottrell E, Alberti H, Rosenthal J, Pope L, Thompson T. Revealing the reality of undergraduate GP teaching in UK medical curricula: a cross-sectional questionnaire study. Br J Gen Pract. 2020 Aug 27;70(698):e644-e650. doi: 10.3399/bjgp20X712325. PMID: 32784219; PMCID: PMC7425203. Wass VJ, Gregory S, Petty-Saphon K. By choice not by chance: supporting medical students towards future careers in general practice 2016 https://www.hee.nhs.uk/sites/default/files/documents/By%20choice%20-%20not%20by%20chance.pdf Scottish Government. Undergraduate medical education in Scotland: enabling more general practice based teaching2019https://www.gov.scot/publications/undergraduate- medical-education-scotland-enabling-more-general-practice-based-teaching/pages/11