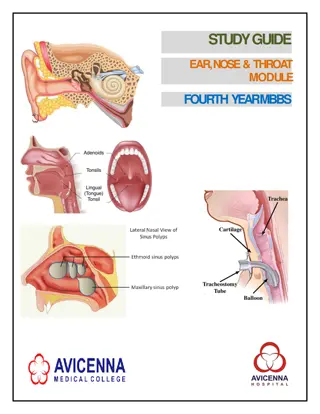
ENT Conditions and Treatments in Primary Healthcare - Updates 2014
Explore the latest updates on ENT conditions and treatments in primary healthcare from 2014, including information on allergic rhinitis, viral rhinitis (common cold), and otitis externa. Learn about available medications, management strategies, and evidence-based recommendations for these common ear, nose, and throat ailments.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
CHAPTER 19: ENT CONDITIONS NATIONAL DEPARTMENT OF HEALTH AFFORDABLE MEDICINES ESSENTIAL MEDICINES PROGRAMME PRIMARY HEALTHCARE 2014 Updates to the 2008 PHC STG & EML
19.1 ALLERGIC RHINITIS Corticosteroid aqueous nasal solution: Directions for use & example of class amended Example of class: The therapeutic agent awarded the contract was budesonide 100 mcg nasal spray. Directions for use: Amended for clarity and correctness. Criterion - 3 monthly review of inhaled corticosteroid: Patients may have continuous OR seasonal allergic rhinitis. Level of evidence: III Expert opinion Contract circular HP07-2014DAI Ref 2 PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014:ENT CONDITIONS 2
19.1 ALLERGIC RHINITIS Chlorpheniramine, oral: retained Cetirizine, oral: retained Loratadine, oral: not added Chlorpheniramine recommended for short term symptomatic use; often prescribed at night (sedative properties). Cetirizine (non-sedating) recommended for severe cases & long term use. Contract award to cetirizine ipo of loratadine. Level of Evidence: III Expert opinion Contract circular HP09-2014SD Ref 2 PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014:ENT CONDITIONS 3 2014
19.1 ALLERGIC RHINITIS Oxymetazoline 0.05%, intranasal: added Nocturnal symptomatic relief for short periods of time. Level of evidence: III Expert opinion PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014:ENT CONDITIONS 4
19.2 VIRAL RHINITIS (COMMON COLD) STG transferred from Chapter 17: Respiratory conditions. PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014:ENT CONDITIONS 5
19.4.1 OTITIS, EXTERNA Topical quinolones:not added Acetic acid 2% in alcohol:retained Kaushik et al s meta-analysis (19 RCTs): No clinically meaningful differences between acidifying agents vs. other topical interventions. Only 1 high quality RCT: acetic acid less efficacious than antibiotic/corticosteroid drops where no symptom resolution within 1 week. Van Balen et al s meta-analysis (2003): Topical antibiotics increased absolute clinical cure rate compared to placebo by 46 % (95% CI 29 to 63 %). No significant difference comparing topical antibiotics vs. antiseptics, or combination antibiotic/corticosteroid preparations. No difference in cure rates between quinolone vs. non quinolone antibiotics. Ideally, topical quinolones should be available for treatment failure with acetic acid. However, irrational use of antibiotics at primary level of care & additional cost implications need consideration. Level of evidence: I,III Systematic review, Expert opinion Kaushik V, Malik T, Saeed SR. Interventions for acute otitis externa. Cochrane Database Syst Rev. 2010 Jan 20;(1):CD004740. van Balen FA, Smit WM, Zuithoff NP, Verheij TJ. Clinical efficacy of three common treatments in acute otitis externa in primary care: randomised controlled trial. BMJ. 2003 Nov 22;327(7425):1201-5. Rosenfeld RM, Singer M, Wasserman JM, Stinnett SS. Systematic review of topical antimicrobial therapy for acute otitis externa. Otolaryngol Head Neck Surg. 2006 Apr;134(4 Suppl):S24-48. Ref 3 PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014:ENT CONDITIONS 6
19.4.2 OTITIS, MEDIA, ACUTE Children Amoxicillin: retained & dose amended Cochrane review: once/twice daily doses of amoxicillin (with/without clavulanate) comparable with three doses for the treatment of acute otitis media in children. Results: Pooled analysis demonstrated the following outcomes: Clinical cure at the end of therapy (RR 1.03, 95% CI 0.99 to 1.07). Clinical cure during therapy (RR 1.06, 95% CI 0.85 to 1.33). Clinical cure at follow-up (RR 1.02, 95% CI 0.95 to 1.09). Clinical cure for recurrent acute otitis media (RR 1.21, 95% CI 0.52 to 2.81). PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014:ENT CONDITIONS 7
19.4.2 OTITIS, MEDIA, ACUTE Children High dose amoxicillin of 90 mg/kg/day recommended for children 3 years of age: Effective against common acute otitis media bacterial pathogens Safe Cheap Has acceptable taste Narrow microbiologic spectrum. Risk factors for resistant S. pneumoniae infections include age ( 2 years) PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014:ENT CONDITIONS 8
19.4.2 OTITIS, MEDIA, ACUTE Children Recommendation: Amoxicillin 45 mg/kg/dose 12 hourly for 5 days. Level of Evidence: I,III Systematic review, Guidelines Updated guideline for the management of upper respiratory tract infections in South Africa: 2014. SAMJ- in press. Thanaviratananich S, Laopaiboon M, Vatanasapt P. Once or twice daily versus three times daily amoxicillin with or without clavulanate for the treatment of acute otitis media. Cochrane Database Syst Rev. 2013 Dec 13;12:CD004975. Piglansky L, Leibovitz E, Raiz S, et al. Bacteriologic and clinical efficacy of high dose amoxicillin for therapy of acute otitis media in children. Pediatr Infect Dis J. 2003;22(5):405 413. Klein JO. Microbiologic efficacy of antibacterial drugs for acute otitis media. Pediatr Infect Dis J.1993;12(12): 973 975] SAMJ, Updated guideline for the management of upper respiratory tract infections in South Africa: 2014, in press. Ref 4 PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014:ENT CONDITIONS 9
19.4.2 OTITIS, MEDIA, ACUTE Adults Amoxicillin: dose not amended (retained as 500 mg 8 hourly for 5 days). Lack of available authoritative guidelines on otitis media in adults - condition mostly presents in children. Target organism is mostly Streptococcus pneumonia, the most virulent with resistance issues. Antibiotic susceptibility studies: 1. NICD GERMS-SA reports (2012,2013): Penicillin susceptible Streptococcus pneumonia isolates (MIC 0.06mg/L) more common amongst older children and adults. Intermediate penicillin resistance (MIC 0.12-1mg/L) mostly presenting in isolates from younger child. Resistance (defined as penicillin MIC 2mg/L) is uncommon. Ref 5 PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014:ENT CONDITIONS 10
19.4.2 OTITIS, MEDIA, ACUTE 2. The European Committee on Antimicrobial Susceptibility Testing (EUCAST) report (2010): For eradication of intermediate resistant Streptococcus pneumonia with amoxicillin: To achieve >90% target attainment rate, time > MIC should be 40% the recommended clinical breakpoint. Dose of 500 mg 8 hourly, time > MIC of 40% was attained 100% of the time for MIC 1mg/L. Probably overcome most resistant isolates with very high doses (1-2 g 8 hourly) - but not advocated for initial empiric therapy. Level of Evidence: III Antibiotic susceptibility studies, Expert opinion NICD GERMS-SA annual report, 2012. NICD GERMS-SA annual report, 2013. European Committee on Antimicrobial Susceptibility Testing. Amoxicillin: Rationale for the clinical breakpoints, version 1.0, 2010. [Online, 2010][Cited,2014] Available at: http://www.eucast.org Ref 6 PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014:ENT CONDITIONS 11
19.4.3 OTITIS MEDIA, CHRONIC, SUPPURATIVE Topical quinolones:not added Not pragmatic for primary care level. Misdiagnosis of TB? Irrational use of antibiotics? The PHC STG recommends referral to secondary level of care, if ear discharge is still present > 4 weeks. (Adult Hospital level STG, 2012 & Paediatric Hospital level STG, 2013 recommends quinolones after dry mopping). Level of evidence: III Expert opinion Adult Hospital level STG, 2012 Paediatric Hospital level STG, 2013 Ref 7 PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014:ENT CONDITIONS 12
19.5 SINUSITIS, ACUTE, BACTERIAL Amoxicillin, oral: duration of therapy course not amended (retained in the STG for duration of 5 days). Meta-analysis of RCTs: Antibiotics should not be prescribed for mild to moderate sinusitis within the 1st week of illness. Avoiding antibiotics for acute sinusitis could reduce antibiotic adverse effects, antibiotic resistance, & cost of healthcare. Cure or improvement 7 -15 days after beginning treatment statistically significantly more common among patients assigned to antibiotics vs. placebo, but differences were small (7% -14% higher rate of improvement with antibiotics). Rate of complications & recurrence did not differ between the 2 groups. Adverse effects of diarrhoea: 80% more common in the antibiotic vs. placebo groups. Level of evidence: I - Meta-analysis Smith SR, Montgomery LG, Williams JW Jr. Treatment of mild to moderate sinusitis. Arch Intern Med. 2012 Mar 26;172(6):510-3. doi: 10.1001/archinternmed.2012.253. Ref 8 PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014:ENT CONDITIONS 13
19.4 SINUSITIS, ACUTE, BACTERIAL Children Amoxicillin: dose amended - Streptococcus pneumoniae is the most common cause of sinusitis. - Aligned with Section 19.4.2 Otitis, media, acute Level of Evidence: III Guidelines, Expert opinion Updated guideline for the management of upper respiratory tract infections in South Africa: 2014. SAMJ- in press. Chow AW, Benninger MS, Brook I, Brozek JL, Goldstein EJ, Hicks LA, Pankey GA, Seleznick M, Volturo G, Wald ER, File TM Jr, Infectious Diseases Society of America. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults.Clin Infect Dis. 2012 Apr;54(8):e72-e112. Ref 9 PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014:ENT CONDITIONS 14
19.4 SINUSITIS, ACUTE, BACTERIAL Adults Amoxicillin: dose not amended - No available RCTs for dose comparisons - recommendations based on distribution of MICs & PK-PD properties of amoxicillin. - US Infectious Diseases Society of America (IDSA) guideline for acute bacterial rhino-sinusitis: - Empirical therapy of standard dose amoxicillin clavulanate (of which the amoxicillin component was either 500 mg 8 hourly or 875 mg 12 hourly). - Among placebo-controlled RCTs in adults (primary inclusion criteria: 7-10 days duration of symptoms) - Clinical benefit of antimicrobial therapy vs. placebo was not prominent - (73% vs 65%; OR, 1.44 [95% CI, 1.24 to 1.68], & NNT of 13). - See susceptibility data (pgs 7, 8) for Streptococcus pneumoniae. Level of Evidence: I,III RCTs, Guidelines, Antibiotic susceptibility studies, Expert opinion Chow AW, Benninger MS, Brook I, Brozek JL, Goldstein EJ, Hicks LA, Pankey GA, Seleznick M, Volturo G, Wald ER, File TM Jr, Infectious Diseases Society of America. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis. 2012 Apr;54(8):e72-e112. Young J, De Sutter A, Merenstein D, et al. Antibiotics for adults with clinically diagnosed acute rhinosinusitis: a meta-analysis of individual patient data. Lancet 2008; 371:908 14. Ip S, Fu L, Balk E, Chew P, Devine D, Lau J. Update on acute bacterial rhinosinusitis. Evid Rep Technol Assess (Summ) 2005: 1 3. Rosenfeld RM, Singer M, Jones S. Systematic review of antimicrobial therapy in patients with acute rhinosinusitis.Otolaryngol Head Neck Surg 2007; 137:S32 45. Falagas ME, Giannopoulou KP, Vardakas KZ, Dimopoulos G, Karageorgopoulos DE. Comparison of antibiotics with placebo for treatment of acute sinusitis: a meta- analysis of randomised controlled trials. Lancet Infect Dis 2008; 8:543 52. Ahovuo-Saloranta A, Rautakorpi UM, Borisenko OV, Liira H, Williams JW Jr, M kel M. Antibiotics for acute maxillary sinusitis in adults. Cochrane Database Syst Rev. 2014 Feb 11;2:CD000243. Ref 10 PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014:ENT CONDITIONS 15
19.4 SINUSITIS, ACUTE, BACTERIAL Penicillin allergy Moxifloxacin: not added - Not rational to add an additional antibiotic specifically for this indication. - The PHC STG recommends that treatment failure requires referral. Level of Evidence: III Expert opinion PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014:ENT CONDITIONS 16
19.6 TONSILLITIS AND PHARYNGITIS First line option Benzathine benzylpenicillin: indicated age group amended Lidocaine 1%: added for reconstitution of benzathine benzylpenicillin - Penicillin is recommended to prevent acute rheumatic fever as a complication of streptococcal pharyngitis in children 3-15 years of age. - Most guidelines recommend treatment for the age group 3-21 years. - The STG includes reconstitution with lidocaine 1% (as recommended in Section 4.9 Rheumatic fever, acute). Recommendations: Benzathine benzylpenicillin recommended for treatment of streptococcal pharyngitis for the age group, 3-21 years of age i.e. children 30 kg and adults . Reconstitution with lidocaine 1% be included in the STG. Level of Evidence: III Guidelines Updated guideline for the management of upper respiratory tract infections in South Africa: 2014. SAMJ- in press. Chow AW, Benninger MS, Brook I, Brozek JL, Goldstein EJ, Hicks LA, Pankey GA, Seleznick M, Volturo G, Wald ER, File TM Jr, Infectious Diseases Society of America. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis. 2012 Apr;54(8):e72-e112. Ref 11 PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014:ENT CONDITIONS 17
19.6 TONSILLITIS AND PHARYNGITIS Second line option Phenoxymethylpenicillin, oral, 12 hourly for 10 days: retained & dosing amended Amoxicillin: not added - 2 studies indicate that once daily amoxicillin is effective, BUT patients with EBV have high risk of developing a rash co-incident with amoxicillin. - Phenoxymethlypenicillin also indicated in the PHC book for prophylaxis against streptococcal infections following rheumatic fever. - Dose aligned with the SAMF (2012) and BNF (2011-2012) for children. Level of Evidence: III Guidelines, Expert opinion Clegg HW, Ryan AG, Dallas SD, et al. Treatment of streptococcal pharyngitis with once-daily compared with twice-daily amoxicillin. Pediatric Inf Dis J 2006; 25: 761-767 Lennon DR, Farrell E, Martin DR, Stewart JM. Once-daily amoxicillin versus twice-daily penicillin V in group A -haemolytic streptococcal pharyngitis. Arch Dis Child 2008; 93: 474-478 SAMF, 2012 BNF for children, 2011-2012 Ref 12 PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014:ENT CONDITIONS 18
19.6 TONSILLITIS AND PHARYNGITIS Penicillin allergy in children Erythromycin: retained & dosing table amended Guidelines recommend macrolides for penicillin-allergy; where supporting evidence is extrapolated from data supporting penicillin. Treatment is recommended from 3 years of age for therapy courses of 10 days. Level of Evidence: III Guidelines Updated guideline for the management of upper respiratory tract infections in South Africa: 2014. SAMJ- in press. Chow AW, Benninger MS, Brook I, Brozek JL, Goldstein EJ, Hicks LA, Pankey GA, Seleznick M, Volturo G, Wald ER, File TM Jr, Infectious Diseases Society of America. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis. 2012 Apr;54(8):e72-e112. Ref 13 PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014:ENT CONDITIONS 19
19.6 TONSILLITIS AND PHARYNGITIS For children < 6 years of age Simple linctus/ tussi infans, oral: deleted Breastmilk/ warm water or weak tea: add sugar or honey and lemon if available:added - Cough linctus - not rational drug use. - STG aligned with IMCI guidelines pertaining to management of a sore throat. Level of Evidence: III Guidelines IMCI Guidelines Ref 14 PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014:ENT CONDITIONS 20 2014
19.6 TONSILLITIS AND PHARYNGITIS Referral criteria Recurrent tonsillitis ( 6 documented episodes/year) for possible tonsillectomy:added as a referral criterion Adapted from the American Academy of Otolaryngology Head and Neck Surgery (AAO HNS ) Guidelines for Tonsillectomy in Children & Adolescents that recommends: Watchful waiting (rather than tonsillectomy) for recurrent throat infection, if < 7 episodes in the past year or < 5 episodes/year in the past 2 years or < 3 episodes/year in the past 3 years. Additional paradise criteria for tonsillectomy: Clinical features (sore throat plus the presence of 1 qualifies as a counting episode: temperature > 38.3 C; or cervical lymphadenopathy (tender lymph nodes or >2 cm); or tonsillar exudate; or positive culture for group A b-hemolytic streptococcus). Treatment with antibiotics had been administered in conventional dosage for proved or suspected streptococcal episodes. Documentation. Level of Evidence: III Guidelines, Expert opinion PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014:ENT CONDITIONS 21
CASE STUDY 15 year old female, presents to the clinic with a cold that has deteriorated. Patient was at the clinic the previous week and was treated for allergic Rhinitis symptoms with chlorphenamine, taken at night. Examination of the nasal passages shows a bilateral purulent nasal discharge , and pain over the sinuses. What would be the best course of treatment? PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014:ENT CONDITIONS 22
CASE STUDY: SOLUTION Check for penicillin allergy. Initiate amoxicillin, oral, 500 mg 8 hourly for 5 days if no allergy, otherwise consider azithromycin weight based dosing. Prescribe paracetamol if pain relief is required. Prescribe oxymetazoline (0.025%), nose drops, 2 drops in each nostril 6 8 hourly for not > 5 days continuously and/or Sodium chloride 0.9%, nose drops, used frequently and in fairly large volumes Question patient on occurrence of infections and consider referral for HIV testing. Counsel patient on when to return to clinic for referral: No improvement in more than 5 days or if fever develops and lasts > 48 hours. Periorbital swelling. Oedema over a sinus. Recurrent sinusitis. PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014:ENT CONDITIONS 23
Slide Ref # Reference 19.1 ALLERGIC RHINITIS 2 1 CORTICOSTEROID AQUEOUS NASAL SOLUTION Contract circular HP07-2014DAI CHLORPHENIRAMINE Contract circular HP09-2014SD 3 2 CETIRIZINE Contract circular HP09-2014SD 19.4 OTITIS 6 3 ACETIC ACID 2% IN ALCOHOL Kaushik V, Malik T, Saeed SR. Interventions for acute otitis externa. Cochrane Database Syst Rev. 2010 Jan 20;(1):CD004740. van Balen FA, Smit WM, Zuithoff NP, Verheij TJ. Clinical efficacy of three common treatments in acute otitis externa in primary care: randomised controlled trial. BMJ. 2003 Nov 22;327(7425):1201-5. 6 3 TOPICAL QUINOLONES Rosenfeld RM, Singer M, Wasserman JM, Stinnett SS. Systematic review of topical antimicrobial therapy for acute otitis externa. Otolaryngol Head Neck Surg. 2006 Apr;134(4 Suppl):S24-48 9 4 AMOXICILLIN Updated guideline for the management of upper respiratory tract infections in South Africa: 2014. SAMJ- in press. Thanaviratananich S, Laopaiboon M, Vatanasapt P. Once or twice daily versus three times daily amoxicillin with or without clavulanate for the treatment of acute otitis media. Cochrane Database Syst Rev. 2013 Dec 13;12:CD004975. Piglansky L, Leibovitz E, Raiz S, et al. Bacteriologic and clinical efficacy of high dose amoxicillin for therapy of acute otitis media in children. Pediatr Infect Dis J. 2003;22(5):405 413. Klein JO. Microbiologic efficacy of antibacterial drugs for acute otitis media. Pediatr Infect Dis J.1993;12(12): 973 975] SAMJ, Updated guideline for the management of upper respiratory tract infections in South Africa: 2014, in press. 10 5 AMOXICILLIN NICD GERMS-SA annual report, 2012. NICD GERMS-SA annual report, 2013. 11 6 AMOXICILLIN NICD GERMS-SA annual report, 2012. NICD GERMS-SA annual report, 2013. European Committee on Antimicrobial Susceptibility Testing. Amoxicillin: Rationale for the clinical breakpoints, version 1.0, 2010. [Online, 2010][Cited,2014] Available at: http://www.eucast.org PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014:ENT CONDITIONS 24
Slide Ref # Reference 19.4 OTITIS 12 7 TOPICAL QUINOLONES Adult Hospital level STG, 2012 Paediatric Hospital level STG, 2013 19.5 SINUSITIS , ACUTE BACTERIAL 13 8 AMOXICILLIN Smith SR, Montgomery LG, Williams JW Jr. Treatment of mild to moderate sinusitis. Arch Intern Med. 2012 Mar 26;172(6):510-3. doi: 10.1001/archinternmed.2012.253. 14 9 AMOXICILLIN Updated guideline for the management of upper respiratory tract infections in South Africa: 2014. SAMJ- in press. Chow AW, Benninger MS, Brook I, Brozek JL, Goldstein EJ, Hicks LA, Pankey GA, Seleznick M, Volturo G, Wald ER, File TM Jr, Infectious Diseases Society of America. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults.Clin Infect Dis. 2012 Apr;54(8):e72-e112. 15 10 AMOXICILLIN Chow AW, Benninger MS, Brook I, Brozek JL, Goldstein EJ, Hicks LA, Pankey GA, Seleznick M, Volturo G, Wald ER, File TM Jr, Infectious Diseases Society of America. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis. 2012 Apr;54(8):e72-e112. Young J, De Sutter A, Merenstein D, et al. Antibiotics for adults with clinically diagnosed acute rhinosinusitis: a meta-analysis of individual patient data. Lancet 2008; 371:908 14. Ip S, Fu L, Balk E, Chew P, Devine D, Lau J. Update on acute bacterial rhinosinusitis. Evid Rep Technol Assess (Summ) 2005: 1 3. Rosenfeld RM, Singer M, Jones S. Systematic review of antimicrobial therapy in patients with acute rhinosinusitis.Otolaryngol Head Neck Surg 2007; 137:S32 45. Falagas ME, Giannopoulou KP, Vardakas KZ, Dimopoulos G, Karageorgopoulos DE. Comparison of antibiotics with placebo for treatment of acute sinusitis: a meta-analysis of randomised controlled trials. Lancet Infect Dis 2008; 8:543 52. Ahovuo-Saloranta A, Rautakorpi UM, Borisenko OV, Liira H, Williams JW Jr, M kel M. Antibiotics for acute maxillary sinusitis in adults. Cochrane Database Syst Rev. 2014 Feb 11;2:CD000243. 19.6 TONSILLITIS AND PHARYNGITIS 17 11 BENZATHINE BENZYLPENICILLIN Updated guideline for the management of upper respiratory tract infections in South Africa: 2014. SAMJ- in press. Chow AW, Benninger MS, Brook I, Brozek JL, Goldstein EJ, Hicks LA, Pankey GA, Seleznick M, Volturo G, Wald ER, File TM Jr, Infectious Diseases Society of America. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis. 2012 Apr;54(8):e72-e112. PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014:ENT CONDITIONS 25
Slide Ref # Reference 19.6 TONSILLITIS AND PHARYNGITIS 18 12 PHENOXYMETHYLPENICILLIN Clegg HW, Ryan AG, Dallas SD, et al. Treatment of streptococcal pharyngitis with once-daily compared with twice-daily amoxicillin. Pediatric Inf Dis J 2006; 25: 761-767 Lennon DR, Farrell E, Martin DR, Stewart JM. Once-daily amoxicillin versus twice-daily penicillin V in group A -haemolytic streptococcal pharyngitis. Arch Dis Child 2008; 93: 474-478 SAMF, 2012 BNF for children, 2011-2012 18 12 AMOXICILLIN Clegg HW, Ryan AG, Dallas SD, et al. Treatment of streptococcal pharyngitis with once-daily compared with twice-daily amoxicillin. Pediatric Inf Dis J 2006; 25: 761-767 Lennon DR, Farrell E, Martin DR, Stewart JM. Once-daily amoxicillin versus twice-daily penicillin V in group A -haemolytic streptococcal pharyngitis. Arch Dis Child 2008; 93: 474-478 SAMF, 2012 BNF for children, 2011-2012 19 13 ERYTHROMYCIN Updated guideline for the management of upper respiratory tract infections in South Africa: 2014. SAMJ- in press. Chow AW, Benninger MS, Brook I, Brozek JL, Goldstein EJ, Hicks LA, Pankey GA, Seleznick M, Volturo G, Wald ER, File TM Jr, Infectious Diseases Society of America. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis. 2012 Apr;54(8):e72-e112. 20 14 BREASTMILK/WARM WATER OR WEAK TEA (WITH SUGAR, HONEY AND LEMON) IMCI Guidelines PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014:ENT CONDITIONS 26