Female Reproductive System Overview: Ovaries to Uterine Tubes
The female reproductive system consists of vital organs like the ovaries, oviducts (fallopian tubes), uterus, and more. Ovaries are female gonads responsible for estrogen secretion and egg production, while the oviducts help in fertilization. The uterus supports fetal development, and other structures like the urinary bladder, urethra, and cervix play crucial roles in waste elimination and childbirth. Understanding the anatomy and functions of these reproductive organs is essential for women's health.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Female Reproductive System (frontal view)
Female Reproductive System 1. Ovary female gonads. Secrete estrogen produces secondary characteristics, menstrual cycle Produces eggs 2 ovaries 4cms long, 2 cms wide
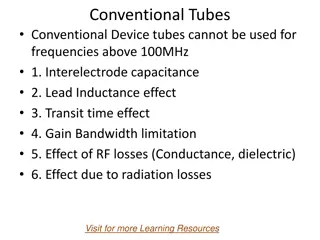
Structure of ovary Fibrous capsule is called tunica albuginea Outer cortex houses developing gametes the oocytes, within follicles Inner medulla is loose connective tissue with largest vessels and nerves 4
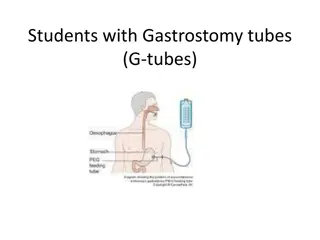
2. Oviduct (fallopian tube) Each ovary is near but not connected to oviduct. Tube with funnel-like opening. Cilia line it to create a current that draws the egg into the tube. Egg is fertilized in the oviduct 3. Uterus thick, muscular, pear-shaped organ. Once egg is fertilized it finishes its development in uterus attached to uterine wall
Female Reproductive System 4. Urinary bladder storage of urine 5. Urethra passage of urine to outside of body 6. Vagina (birth canal) leads to outside of body 7. Cervix narrow neck of uterus 8. Rectum passage for wastes
Uterine Tubes (Fallopian Tubes) Receive the ovulated oocyte and provide a site for fertilization Empty into the superolateral region of the uterus via the isthmus Expand distally around the ovary forming the ampulla The ampulla ends in the funnel-shaped, ciliated infundibulum containing fingerlike projections called fimbriae 7
Uterine Tubes (Fallopian Tubes) Function: events occurring in the uterine tube Fimbriae sweep oocyte into tube, cilia & peristalsis move it along, sperm reaches oocyte in ampulla, fertilization occurs within 24 hours after ovulation & zygote reaches uterus about 7 days after ovulation 8
The Uterine Wall Three basic layers Perimetrium: outer serous membrane Myometrium: middle muscle Endometrium: inner mucosal lining 9
Uterine Histology Endometrium Simple columnar epithelium Stroma of connective tissue and endometrial glands Stratum functionalis: Shed during menstruation Stratum basalis: Replaces stratum functionalis each month Myometrium 3 layers of smooth muscle Perimetrium Visceral peritoneum 10
Vagina Thin-walled tube lying between the bladder and the rectum, extending from the cervix to the exterior of the body Mucosa near the vaginal orifice forms an incomplete partition called the hymen Vaginal fornix: upper end of the vagina surrounding the cervix 11
Female External Genitalia Mons pubis: fatty pad over the pubic symphysis Labia majora & minora: folds of skin encircling vestibule where find urethral and vaginal openings Clitoris: small mass of erectile tissue 12
Female External Genitalia Perineum 13
Bartholins Glands The Bartholin's glands are located on each side of the vaginal opening. They secrete fluid that helps lubricate the vagina.
Ovaries Each follicle consists of an immature egg called an oocyte Cells around the oocyte are called: Follicle cells (one cell layer thick) Stimulated to mature by FSH from the pituitary gland Granulosa cells (when more than one layer is present) Thecal cells: Cells in the ovarian stroma Thecal & granulosa cells work together to produce estrogen
Follicle Development 1. Primordial follicle: one layer of squamous-like follicle cells surrounds the oocyte 2. Primary follicle: two or more layers of cuboidal granulosa cells enclose the oocyte 3. Secondary follicle: has a fluid-filled space between granulosa cells that coalesces to form a central antrum 4. Graafian follicle: secondary follicle at its most mature stage that bulges from the surface of the ovary 5. Corpus luteum : ruptured follicle after ovulation 16
Corpus luteum After ovulation, the remains of the follicle are transformed into a structure called the corpus luteum. If a pregnancy progesterone to maintain the wall of the uterus during the early period of development. occurs, it produces
Corpus albicans If fertilization does not occur, the luteum will begin to break down about 2 weeks after ovulation. corpus Degeneration when fibroblasts enter the corpus luteum and a clump of scar tissue forms called the corpus albicans. occurs
The Menstrual Cycle What is the menstrual cycle? Cycle during which an egg develops and is released from the ovary and the uterus is prepared to receive a fertilized egg Menarche: first menstrual period usually occurs between age 11 and 12 Menopause: time when a woman stops menstruating, usually between 45 & 55 and is no longer able to conceive.
The Ovarian Cycle Follicular phase 1st approx 14 days but variable Egg develops in a follicle Stimulated by FSH Estrogen produced Ovulation Egg released from follicle (LH surge) Egg in abdominal cavity Picked up by fimbria of fallopian tube Not necessarily halfway point Luteal phase Postovulatory phase 14 days (more constant) Corpus luteum develops from exploded follicle Produces progesterone as well as estrogen Progesterone stimulates uterus to be ready for baby If no pregnancy, corpus luteum degenerates into corpus albicans 21
Ovulation Signal for ovulation is LH surge Ovarian wall ruptures and egg released, surrounded by its corona radiata 22
Oogenesis Generation of eggs Starts in fetal period No more oocytes made after about 7th month Developed only to early stage of meiosis I by birth and stops (called primary oocyte) 6-12 primordial oocytes each cycle selected to develop for ovulation (most die) Only then is meiosis I completed Secondary oocyte is then arrested in meiosis II Meiosis II not completed (now an ovum) unless sperm penetrates its plasma membrane Of the 4 daughter cells, only one becomes ovum (needs a lot of cytoplasm) The other 3 become polar bodies
Time: one cycle (approx 28 d.) Pituitary hormones FSH: follicle stimulating hormone LH: luteinizing hormone ovulation * Follicular phase Luteal phase Ovarian hormones Estrogen Progesterone 24
The cyclic changes of uterine wall and follicle (hormone graphs should be above) If no baby, decreasing progesterone - slough Proliferative phase: rebuilds itself after slough Secretory phase: vascular rich glands enlarge: will sustain baby (needs progesterone: corpus luteum initially then placenta) 25
The Menstrual Cycle 1. Menstruation: Loss of egg and uterine tissue via vagina if fertilization does not occur 2. Follicle Stage (follicular stage): lasts 10 days, FSH & LH levels increase, egg matures, follicle secretes estrogen to prepare uterus
The Menstrual Cycle 3. Ovulation: High level of estrogen detected by hypothalamus, increased LH, decreased FSH, follicle bursts egg released 4. Corpus Luteum Stage (Luteal Phase): LH converts follicle to corpus luteum secretes estrogen & progesterone. Progesterone prepares uterus. Increased progesterone keeps LH & FSH low
Days 1-14 Pituitary Gland Produces FSH Follicle Stimulating Hormone Triggers formation of the Follicle Within the ovary Produces Estrogen & Ovum Triggersuterine liningthickening
Days 14 - 28 Pituitary Gland Produces LH Lutinizing Hormone Triggers Ovulation and the formation of the Corpus Lutium Within the ovary Produces Progesterone Continuesuterine liningthickening
Another Way of Looking at Negative Feedback in the Female Reproductive System (Hormones of the Menstrual Cycle) Brain Pituitary gland FSH (causes egg to mature in follicle) LH (causes to egg to be let go = ovulation) ovary Estrogen (causes uterine lining to thicken & build up to prepare for egg) uterus Progesterone (helps maintain uterine lining)
Hormones of Menstrual Cycle What happens if fertilization occurs? Corpus luteum keeps producing progesterone to maintain pregnancy. After 5 weeks the embryo produces progesterone this inhibits LH & FSH so no menstrual cycle What happens if fertilization does not occur? There is no implantation the corpus luteum breaks down. Progesterone level drops, uterine lining breaks down menstruation. FSH & LH are produced again new cycle Average Menstrual Cycle is 28 days long