Framework for Person-Centered Medication Decisions
This highlights the approach to person-centered medication decisions starting with goals of care and organizing interdisciplinary medication reviews. Includes tools, templates, and guidance on special circumstances like antipsychotic use. Emphasizes non-pharmacologic approaches and lessons learned from reducing antipsychotic usage.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
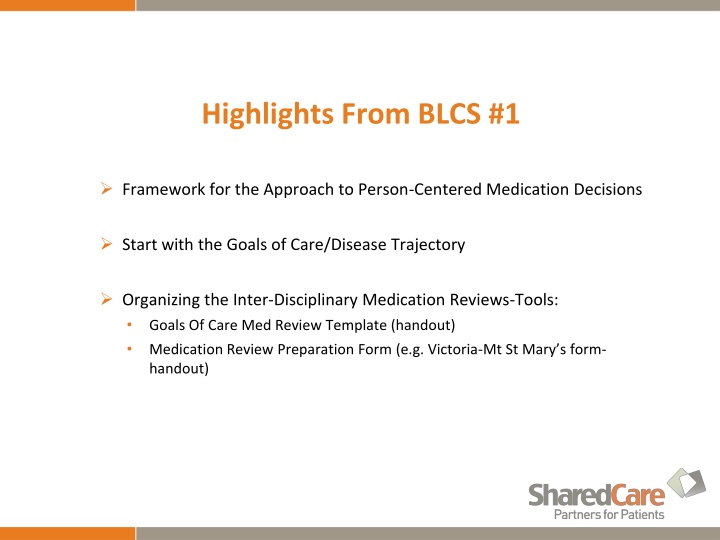
Highlights From BLCS #1 Framework for the Approach to Person-Centered Medication Decisions Start with the Goals of Care/Disease Trajectory Organizing the Inter-Disciplinary Medication Reviews-Tools: Goals Of Care Med Review Template (handout) Medication Review Preparation Form (e.g. Victoria-Mt St Mary s form- handout)
Approach To Person-Centered Medication Decisions Used with Permission-Fraser Health Authority
Set the Context in GOC Symptoms,Function Health Care CG burden Focus on Clinical Issues/Symptoms Agents/Factors Actions Monitoring Plan/Impact of Change (Adapted from Template of Dr. Ted Rosenberg, Victoria, BC)
Special Circumstances-Use of Antipsychotic Polypharmacy Risk Reduction Building Local Capacity and Sustainability Medications Special Circumstances-Use of Antipsychotic Medications Dr. Chris Rauscher
Choosing Wisely Canada- Antipsychotics: Should be prescribed cautiously as they provide limited benefit and can cause serious harm, including premature death. Limited in dementia to (BPSD) cases where non-pharmacologic measures have failed, and where the symptoms either cause significant suffering, distress, and/or pose an imminent threat to the patient or others. A thorough assessment can make use of these medications unnecessary
Non-Pharmacologic Approaches A recent RCT looked at applying person-centered care, med review, social interaction and exercise for the real-world (not needing outside resources) and demonstrated reductions in neuropsychiatric symptoms (NPS), antipsychotic use and mortality but only if the non-pharmacologic approaches could be effectively applied. Am J Psychiatry 2016;173:252-262 7
Agassiz-Our Story . . . . Why listen to us? Because we tried to reduce our use of antipsychotics we failed, we tried again - learning some lessons along the way. 30.00% 25.20% 25.00% 80 % reducti 22.70% 22.30% 20.00% 18% 14.80% 15.00% 10.00% 5.20% 5.00% 4.20% 5.00% 3.10% 0.00% 06/2009 06/2010 06/2011 11/2011 06/2012 11/2012 03/2013 03/2014 11/2014
The results - sustained 30.00% 25.20% 25.00% 22.70% 22.30% Implemented Consent Form 20.00% 18% Stopped and Restarted Antipsychotics 14.80% 15.00% Staff Advisory Committee Education Care Rounds Aromatherapy Music Therapist 10.00% Staff Wellness 5.20% 5.00% 4.20% 5.00% 3.10% 0.00% Rate of antipsychotic use was 6.1 % in May 2016 at Cheam Village. Rate typically varies between 5 and 10%.
What our staff say There is no difference we have the same problems we no longer give them drugs. Why did we give them drugs in the first place? I just don t think about it anymore ! Our DOC commented that in the last year staff at care round have stopped asking about medications - now they never ask
Number of After Hour Calls to Physician 1800 Hours to 0800 Hours From April 2016 to June 2016 1 call no visits 95 Residents (83 Days)
Behaviours that Are Not Likely to Respond to Medications E. Drance & C. Ward Physician Workshop 2016
P.I.E.C.E.S. 3-Question Template Q. 1 What has changed? Avoid assumptions; think atypical. Q. 2 What are the RISKS and possible causes? Think P.I.E.C.E.S. Q. 3 What is the action? Interventions Interactions Information P.I.E.C.E.S. 6th Ed.
Q2. What are the RISKS and possible causes think P.I.E.C.E.S.? P - Physical I - Intellectual E - Emotional C - Capabilities E - Environment S - Social Think Triggers (Antecedents) P.I.E.C.E.S. 6th Ed. E. Drance & C. Ward Physician Workshop 2016
The Physicians role Asking relevant questions regarding: What is the number one problem you need help with? Encourage use of PIECES assessment and BPSD Algorithm Diagnosis and Treatment (look for untreated medical conditions) Medication Review/Review for Polypharmacy Appropriate Prescribing when and why? Consent Therapeutic Trial Taper & Discontinuation E. Drance & C. Ward Physician Workshop 2016
CLeAR Results from Wave 2 Overall decrease from 33% (Sept 2015) to 28% (Dec 2016) Existing residents: By the end of CLeAR, 709/895 residents (79%) had their antipsychotics discontinued or reduced (44% discontinued; 35% reduced) Newly-admitted residents: -562/1198 residents (43%) were admitted onantipsychotics -292/562(52%) had their antipsychotics discontinued or reduced (27% discontinued; 25% reduced Nov 2016
Current Desired Areas to discuss Setting Up/Scheduling How to achieve Family involvement/ Goals of Care Team involvement/ Having required info F/U-Monitoring and Review Other
91 Y.O. Woman-Moderate Dementia Drug Reconciliation Problems Identified at the Review - Dementia MMSE 11; Functional Review - Engages with family and will speak with some paraphrasia - will do a.m. care with standby - Toilets self - Can find and walk to common area and dining room - Still feeds self MedicationsIndications Oxazepam 30mg - Insomnia Galantamine 16mg Dementia Risperidone 0.5mg BID Agitation/Aggression/Paranoia Citalopram 20mg Depression, irritability Felodipine 10mg HTN HCTZ 25mg TN Atorvastatin 20mg Hyperlipidemia (no IHD/CVA) Ecasa-81mg od Primary Prevention stroke and MI Metformin 1000mg BID DM Allopurinol 300mg Gouty arthritis Alendronate, Ca, Vit. D Osteoporosis Behaviour no reported problems, some anxiety at pill time - Unsteady, Forgets to use walker - Anorexia, Poor intake, Weight loss 5 lbs. dermatitis Other Clinical findings BP -124/64 sitting and 106/60 standing HGB -104 ;Ferritin 30 A1C 5.5 GFR 54 - Constipation - Edema - +3 with some stasis - Caregiver Stress - husband and daughters exhausted Goals of Care: QofL, maintain function, control symptoms, not survival , expected life expectancy <2 years
Set the Context in GOC Symptoms, Function Health Care CG burden Focus on Clinical Issues/Symptoms Agents/Factors Actions Monitoring Plan/Impact of Change (Adapted from Template of Dr. Ted Rosenberg, Victoria, BC)
GOC Outcomes Symptoms, Function Health Care CG burden Focus on Clinical Issues/Symptoms Agents/Factors Actions Monitoring Plan/Impact of Change Fall, Orthostatic BP BP meds, CNS meds Stop (taper): Felodipine, HCT; Stop: Naproxen Reduce: Citalopram 10mg OD, Respiridone 0.25mg OD, Oxazepam 7.5mg BP: 146/72 Balance better, no falls Mood stable Sleeping OK Edema BP meds Stop (taper): Felodipine, HCT Edema +1 Anorexia, Nausea, Swallowing, Anemia Calcium, Alendronate, Atorvastatin, ASA, Metformin, Allopurinol, Galantamine Stop: Ca, Alendronate, Atorvastatin, ASA Reduce: Metformin, Allopurinol Galantamine re-started Add Fe Gluc. Appetite and weight up Hb 136 Constipation Calcium Stop Calcium Less laxative Reduced GFR Naproxen Allopurinol Stop Naproxen Reduce Allopurinol Inc. GFR Pill Burden All meds As above Reduced pill burden Used with permission from Dr. Ted Rosenberg, Victoria, BC