Gestational Trophoblastic Disease
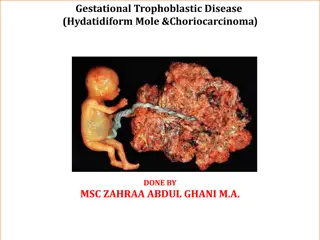
Gestational Trophoblastic Disease (GTD) is a spectrum of proliferative abnormalities associated with pregnancy. It includes Hydatidiform Mole, Invasive Mole, Choriocarcinoma, and Placental site trophoblastic tumor (PSTT). The incidence varies across countries, with different types and etiologies contributing to its development. GTD is characterized by changes in chorionic villi, and factors such as maternal age, nutrition, and immune mechanisms play a role. Understanding the pathology, types, and etiology of GTD is essential in its management.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
GESTATIONAL TROPHOBLASTIC DISEASE
DEFINITION Gestational Trophoblastic Disease(GTD) encompasses a spectrum of proliferative abnormalities of Trophoblastic associated with pregnancy Persistent GTD is referred as Gestational Trophoblastic Neoplasia(GTN)
Conventional Histological Classification Hydatidiform Mole(Complete and partial) Invasive Mole Choriocarcinoma Placental site trophoblastic tumor(PSTT)
DEFINITION It is an abnormal condition of the placenta where there are partly degenerative and partly proliferative changes in the young chorionic villi Cluster of small cyst Benign with malignant potential
INCIDENCE Philippines 1 in 80 India 1 in 400 USA 1 in 2000
TYPES COMPLETE INCOMPLETE
ETIOLOGY Exact cause is unknown Highest in teenage pregnancies and women over 35 years of age Prevalence vary with race and ethnic origin Faulty nutrition
ETIOLOGYContd Disturbed maternal immune mechanism Chromosomes are derived from the father H/O hydatidiform mole increase the chance of recurrence
PATHOLOGY Disease of the CHORION Death of the ovum or Failure of the embryo to grow Hydatidiform mole (Cyst begin to form from 3rdto 5thweek, when feto-maternal circulation has become established)
PATHOLOGY.Contd HYDATIDIFORM MOLE Secretions from hyperplastic cells and Transferred substances from the maternal blood Accumilation of these substances in the stroma of the villi(which are devoid of blood vessels) Distension of the villi to form small cyst
NAKED EYE APPEARANCE Mass filling in the uterus Mass is made up of clusters of cyst of varying size No trace of embryo or amniotic sac
MICROSCOPIC APPEARANCE Marked proliferation of syncitial and cyto- trophoblastic epithelium Thinning of stromal tissue due to accumulation of fluid Absence of blood vessels Villus pattern is distinctly maintained
OVARIAN CHANGES Increased HCG Bilateral leuteal cyst (Increased HCG,P,E) Regress 2 months after expulsion of mole
CLINICAL FEATURES AGE AND PARITY Prevalent amongst teenaged and elderly H/O amenorrhoea 8-12 weeks
CLINICAL FEATURES..Contd SYMPTOMS Vaginal bleeding Varying degree of lower abdominal pain Over distension of the uterus Concealed haemorrhage Perforation of the uterus Infection Uterine contraction to expel the content
CLINICAL FEATURES..Contd Constitutional symptoms Patient becomes sick Excessive vomiting Breathlessness Thyrotoxic feature Expulsion of grape like vesicles per vaginum is diagnostic H/O quickening absent
CLINICAL FEATURES..Contd SIGNS Feature of early pregnancy Patient looks more ill Pallor out of proportion to visible blood loss Features of pre eclampsia
CLINICAL FEATURES.Contd PER ABDOMEN Size of the uterus is more than the period of amenorrhoea Feel the uterus doughy Fetal parts are not felt No fetal movement Absence of FHS
CLINICAL FEATURES.Contd VAGINAL EXAMINATION Internal ballottement cannot be elicited Unilateral or bilateral enlargement of the ovary Finding vesicles in the vaginal discharge Cervical os open
INVESTIGATIONS Full blood count, ABO and Rh Hepatic, renal and thyroid function test Sonography Snow storm appearance HCG 1 in 200 to 1 in 500 X-Ray abdomen- No fetal shadow X-Ray chest Pulmonary embolism
COMPLICATIONS Haemorrhage and shock Seperation Perforation Evacuation Infection No membranes Degenerated vesicles Lowered resistance Increased operative interference
COMPLICATIONS..Contd Perforation of the uterus Dilatation and evacuation Perforating mole Pre eclampsia with convulsion Coagulation failure Acute pulmonary insufficiency 4-6 hours following evacuation LATE Choriocarcinoma
MANAGEMENT PRINCIPLE 1. To restore the blood loss 2. To evacuate the uterus 3. To minimise infection
MANAGEMENTContd PATIENT CLASSIFICATION GROUP A Mole is in the process of expulsion GROUP B Uterus remain inert
MANAGEMENTContd SUPPORTIVE THERAPY GROUP A Morphine 15mg IM 5% Dextrose Blood transfusion GROUP B Blood should be kept ready prior to elective evacuation
MANAGEMENTContd DEFINITIVE MANAGEMENT GROUP A S/E or D/E Oxytocin 10-20 units in 500 ml 5% dextrose 40-60 drops/minute Digital exploration and removal of ovum under GA using ovum forceps Methergin 0.2mg IM GROUP B Blood should be kept ready prior to elective evacuation Slow dialatation of the cervix followed by suction and evacuation
COMPLICATIONS OF VAGINAL EVACUATION Injury to the uterus Haemorrhage Shock Acute pulmonary insufficiency Thyroid storm
COMPLICATIONS OF VAGINAL EVACUATION Injury to the uterus Haemorrhage Shock Acute pulmonary insufficiency Thyroid storm
INDICATIONS FOR HYSTERECTOMY Patient with age over 35yrs Completed family irrespective of age Uncontrolled haemorrhage or during surgical evacuation Reduces the risk of GTN
INDICATIONS FOR HYSTEROTOMY Profuse vaginal bleeding Cervix unfavourable Accidental perforation of the uterus following surgical evacuation