Glycogen Metabolism: An Insight into Carbohydrate Storage Processes
Explore the intricate processes of glycogen metabolism, including glycogenesis and glycogenolysis, shedding light on the formation and breakdown of glycogen in animal cells. Delve into the roles of key enzymes such as glycogen synthase and the significance of glycogen as a major carbohydrate storage form. Discover the sites, importance, and mechanisms involved in glycogen metabolism, providing a comprehensive view of how cells utilize and regulate glycogen for energy maintenance.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
CHO CHO METABOLISM METABOLISM ( (GLYCOGEN GLYCOGEN METABOLISM METABOLISM) ) By ShuzanAli Mohammed Ali Assist. Prof. of Medical Biochemistry & Molecular Biology 4/17/2025 12:34 AM shuzan.ali@fmed.bu.edu.eg 1
GLYCOGEN METABOLISM Glycogen is the major storage form of carbohydrates in animal cells. Its metabolism involves two processes. I- Glycogenesis: (Glycogen formation). II- Glycogenolysis: (Glycogen breakdown). 4/17/2025 Shuzan.ali@fmed.bu.edu.eg 2
I. GLYCOGENESIS Definition: It is the formation of glycogen from or (Glucose or other hexoses Glycogen) Site: It occurs in the cytosol of cells (except RBCs) specially in liver & muscles. Importance: Storage of excess glucose, or other hexoses taken in food. Glucose Other hexoses 4/17/2025 Shuzan.ali@fmed.bu.edu.eg 3
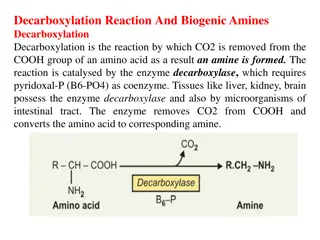
H H H O P OH OH H H C C H O P C OH OH C C C C ADP ATP H C OH H C OH H OH ADP HO Phosphoglucomutase ATP H C OH Mg++ H C OH O H C C OH H HO C H C H Phosphoglucomutase HO O O Mg++ HO C Glucokinase H HO OH C H HO H C C H OH O O O H C OH H C Glucokinase hexokinase H C OH H C OH H C C OH H C H C H H C H C H C CH2OH CH2OH CH2O P CH2OH CH2O P CH2OH Glucose Glucose-6-phosphate Glucose-6-phosphate Glucose-1-phosphate Glucose-1-phosphate Glucose UTP UTP UDP-Glucose UDP-Glucose Pyrophosphorylase Pyrophosphorylase PPi PPi UDP UDP UDP UDP H O O H O O H H UDPG acts as a substrate for CHO UDP C C C CHO C UDP H2O H2O H NAD+ NAD+ 2 NADH H+ + + 2 2 NADH H+ C glycogen synthesis. OH 2 H OH H C H C C OH OH H C OH C OH H HO C H HO H C H O O HO HO C C H H O O HO C H HO C UDPG-Dehydrogenase UDPG-Dehydrogenase H C OH H C OH H C C OH OH H C OH H C OH H H C OH H C H C C H C OH H C H COOH COOH CH2OH CH2OH COOH COOH D-Glucuronic acid UDP-Glucose UDP-Glucose UDP-Glucuronic acid UDP-Glucuronic acid D-Glucuronic acid NADPH H+ + NADPH H+ + 4/17/2025 Shuzan.ali@fmed.bu.edu.eg 4 NADP+ NADP+ COOH CH2OH CH2OH CH2OH NADPH H+ CH2OH CH2OH NADPH H+ COOH NADP+ + + CH2OH HO H C H NADH H+ + NADH H+ NAD+ NAD+ NADH H+ C O NADP+ + C O HO C H + HO C HO C H + NADH H+ NAD+ NAD+ H C OH C O H C OH H C OH H C O HO C H C OH HO C H CO2 H H C OH H C OH HO C C H H C OH OH OH H C HO OH C H H C CH2OH C CO2 H OH CH2OH H CH2OH OH CH2OH HO C H C HO C H D-Xylulose CH2OH L-Xylulose CH2OH Xylitol CH2OH L-Gulonic acid CH2OH in lower animals Not in human or guinea pigs in lower animals Not in human or guinea pigs L-Xylulose D-Xylulose Xylitol L-Gulonic acid L-Ascorbic acid HMP-Shunt The Uronic Acid Pathway L-Ascorbic acid HMP-Shunt The Uronic Acid Pathway
I. Glycogen synthase(the key enzyme): Ittransferglucose from UDPG to a glycogen primer forming 1,4-glucosidic bonds between C1 of activated glucose of UDP-G & C4 of a terminal glucose residue of glycogen, liberating UDP. Glycogen synthase function is to elongate short branches in the glycogen tree up to 12 glucose units. 4/17/2025 Shuzan.ali@fmed.bu.edu.eg 5
A preexisting glycogen molecule or glycogen primer must be present to initiate this reaction. Glycogen may in turn be formed on a primer known as glycogenin (37-kDa protein, glycosylated on a specific tyrosine residue by UDP-G). Further glucose residues are attached in the 1 4 position to make a short chain that is a substrate for glycogen synthase. 4/17/2025 Shuzan.ali@fmed.bu.edu.eg 6
II. The branching enzyme: Ittransfers some glucose units from the end of a long branch to one of glucose units in the middle of an adjacent long branch forming 1,6-glucosidic bond. A new branch appears on which glycogen synthase can act again. 4/17/2025 Shuzan.ali@fmed.bu.edu.eg 7
Biosynthesis of glycogen (Glycogenesis) Glycogen primer 4/17/2025 Shuzan.ali@fmed.bu.edu.eg 8
Regulation of glycogenesis: Glycogen synthase is the key enzyme. 1. Covalent modification: Glycogen synthase is present in 2 forms: Glycogen synthase a (activedephosphorylated) Glycogen synthase b (inactivephosphorylated) 4/17/2025 Shuzan.ali@fmed.bu.edu.eg 9
Hormonal regulation of glycogenesis Adrenaline (in muscle and liver) Glucagon ( in liver only ) Insulin Adenyl cyclase Phosphodiesterase ATP cAMP AMP Protein Kinase ATP ADP P Glycogen Synthase (b) (inactive) Glycogen Synthase (a) (active) P P Pi H2O Phosphatase Insulin Diagrammatic representation of hormonal control of Glycogenesis 4/17/2025 Shuzan.ali@fmed.bu.edu.eg 10
2. Induction & repression of the key enzyme: CHO feeding induce insulin synthesis of Glycogen synthase, glycogenesis is stimulated. Fastingdecreases insulin & increases anti-insulin decrease synthesis of Glycogen synthase & glycogenesis is inhibited. 4/17/2025 Shuzan.ali@fmed.bu.edu.eg 11
3. Allosteric Regulation: Glycogen synthase is allosterically activated by G-6-P and allosterically inhibited by glycogen. CHO feeding increase insulin so increase glycogenesis. Fasting decrease insulin and increase anti- insulin and inhibit glycogenesis. 4/17/2025 Shuzan.ali@fmed.bu.edu.eg 12
117 4/17/2025 Shuzan.ali@fmed.bu.edu.eg 13
I. GLYCOGENOLYSIS Definition: It is the breakdown of glycogen into glucose or glucose 6- phosphate Site: It occurs in the cytosol of cells (except RBCs) specially in liver & muscles. Importance: 1. In liver: supplies blood glucose during fasting less than 18 hours. 2. In muscles: source of energy during exercise. 4/17/2025 Shuzan.ali@fmed.bu.edu.eg 14
Steps: 1. The key enzyme (Glycogen phosphorylase) catalyzes removal of glucose residues from outermost chains in the form of G-1-P until 4 glucose units on either side of -1,6 branching point. 2. Then 1 , 4 - glucan transferase transfers a trisaccharide unit from one side to the other. 3. Debranching enzyme catalyzes hydrolytic splitting of -1, 6 bond; phosphorylase can act again. 4/17/2025 Shuzan.ali@fmed.bu.edu.eg 15
Glycogen Phosphorylase is the key enzyme. 4/17/2025 Shuzan.ali@fmed.bu.edu.eg 16
G-6-Phosphatase: It is present in liver, kidneys & intestines. It is not present in muscles. Liver glycogen can give glucose to blood, but Muscle glycogen cannot give glucose to blood directly (may give it through Cori s cycle & Glucose-alanine cycle). . 4/17/2025 Shuzan.ali@fmed.bu.edu.eg 17
Regulation of glycogenolysis: Glycogen phosphorylase is the key enzyme. 1. Covalent modification: Glycogen phosphorylase is present in 2 forms: Glycogen phosphorylase a (activephosphorylated) Glycogen phosphorylase b (inactivedephosphorylated) Inactive phosphorylase (b) is converted to active phosphorylase (a) by phosphorylase (a) kinase, with ATP as phosphate donor. Inactive Phosphorylase (b) kinase is activated to phosphorylase (a) kinase by cAMP dependent protein kinase A requires cAMP for its activity. 4/17/2025 Shuzan.ali@fmed.bu.edu.eg 18
4/17/2025 Shuzan.ali@fmed.bu.edu.eg 19
2. Induction & repression of the key enzyme: CHO feeding induce insulin decrease synthesis of glycogen phosphorylase so glycogenolysis is inhibited. Fasting decreases insulin & increase anti- insulin increase synthesis of glycogen phosphorylase so stimulated. glycogenolysis is 4/17/2025 Shuzan.ali@fmed.bu.edu.eg 20
3. Allosteric Regulation: Muscle phosphorylase is allosterically activated by AMP which is increased during muscular exercise. CHO feeding increase insulin leading to inhibition of glycogenolysis. Fasting decrease insulin & increase anti- insulin stimulation of glycogenolysis. 4/17/2025 Shuzan.ali@fmed.bu.edu.eg 21
The lactic acid (Coris) cycle: In contracting muscle; Glycogen gives G-6-P which by glycolysis gives lactate as there is no O2. Lactate diffuses to blood and goes to the liver, where lactate is converted to glucose by gluconeogenesis. Glucose can return back to muscles 4/17/2025 Shuzan.ali@fmed.bu.edu.eg 22
Glucose-alanine cycle: If pyruvicacidin muscle is changes to alanine by transamination, it goes to blood then to liver where alanine is changed again transamination. By gluconeogenesis, alanine gives glucose which diffuses from liver to blood to contracting muscle again to supply energy. to pyruvic by 4/17/2025 Shuzan.ali@fmed.bu.edu.eg 23
The lactic acid (Cori) cycle and glucose-alanine cycle 4/17/2025 Shuzan.ali@fmed.bu.edu.eg 24
Difference between liver glycogen and muscle glycogen Liver Glycogen Amount 5% =100 gm (liver ~ 2 KG) Source Dietary hexoses by glycogenesis Gluconeogenesis Function - Source of blood glucose (G-6-Ptase) Points Muscle Glycogen 1% =300 gm (muscles~ 30 Kg) Blood glucose by glycogenesis - Source of energy to muscle does NOT give blood glucose except through Cori s or glucose-alanine cycle - Little effect by diet - Not reduced by fasting . - Markedly reduced - Dimer (each monomer contains 1 mol. of PLP) - Allosterically + by AMP Increase No effect Decrease Decrease -Source of energy to liver -Increased by diet -Reduced by fasting - Not reduced - Monomer - No PLP (no vit B6) - Not affected by AMP Increase Decrease Decrease Decrease Feeding Status By Exercise Glycogen Phosphorylase Insulin Glucagon* Adrenaline Thyroxin 4/17/2025 Shuzan.ali@fmed.bu.edu.eg 25
GLYCOGEN STORAGE DISEASE ( GLYCOGENEOSIS) Definition: Inborn errors of glycogen metabolism caused by deficiency of one of enzymes of glycogenesis or glycogenolysis in different tissues. Characterized by deposition of: 1. abnormal type or 2. abnormal quantity of glycogen in tissues mainly in the liver and muscle. 4/17/2025 Shuzan.ali@fmed.bu.edu.eg 26
Glycogenosis Disease Deficient Enzyme & Manifestations Type I Von Gierke s disease Glucose-6-phosphatase, enlarged liver & kidney. uric acid, lactic acid, cholesterol, lipid & ketone bodies, Fasting hypoglycemia Type II Pompe s disease Lysosomal glucosidase enzyme in all organs. Fatal in early life. Type III Limit dextrinosis or Cori disease Debranching enzyme in liver and muscle. Glycogen has short branches Type IV Amylopectinosis (Andersen disease) Branching enzyme in liver. Glycogen has few long branches like amylopectin. Type V Mc Ardle s syndrome Muscle phosphorylase. Muscles become weak after a short exercise (little or no lactate in bl. after exercise) Type VI Her s disease Liver phosphorylase (enlarged liver by glycogen) Type VII Tarui s disease Phosphofructokinase in muscle and RBCs. (as type V plus hemolytic anemia) Type VIII Liver phosphorylase kinase Type IX Liver and muscle phosphorylase kinase Type X cAMP-dependent protein kinase A 4/17/2025 Shuzan.ali@fmed.bu.edu.eg 27
Type I glycogenosis (Von Gierkes disease) Cause: deficiency of G-6-phosphatase in liver & kidneys accumulation of large amounts of glycogen in liver & kidneys. Manifestations: 1- Enlargement of liver and kidney (glycogen accumulation) 2- Fasting hypoglycemia: liver G-6-P cannot leave the liver. 3-Hyperlipemia & hypercholesterolemia: lipids is the metabolic fuel. There is increased lipolysis (increased FFA in plasma) increased ketogenesis metabolic acidosis. 4- Hyperuricemia (gout): due to increased HMP shunt increased ribose-5-P stimulation of de novo synthesis of purines increased uric acid formation 5- Lactic acidemia: the liver cannot form glucose from lactate (no Cori s cycle) which leads to acidosis. 4/17/2025 Shuzan.ali@fmed.bu.edu.eg 28
4/17/2025 Shuzan.ali@fmed.bu.edu.eg 29