Guide for New Medical Staff: Quality and High Reliability Organizations
"Discover the essentials of quality healthcare and high reliability organizations in this introductory guide for new medical staff. Learn about committee structures, achieving zero harm, characteristics of HROs, quality reporting requirements, and hospital promoting interoperability."
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
QUALITY AND YOU An Introductory GUIDE for New Medical Staff
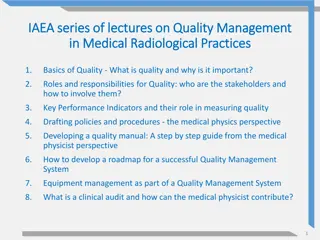
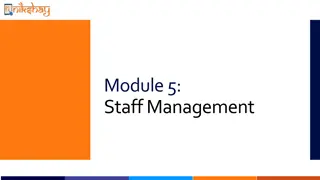
Committee Structure / HRO QUALITY REPORTING STRUCTURE
Deference to Expertise Sensitivity to Operations SJ/C System Board SJH / CH Board Professional Relations Committee Quality Analysis Implementation Committee (QAIC) Risk EOC Management Committee Committee Infection Prevention Patient Safety Committee Medical Executive Committee Just Culture Committee Critical Care Joint Invasive Procedures Preoccupation with Failure Reluctance to Simplify Nightingale Heroes Data Review Committee Sentinel Events Committee Quality 20/22 P&T Shared Governance Just Culture Philosophy Communication Tools CEO Council TBD Intranet R.A.D.A.R Resilience 3/22/2025
High Reliability Organization High Reliability Organizations (HRO) are those organizations that are high-risk, dynamic, turbulent, and potentially hazardous, yet operate nearly error-free. Patient variability & diverse human factors make healthcare delivery even more complex and often unpredictable. Steps to achieve Zero Harm (The Joint Commission): Ensure leadership is committed to zero harm Ensure a culture of safety Incorporate process improvement methodologies into daily work Demonstrate how everyone is committed to quality & safety
Five Characteristics of a High Reliability Organization
CMS / TJC / Others QUALITY REPORTING REQUIREMENTS
Hospital Promoting Interoperability Created by CMS in 2011 for the mandated adoption of functions and standards for electronic health record technology. Program requirements change annually. Measures Report Antimicrobial Use and Resistance (AUR) data to NHSN E-Prescribing Query of Prescription Drug Monitoring Program (PDMP) Support Electronic Referral Loops by Sending Health Information Support Electronic Referral Loops by Receiving and Reconciling Health Information (or Health Information Exchange Bi-Directional) or (Enabling Exchange under TEFCA) Provide Patients Electronic Access to their Health Information Report on the following Syndromic Surveillance Reporting Immunization Registry Reporting Electronic Case Reporting Electronic Reportable Lab Result Reporting Bonus Public Health Registry Reporting Clinical Data Registry Reporting
Electronic Clinical Quality Measures (eCQMs) Measures specified in a standard electronic format that use data electronically extracted from electronic health records Were initially part of hospital promoting interoperability program but were moved to the hospital inpatient quality reporting program Both CMS and TJC require eCQM reporting
CMS / TJC Inpatient Quality Measures Influenza Vaccination Among Healthcare Personnel Hospital Commitment to Health Equity COVID-19 Vaccination Among Healthcare Personnel Safe Use of Opioids Concurrent Prescribing (eCQM) Death Rate among Surgical Inpatients with Serious Treatable Conditions Severe Obstetric Complications (eCQM) Hospital 30-day, All-Cause, Risk Standardized Mortality Rate following Acute Ischemic Stroke Three additional self selected eCQMs Risk-Standardized Complication Rate Following Primary Elective THA and/or TKA Cesarean Birth (eCQM) Hospital Wide- All-Cause Unplanned Readmission Hybrid Hospital-Wade All-Cause Risk Standardized Mortality Excess Days in Acute Care following AMI; HF; PN Hybrid Hospital Wide All-Cause Readmission Hospital Risk-Standardized Payment Associated with a 30-Day Episode of Care for AMI; HF; PN; THA/TKA HCAHPS Survey Medicare Spending Per Beneficiary Screening for Social Drivers of Health Early Elective Delivery Screen Positive Rate for Social Drivers of Health Maternal Morbidity Structural Measure Severe Sepsis / Septic Shock Management 50
CMS Outpatient Quality Measures Admissions & ED visits for Patients Receiving OP Chemo Cardiac Imaging for Preoperative Risk Assessment for Non-Cardiac Low-Risk Surgery 7-Day Risk Standardized Hospital Visit Rate after OP Colonoscopy Breast Cancer Screening Recall Rate MRI Lumbar Spine for Low Back Pain Hospital Visits after Hospital Outpatient Surgery Abdomen CT Use of Contrast
Additional data submission to various organizations Georgia Registry of Immunization Transactions and Services (GRITS) American Heart Association (AHA) Blue Cross/ Blue Shield Quality In-Sights Hospital Incentive Program (Q-HIP) Get With The Guidelines (GWTG) Stroke and Coverdell Registry American College of Cardiology (ACC)- Percutaneous Cardiovascular Intervention (PCI) and Implantable Cardioverter Defibrillator (ICD) Society of Thoracic Surgeons (STS) Vascular Registry ECMO Registry National Healthcare Safety Network (NHSN) TAVER Registry
CMS / QHIP VALUE BASED PAYMENT
What are Value Based Payment Programs These are programs put in place by CMS and other commercial payors to reward and / or penalize good and / or less than optimal care of patients. Pay for performance programs have morphed each year since inception. The most recent focus is on outcomes, patient satisfaction, safety, and efficiency and cost reduction.
HAC Hospital Acquired Conditions Penalty Program 1% penalty for worst-performing 25% of hospitals Payment adjustment applies to all Medicare fee-for-service discharges for the applicable fiscal program year Total HAC Score is the equally weighted average of scores on the measures included in the program Five chart-abstracted measures of HAIs submitted to NHSN CLABSI CaUTI SSI for abdominal hysterectomy & colon procedures MRSA Bacteremia CDI One claims-based composite measure of patient safety (PSI-90) v.10.0 Typically based on two years of data Adjustments were made for COVID Excluding CY 2020 and 2021 claims data from HAC Program calculations Updated PSI-90 measure to include a risk adjustment parameter for COVID POA
VBP Value Based Purchasing 4 Domains equally weighted at 25% each are used to calculate total score Clinical Outcomes Domain 30-Day Mortality Measures (AMI, CABG, COPD, HF, PN) THA/TKA Complication Rate Person & Community Engagement HCAHPS Safety Domain CaUTI CDI CLABSI MRSA Bacteremia SSI Abdominal Hysterectomy / Colon Efficiency & Cost Reduction Medicare Spend per Beneficiary
VBP Value Based Purchasing Bonus / Penalty program 2% taken off the top hospital has capacity to lose all 2% or earn back a portion up to greater than 2% based on performance Hospital receives two scores on each measure and dimension Achievement score is determined by comparing performance to score between Threshold which is 50thpercentile and Benchmark which is top 10% Improvement score is determined by comparing performance to the hospitals own performance in a previous timeframe (2 5 years prior based on measure) HCAHPS also factors in consistency score and floor CMS uses the greater of either to calculate overall total performance Payment adjustment applied to all Medicare Fee for Service discharges in applicable payment year Program requirements set through FY 2029 Data timeframes vary by measure. Modifications made to data timeframes to adjust for COVID.
HRRP Hospital Readmission Reduction Program Penalty program up to 3% based on 30-day all cause readmission for specific diagnosis AMI Pneumonia THA/TKA Payment adjustment applies to all Medicare fee-for-service discharges for the applicable fiscal program year Payment reduction Calculation Excess Readmission Ratio (ERR) Hospitals stratified into peer groups based on number of dual eligible patients Calculates ERR for each peer group Compares hospital performance to peer group median ERR Calculates payment adjustment factor Adjustments made to patients included for COVID. - HF - COPD - CABG
What Physicians Can Do to Help. . . . . 1. Be aware of measures under scrutiny 2. Use order sets as frequently as possible that have been vetted as best practice and include quality measures. 3. Be open to suggestions from St. Joseph s/Candler colleagues about drug choices, clarification of diagnosis, etc 4. Do all medical records in a timely fashion. 5. Know PSI data in HAC program comes from physician documentation. 6. Answer coding / CDI queries promptly. 7. Support nursing protocols to discontinue foley catheters. 8. Discontinue central lines as soon as possible.
What Physicians Can Do to Help. . . . . 9. Consider alternative causes of diarrhea (laxatives, contrast, or PPIs) prior to ordering c-diff testing. 10. Remember HCAHPS Communication with Physicians counts toward VBP scores. 11.Patient enrollment in hospice within the year prior to admission or on the day of admission excludes the patient from mortality calculations. 12.Start palliative care / hospice discussions with patients / families when appropriate. Utilize the palliative care team when appropriate.
QUESTIONS? Put me in your cell phone: Mindy McStott, LMSW, BSN, RN Director, System Quality Performance Office: 912-819-6676 Cell: 229-339-1247 Email Address: mcstottm@sjchs.org