Guide to Initiating Buprenorphine in the Emergency Department
Learn how to initiate buprenorphine and refer patients to treatment in the emergency department to combat the opioid epidemic. Understand the benefits, protocols, and considerations for using buprenorphine effectively and safely.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
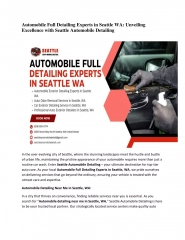
ED Initiated Buprenorphine & Referral to Treatment A brief guide for ED Practitioners Comments or questions? Kathryn Hawk, MD, MHS Kathryn.hawk@yale.edu Ryan McCormack, MD, MS Ryan.mccormack@nyulangone.org Study email: ED-Connect@nyulangone.org Why the ED? Because that s where the patients are! Responding to the Opioid Epidemic Opioid-related ED visits are escalating. We are on the front lines with little preparation or tools to combat this crisis. Opioid-related ED visits more than doubled in 10 years. ED visits for overdose (OD) increased 30% from July 2016 Sept 2017. ED visits and surviving an OD are strong predictors of subsequent OD death. 90% of patients with substance use disorder go untreated. ED is the only access point for healthcare for many. We encounter patients at critical moments in their lives. What can you do? Prescribe opioids safely and judiciously Increase access to medication treatments Initiate buprenorphine Provide Warm scheduled referrals Offer harm reduction strategies Overdose education and training Naloxone Prescription Community resources (e.g. peers) What is the evidence? Buprenorphine (BUP) for Opioid Use Disorder (OUD) has been well-studied and clinically used for decades. Strong evidence of BUPs effectiveness: OD, Death, drug use, HIV/HCV, Crime Treatment engagement, Social functioning quality Build trust and engage the patient Treat with empathy and respect We have medicine that works! D Onofrio et al. (JAMA 2015) showed BUP in the ED is feasible and safe with strong 30-day treatment effect: Twice as likely to be in treatment Less illicit drug use reported What do I need to know about buprenorphine? It is NOT simply replacing one drug for another How does it work? BUP reduces craving and withdrawal. Do not give BUP until the patient is in opioid withdrawal. o BUP is a partial agonist at the mu-opioid receptor with higher affinity than full agonists. Thus, if given to too early, BUP will cause withdrawal by displacing full agonist. It is safer than full agonists because of its ceiling effect . o Once at a therapeutic level, higher doses don t cause more mu-receptor activation or CNS depression. Patients can safely be prescribed BUP for unobserved home induction (if not yet in withdrawal in the ED). (methadone, heroin)
Screen: Identify Non-Medical Opioid Use ED-Initiated Buprenorphine Clinical Protocol Flow Diagram Using EMR template for guidance and documentation is recommended. Assess ED-BUP eligibility OUD with current, regular use Willing to start BUP today (in ED or by prescription)? Consider complicating factors (Methadone/Long- acting opioids, co-occurring sedative use, etc.) No Do not administer BUP in ED Consider consultation or inpatient for complex cases Harm reduction See All Patients below Assess for withdrawal Clinical Opiate Withdrawal Scale (COWS) No objective withdrawal (COWS <8) Objective signs of withdrawal (COWS 8) Do not administer BUP in ED Administer BUP(Dose 1) Consider additional dose(Dose 2) Reassess symptoms after >30 min Waiveredprovider able to prescribe BUP? Labs: UTox (confirm opioid use & exclude methadone) and hcG. Consider LFTs, HIV, & HCV. No Yes Warm Referral for treatment Ancillary withdrawal management if referral >24hrs Legally, patients may be treated with BUP in ED 3 days in a row. Our ED providers should avoid having patients return to the ED for repeat dosing. Prescribe BUP bridge to appointment or for home induction(Rx) Provide Education, instructions,& referral for treatment. Consider Naloxone kit. Update contact information. Consider HIPAA form for follow-up. Notify Research staff & patient contact for quality improvement & paid study. All Patients: Footnotes: Dose 1: Typically start with 4mg. BUP can cause precipitated withdrawal if given too soon. Start low dose (2-4mg) if borderline symptoms or any uncertainty. If COWS >12 give 8mg. Generally, time to withdrawal is 12 hours for short-acting opioids. Dose 2: Day 1 Total 8-16mg SL BUP/Nx. Higher doses may be considered by experts for longer withdrawal/craving suppression. RX: Typical bridge dosing: BUP/Nx 16mg SL daily x # days until appointment. See unobserved home induction orders: BUP/Nx: 4mg SL up to 4x on day 1, then 16mg SL qDay x # days until follow up appointment. :Worsening symptoms after BUP may be precipitated withdrawal. No further BUP should be given. Provide supportive medications (e.g. clonidine, anti-emetics, NSAIDS) Consult expert if severe. Ancillary medication treatments with BUP induction are not needed unless unable to bridge BUP to next appointment.
Step by Step Pocket Guide to ED-initiated BUP Step? 1:? Identify? patients? with? possible? OUD? How? many? times? in? the? last? year? have? you? used? heroin,? fentanyl,? or? prescription? opioid? medications? for? nonmedical? reasons? ? ? ? Any? response? >never? is? a? positive? screen? and? warrants? further? assessment.? ? Step? 2:? ? Assess? eligibility? for? ED-initiated? buprenorphine? (BUP)? by? meeting? the? following? criteria.? Recent,? regular? opioid? use? (i.e.,? daily/almost? daily? use,? including? within? the? last? 7? days)? Meets? DSM-5? criteria? for? moderate? to? severe? OUD? (4? or? more? criteria)? Needs? treatment? (i.e.,? not? already? in? formal? medication? treatment? program)? ? Step? 3:? Assess? willingness? to? receive? ED-initiated? BUP? (in? ED? or? by? prescription)? Would? you? like? to? receive? buprenorphine? (suboxone)? in? the? ED? today. ? Provide? information? and? decision? support? as? needed? so? that? the? patient? may? weigh? treatment? options.? ? Engage? the? patient? to? enhance? motivation? for? treatment.? ? Be? cognizant? of? negative? language? and? stigma.? ? ? Step? 4:? Consider? complicating? factors? and? potential? contraindications? Recent? Methadone? or? long-acting? opioid? use? Unstable? alcohol,? benzodiazepine,? or? other? sedative? use? ? Medical,? psychiatric,? or? surgical? instability? or? decompensated? liver/lung/heart/kidney? disease? Prisoner? (Ok? to? treat,? but? may? be? unable? to? fill? prescription? or? continue? medication)? Pregnancy? (NOT? a? contraindication!? BUP? formulations? without? naloxone? preferred)? ? Step? 4:? ? Assess? for? objective? signs? of? opioid? withdrawal? Patient? MUST? have? objective? signs? of? withdrawal? before? starting? BUP!? (Minimum? COW 8)? Risk? of? precipitated? withdrawal? if? BUP? given? too? early? or? in? patient? taking? methadone? ? Step? 5:? Laboratory? testing? is? not? required? UTOX? and? hcG? often? required? for? referral.? UTOX? to? confirm? opioid? use? and? exclude? methadone? use.? Consider? LFTs,? HIV? and? HCV? testing? as? these? are? recommended? early? in? treatment.? ? ? ? Step? 6:? Offer? to? initiate? BUP? in? appropriate? patients? ? For? patients? in? withdrawal? (COWS? ? 8):? Typical? initial? dose? is? BUP? SL? 4-8mg.? Reassess? >30? minutes? later? before? giving? second? dose.? Less? experienced? providers? should? start? low? (dose)? and? go? slow.? Patients? with? severe? withdrawal? should? receive? an? initial? dose? of? 8mg.? Total? day? 1? dose? is? typically? 8-16mg.? ? For? patients? not? in? withdrawal:? ? DEA? X-waivered? providers? may? prescribe? BUP? for? unobserved? home ? induction.? ? Step? 7:? Reassess? symptoms? 30-60? minutes? after? BUP? administration? ? Step? 8:? Provide? prescription? of? BUP/naloxone? when? appropriate? (DEA? X-waivered? providers? only)? Bridge? Prescription:? ? Buprenorphine/naloxone? 8mg/2mg? (tabs? or? film):? ? Two? tabs/strips? sublingual? once? daily.? ? Disp:? quantity? sufficient? to? appointment? (goal? 2-7? days).? o? BUP? without? naloxone? (Subutex)? is? not? recommended,? except? in? pregnancy.? (Abuse? potential)? Unobserved? Induction? Prescription:? Patients? who? are? not? yet? in? opioid? withdrawal? may? be? given? a? prescription? for? unobserved? home ? induction? along? with? the? instructions.? ? BUP/NX:? 4mg? tab/film? up? to? 4? times? on? day? 1,? then? 16mg? SL? once? daily.? ? Step? 9:? ? Facilitate? referral? for? ongoing? medication? treatment? ? Facilitate? a? warm? referral? --? i.e.? a? scheduled? appointment? with? an? X-waivered? BUP? prescriber.? ? If? BUP? not? prescribed,? needs? appointment? before? withdrawal? (24? hours)? ? Patients? may? be? administered? BUP? in? the? ED? for? no? more? than? 72hours? in? a? row.? Avoid? ED? revisit? if? possible.? Consider? social? work,? peer? support? referral,? and/or? other? services? to? aid? with? navigation? and? support.? ? Step? 10:? ? Provide? patient? with? education? and? resources? Provide? materials? about? OUD? and? BUP,? medication? instructions/precautions,? other? resources? &? referral? ? Consider? prescribing? a? naloxone? kit? and? providing? other? harm? reduction? advice.? ? Step? 11:? Facilitate? future? contact? and? quality? improvement? and? potential? research? Update? contact? information? ? obtain? HIPAA? authorization? for? potential? future? contact.? ? How do I obtain an X-waiver to prescribe BUP? DATA waiver training for providers https://www.samhsa.gov/medication-assisted-treatment/training-resources/buprenorphine-physician-training https://pcssnow.org/education-training/ ACEP 2018 Scientific Assembly September 29, 2018 (https://bit.ly/2P2Juhn)
How to assess for withdrawal? How to assess for OUD? Questions based on DSM-5 criteria: 1. Have you found that when you started using, you ended up taking more than you intended to? 2. Have you wanted to stop or cut down on using opioids? 3. Have you spent a lot of time getting or using opioids? 4. Have you had a strong desire or urge to use opioids 5. Have you missed work or school or often arrived late because you were intoxicated, high or recovering from the night before? 6. Has your use of opioids caused problems with other people such as with family members, friends or people at work? 7. Have you had to give up or spend less time working, enjoying hobbies, or being with others because of your drug use? 8. Have you ever gotten high before doing something that requires coordination or concentration like driving, boating, climbing a ladder, or operating heavy machinery? 9. Have you continued to use even though you knew that the drug caused you problems like making you depressed, anxious, agitated or irritable? 10.Have you found you needed to use much more drug to get the same effect that you did when you first started taking it? 11.When you reduced or stopped using, did you have withdrawal symptoms or felt sick when you cut down or stopped using? L O S S O F C O N T R O L Clinical Opioid Withdrawal Scale (COWS) Moderate OUD: 4-5 symptoms Severe OUD: 6 or more symptoms Most providers fear talking to patients about substance use. This guide may help: Step 1. Raise the Subject/Establish Rapport Introduce yourself Raise the subject of opioid use and ask permission to discuss OUD Assess patients subjective level of physical discomfort (i.e., withdrawal) Step 2. Provide Feedback Review patients drug use and patterns Ask the patient about and discuss drug use and its negative consequences Make a connection (if possible) between drug use and visit or medical issues Provide feedback on OUD diagnosis and treatment options (e.g., medication (BUP, methadone, naltrexone), behavioral outpatient programs, 12-step, and/or harm reduction strategies. Step 3. Enhance Motivation Assess readiness to change with regard to starting preferred treatment On a scale of 1-10, how ready are you to start BUP right now? Enhance Motivation Ask a series of open-ended questions designed to evoke Change Talk (or motivational statements) about their target behavior. Reflect or reiterate the patient s motivational statements regarding entering treatment. Step 4. Negotiate & Advise Negotiate goal regarding the target behavior (e.g. starting BUP) Give advice Complete a referral/treatment or goal agreement, and secure and provide the actual referral for treatment (BUP or other) Video example: https://www.aetna.com/health-care- professionals/patient-care-programs/impact-of-opioid-use-disorder.html Only start BUP if COWS 8.