Guidelines on Tobacco Use in Mental Health: Overcoming Obstacles
Anticipate the impact of tobacco use on antipsychotic drug metabolism, alter doses accordingly. Focus on addressing obstacles to smoking cessation in general hospitals, with a spotlight on severe mental illness. Explore the drivers of premature mortality in individuals with mental disorders, including smoking, alcohol misuse, poverty, obesity, and prescribed medications. Learn how to offer effective interventions for smoking cessation in clinical settings.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
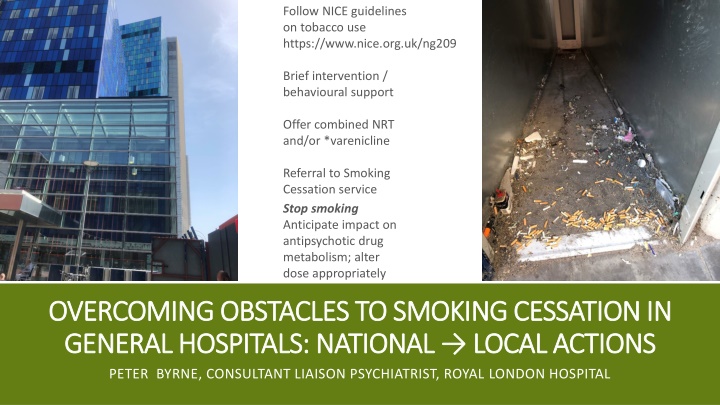
Follow NICE guidelines on tobacco use https://www.nice.org.uk/ng209 Brief intervention / behavioural support Offer combined NRT and/or *varenicline Referral to Smoking Cessation service Stop smoking Anticipate impact on antipsychotic drug metabolism; alter dose appropriately OVERCOMING OBSTACLES TO SMOKING CESSATION IN OVERCOMING OBSTACLES TO SMOKING CESSATION IN GENERAL HOSPITALS: NATIONAL LOCAL ACTIONS GENERAL HOSPITALS: NATIONAL LOCAL ACTIONS PETER BYRNE, CONSULTANT LIAISON PSYCHIATRIST, ROYAL LONDON HOSPITAL
FOCUS OF THIS TALK: WHERE / HOW WE WORK, AIMED AT CLINICIANS (POSITIONS OF INFLUENCE) Nationally, falling smoking rates (<15%) except in people with mental health (MH) conditions evidence of return to smoking / increased rates in severe mental illness (SMI) rates during pandemic, pandemic s secondary effects on health / care services and ongoing cost of living crisis. Start with data & known comorbidities harm. General hospitals: even before Covid but increasing since the end of lockdowns people with SMI / PD / dementia / ID / Addictions etc. are admitted more often to general hospitals than psych hospitals. (Shorter duration stay with unfamiliar teams) Treatment gap in MH conditions (other than psychosis, only a minority get any treatment) has a parallel with policy-practice gap in general hospitals The not-with-MH-services people with mental disorders: there is no funding for GPs to prescribe Nicotine Replacement Therapy; will IAPT ask about smoking? The short lengths and reactive natures of admission put excess pressures on GP, community
Seven drivers of Premature Mortality in people with severe mental illness. (SMI) Smoking Direct cause of cardiovascular diseases & chronic obstructive lung disease (COPD) #1 preventable cause of cancer Risk taking behaviours Byrne, 2023: Irish Journal Psychological Medicine Alcohol excess / dependence Excess = weekly consumption above 14 units associations with accidents, hypertension etc major preventable cause of cancer Poverty-Inequality Chronic stressors: food/fuel poverty, housing insecurity Specific: Adverse Childhood Experiences, bullying Prescribed / Illegal Opioids Strong links to poverty taken for chronic pain despite lack of efficacy; most deaths are due to respiratory arrest Inequalities worsen health effects Obesity-Diabetes = unhealthy diet + low levels exercise Inequalities drive childhood overweight Hidden effects e.g. diabetes in the liver Obesogenic prescribing Antipsychotics (APs), antidepressants, mood stabilisers; polypharmacy; excess or inappropriate use: e.g. APs in intellectual disability, personality disorder & dementia in the absence of psychotic symptoms Accidents, violence (to / by) sexually transmitted infections e.g US hepatitis rates are 1% in the general population; 20% in SMI (x) Substance misuse (nicotine and cannabis as gateway drugs) Organ damage higher if liver impairment Interactions with prescribed medication e.g.
UK Gov data as Fingertips SMI and Public Health Outcomes Framework 3 years to 2010: adults with SMI were 2.5 to 7.2 2.5 to 7.2 times more likely to die before aged 75 two thirds from preventable physical diseases
UK Gov / fingertips, PHOF map of upper tier local map of upper tier local authorities (April 2020 to authorities (April 2020 to March 2021) in England for March 2021) in England for premature mortality in adults premature mortality in adults with severe mental illness. with severe mental illness. Directly standardised rate Directly standardised rate - - per 100,000, 2018 to 2020 per 100,000, 2018 to 2020
ARE PEOPLE WITH MENTAL DISORDERS (1 IN 4 OF US) A DIFFERENT SPECIES? NO, SOME SOLUTIONS DIFFER It only took seven decades to reduce smoking rates - taxes on products, bans on advertising, fall in tobacco production (incl State subsidy) & more - achievements by public health, ASH More addicted to nicotine, more vulnerable to complications of smoking (especially if alcohol excess) and further negatives ( Meds doses; tobacco poverty; social isolation) but ppl with MH probs want to quit just as much as other smokers People with severe mental illness (SMI) have smoking rates of 40%; Addictions, PD, ID even higher Evidence-based treatments +++ and quits even in lock up psychiatry wards do NOT increase violence/aggression Alongside more MH awareness, better coping strategies other than cigs. Growing awareness that smoking adds to mental disorder symptom burden (smoking is not a relief against these) General hospitals speak of patient journey true, but it s less a country stroll and more of a roller coaster
OBSTACLES TO SCREEN + INTERVENE Community MH teams Psych wards Gen Hospital Fragmentation of heath services, education (medicine V psychiatry), with public health / addictions separated from mainstream services Risk to self and others #1, other priorities trump Time pressures, delegate to GP, acute care, other Enforced cessation when in plain sight Just like smoking cessation in clinical contexts is everybody s job , does the same thing happen (NOTHING) within national governments, health structures, arms length bodies, local authorities, now ICS Boards? we have to focus on the things we have to fix now we have enough to do without being her GP as well as long as he s here for the ward round, let him smoke NRT NRT We have all the evidence we need but (1) training gap and (2) institutional barriers to implement what works Wide variation between teams Varenicline X E cigs X Varenicline ? E cigs
LEADERSHIP AT ALL LEVELS, AND NOT STOP-START At individual level, the patient-clinician relationship: to help people to live the lives they have reason to value . Is smoking a choice? Really? Return the focus to health We are NOT forcing patients or staff into Nicotine withdrawal: generous NRT (2 sources), E Cigs and anti-nicotine craving medications; pair break from ward with NRT How organisations communicate SmokeFree Policies and enforce them: NO SMOKING means no smoking; close the smoking shelters, meeting points, end fresh air breaks The inequalities of Smoking and the inequalities of access / preventable smoking deaths are important. Resource staff with time: training & practice, supervision At the very top, we have Dr Bola Owalabi sCORE 20 plus 5 (tobacco crosses all five) and the NHS Tobacco Dependence Stakeholder Group (Chair, Dr Sanjay Agrawal) NCCMH / RCPsych s QUITT programme pilot sites (comm MH and acute Trusts)
Driving change / key areas Electronic and supervision reminders for clinicians, all patient- facing staff Keeping tobacco on every agenda across fragmented health / care services Comorbidities: resp and MH and cardiac and more. NO MORE either / or thinking Snapshots of rates of smoking and training: hospital Comms; end harms too The challenges of directive-fatigue, competing priorities Policy Practice Very brief advice, Vaping and Varenicline When to activate enforcement (no smoking rules)
THEORY OF CHANGE IN ONE SLIDE Coproduce, co-create Evaluate openly Experiment, QI Explore Educate + Sustain Establish norms Hug Smack Nudge Shove