Guillain-Barré Syndrome: An Overview
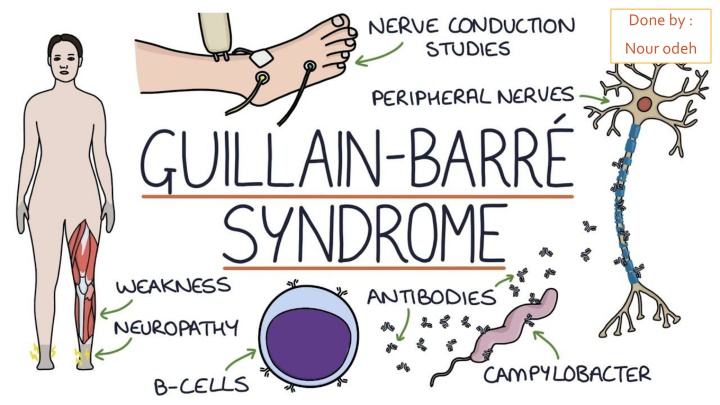
Guillain-Barré syndrome (GBS) is an acute postinfectious polyneuropathy characterized by autoimmune reaction, nerve conduction loss, ascending limb weakness, cranial nerve involvement, and potential respiratory muscle weakness. Etiology involves prior infections or vaccinations, while pathophysiology includes autoimmune-mediated demyelination. Clinical features range from minor sensory symptoms to flaccid paralysis, with potential life-threatening complications. Examination reveals limb paralysis, sensory deficits, and autonomic instability.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Done by : Nour odeh
Guillain-Barr syndrome (GBS) is an acute postinfectious polyneuropathy . Acute inflammatory and demyelinating polyneuropathy with variable axonal damage . Demyelinating of the PNS .
Etiology Overview About of GBS patients experience symptoms of an upper respiratory or gastrointestinal tract infection 1 4 weeks prior to onset of GBS.[1] The causal connection between pathogens and GBS is still undetermined. Associated pathogens[1][3][4] Campylobacter jejuni: campylobacter enteritis is the most common disease associated with GBS. Cytomegalovirus: most common virus associated with GBS HIV Influenza Epstein-Barr virus Mycoplasma pneumoniae Vaccination There have been reports of small increases in incidence after administration of certain vaccines.[5] In the US, Guillain-Barr syndrome is listed as vaccination injury for the seasonal influenza vaccines. (swine).
Pathophysiology Postinfectious autoimmune reaction that generates cross-reactive antibodies (molecular mimicry) Infection triggers humoral response formation of autoantibodies against gangliosides or other unknown antigens of peripheral Schwann cells immune-mediated segmental demyelination axonal degeneration of motor and sensory fibers in peripheral and cranial nerves .
Clinical feature Due to progressive loss of nerve conduction . Spinal pain minor sensory symptoms (paraesthesiae in the extremities) may precede progressive, ascending, symmetrical limb weakness. motor :Paralysis of the legs then arms ( Ascending paralysis) cranial nerve involvement : drooling, dysphagia (and nasal regurgitation) and slurred speech. Later still, respiratory muscle weakness, with dyspnoea and fatigue, may develop. The course of the illness may be very rapid, with maximum deficit being reached in hours or days by definition in less than a month. Progression may arrest at any stage, some patients having a relatively mild illness and remaining ambulant, others spending weeks ventilated in an intensive care unit. Individual slowly recover over several month ( until remyelination) . GBS paralysis affects the muscles of respiration, possibly leading to death due to respiratory failure.
On examination there is flaccid paralysis of the limbs early tendon areflexia minor sensory deficits. Cranial nerve palsies particularly include the facial nerve and bulbar dysfunction. Autonomic instability in severe Guillain Barre syndrome 1. labile blood pressure and cardiac dysrhythmias 2. sphincteric symptoms, e.g. urinary hesitancy and retentio
Overview of subtypes and variants of Guillain-Barr syndrome Description Etiology Clinical features Acute variant of Guillain-Barr syndrome Predominantsub- typeaffecting60 80%ofGBSpatients in North America and Europe Associated withCampylobacter andCMV Autoantibodiesagainst various antigens Ascending paralysis Autonomic neuropathy CN defects andpain Peak at 4 weeks Acute inflammatory demyelinating polyneuropathy(AIDP)[7] CIDPhas not been linked to anypathogenin particular. Anti-GM1 ganglioside autoantibodies Chronic inflammatory demyelinating polyneuropathy(CIDP)[8][9] Chronic variant of Guillain-Barr syndrome Similar to those ofGBS, but lasting> 2 months A limited variant ofGBS characterized by cranial nerve involvement Ophthalmoplegia Ataxia Areflexia Autoantibodiesdirected againstganglioside Miller-Fisher syndrome Multifocal motor conduction block Anti-GM1 ganglioside autoantibodies Usually normal protein levels inCSF[11] A variant ofGBSsolely affecting the motor neurons. Differential diagnosis for amyotrophic lateral sclerosis Asymmetric paralysis andareflexia Initially involves thedistalupper limbs Multifocal motor neuropathy(MMN)[10] Typically occurs after an infection withCampylobacter jejuniand may be associated withantibodiesdirected towardGM1ganglioside- likeepitopes. Anabrupt-onsetvariant ofGBS Affects motor nerve fibers with variable severity and spares sensory fibers Acute paralysis Areflexia without sensory loss Acute motor axonal neuropathy(AMAN)
Diagnostics Lumber puncture Cerebrospinal fluid: albuminocytologic dissociation Protein levels and normal white blood cell count in cerebrospinal fluid (CSF) though findings may be normal early in the disease Serological screening To identify potential pathogens (e.g., Campylobacter jejuni) Detection of antibodies directed against gangliosides (Up to one-quarter of patients ) Because these investigations are often negative, other tests may be necessary to eliminate disorders that enter the differential diagnosis Electroneurography Nerve conduction velocity (NCV) due to demyelination but may show only mild or no abnormality at early stages. Electromyography Signs of denervation: characteristic of axonal lesions Pathologic spontaneous activity (unfavorable prognostic sign) but may show only mild or no abnormality at early stages. ECG: autonomic cardiac dysregulation impaired heart frequency variation
Treatment Supportive management (to reduce symptoms) in the progressive phase :Monitor cardiac and respiratory function: ECG , in some cases, intensive care unit (ICU) treatment and intubation may be indicated Limb weakness requires regular physiotherapy, to prevent joint stiffness and contractures, and turning, to protect against pressure sores. Low molecular weight heparin should be administered as prophylaxis against deep vein thrombosis and pulmonary embolism. Mouth and eye care, and aspiration of secretions. Intravenous immunoglobulins (immunosuppressive ) 1-plasma exchange . 2- high-dose intravenous immunoglobulins (usually five daily infusions). These treatments have been shown to speed the rate of recovery and hence reduce the risk of complications. Although GBS is considered an autoimmune disease, glucocorticoids are not recommended for treatment. They have not shown to fasten recovery or affect the long-term outcome.
Prognosis Guillain Barre syndrome is usually a mono- phasic illness, 80% of patients with GBS have a good prognosis[13] Disease progression peaks 2 4 weeks after the onset of symptoms. Symptoms then recede in reverse order of their development (i.e., the last symptoms to appear resolve first, as Schwann cells remyelinate peripheral nerve axons). 5-10% of patients with GBS die due to acute complications such as: Respiratory paralysis (apnea) Pulmonary infection/embolism Cardiac dysfunction MORE THAN 10 % of affected individuals are still unable to walk unaided. permanent disability and a few relapse .
Indicators of poor prognosis include: increasing patient age. rapid onset of weakness. need for ventilation. antiganglioside antibodies. preceding diarrhoeal illness . electrophysiological parameters showing significant axonal degeneration.
Reference : https://next.amboss.com/us/article/7R04of?q=guillainbarr%C3%A9%20syndrome#Zf193c1b0b16db4d30e7f29d4e766 d3e8 https://www.osmosis.org/learn/Guillain-Barre_syndrome lecture note neurology .

![❤[PDF]⚡ Zee Zee Does It Anyway!: A Story about down Syndrome and Determination](/thumb/20462/pdf-zee-zee-does-it-anyway-a-story-about-down-syndrome-and-determination.jpg)