Gynaecological Referrals from Primary to Secondary Care: Dr. Fozia Malik
This content covers gynaecological referrals to secondary care, including chronic pelvic pain, polycystic ovary syndrome, and non-neoplastic disorders. It provides information on the definition, contributory factors, and management of chronic pelvic pain, as well as the diagnosis and risks associated with polycystic ovarian syndrome.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Gynaecological referrals from primary to secondary care Dr Fozia Malik MRCOG,DFSRH 14/11/2018
Referral to Gynaecology Out Patient chronic pelvic pain Polycystic Ovary Syndrome Non-neoplastic epithelial disorders of the vulva Contraception Vaginal discharge
chronic pelvic pain CPP is defined as intermittent or continuous pain of at least six months' duration felt in the lower abdomen or pelvis, NOT associated exclusively with menstruation, intercourse, pregnancy or malignancy
Management of chronic pelvic pain A careful history is required including assessment for red flag symptoms. Examination should involve assessment for abdominal scars or localised spots of pain. Focal tenderness or pelvic floor trigger points may be detected on vaginal examination. Investigations include swabs to screen for sexually transmitted infections, urinalysis and USS pelvis. Therapeutic options include simple analgesics or adjuvant analgesics such as amitriptyline or gabapentin. Hormonal treatment for ovarian suppression should be trialed before offering diagnostic laparoscopy
siPolycystic Ovarian Syndrome Ovary Syndrome PCOS should be diagnosed according to the Rotterdam consensus criteria polycystic ovaries oligo-ovulation or anovulation clinical and/or biochemical signs of hyperandrogenism
Risk associated with PCOS Metabolic consequences of PCOS Risk of developing gestational diabetes Risk for type II diabetes Risk of developing sleep apnoea Risk of developing cardiovascular disease Risk of having reduced health-related quality of life Risks of cancer in women with PCOS
Strategies for reduction of risks Exercise and weight control It is recommended that lifestyle changes, including diet, exercise and weight loss, are initiated as the first line of treatment Insulin-sensitising agents have not been licensed in the UK for use in patients without diabetes.
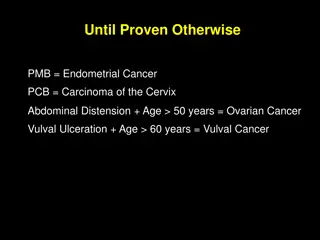
Non-neoplastic epithelial disorders of the vulva
Non-neoplastic epithelial disorders of the vulva Vulval pruritus has a wide, differential diagnosis. Lichen sclerosus (LS) is common and most patients respond to topical ultrapotent corticosteroids. LS not responsive to treatment might be due to hyperkeratotic disease, poor treatment compliance, contact sensitivity to steroids, or infection. For difficult cases, the opinion of a vulval dermatologist is invaluable Some patients with lichen sclerosus will need referral to a vulval service when they do not respond to topical steroids (or develop symptoms whilst on treatment). In these patients consider:
contraception Most methods of contraception are safe for most women. For women with certain medical conditions, the UK Medical Eligibility Criteria provides guidance on the relative safety of each method. Long-acting reversible contraception methods are associated with lower failure rates as they are less user-dependent than other methods. Women requesting contraception should receive comprehensive and clear verbal and written information on all methods that are safe for them, in order to make an informed choice
Vaginal discharge Careful history taking to identify symptoms, which will guide examination and tests required Identify sites needing sampled depending on sexual practices Confirm timing of sexual exposure to assess reliability of tests and possibility of window periods Allow discussion of other sexual health issues (e.g. psychosexual problems) Be mindful that this consultation may be embarrassing or uncomfortable for the patient A non-judgemental attitude is key