Health: Concepts and Practices
Explore the meaning of health beyond just the absence of disease, emphasizing physical and mental well-being. Learn about health promotion, observational mindset, and the role of support workers in healthcare. Understand the significance of health status indicators and descriptive language in healthcare settings.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
895.44 NDCPD July 2012 1
A. What is Health? More than absence of disease Positive concept Physical health good body health as result of what? Mental health emotional and psychological well-being. What does this mean to you? Health changes over time. How? 2
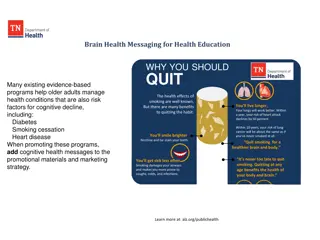
B. Health Promotion Nutrition Strong Social relationships Exercise Hygiene & Infection Control Stress Management Health Care Public Health Policies & Practices 3
C. Observational Mind-set How do people who can t talk tell you that something is wrong? It s very important that we develop a keen observation sense. Know what the person is like by using: visual sense auditory smell touch 4
DSPs become the eyes, ears, & nose for the supervisor, nurse, or doctor. Take a look at questions on page 9 5
D. Health Status Indicators Usually give more info to doctor/nurse than just a written report Health Related Habits like smoking, drinking, lack of exercise Sleep any changes in pattern or time Eating and Weight changes that may occur over time 6
E. Descriptive Language Leaves little room for interpretation Goes back to the English classroom Which is descriptive? Al was aggressive today. Al hit the wall with his right fist. How can we make this descriptive ? Henry isn t feeling well today. 7
You may need to assist with a wide range of supports with health appointments. Be sure to support the individual to do as much for them selves as possible and to take an active role Be sure to help them prepare for the appointment. After the appointment, rely the information to all those concerned and help ensure the Doctor s recommendations are followed. active role in the appointment. 8
The main forms of intervention are: Physical Therapy Occupational Therapy Speech Therapy As a DSP, you may have many roles when supporting people who need Adaptive Equipment or therapy sessions. 9
Illness is the opposite of health How? Illness affects the body as well as the mind How can an ulcer for example, affect the mind? 10
Respiratory & Circulatory Heart, lung, nose Transfer food & oxygen to cells, removes toxins Gastrointestinal Mouth, stomach, intestines, liver, pancreas Breaks food down so it can be absorbed 11
Genitourinary Kidneys, ureters, bladder, urethra, testes, ovaries Urinary- filters blood, stores and eliminates waste Organs of reproduction Nervous Brain, spinal cord, nerves Control & regulate all other systems 12
Muscular/Skeletal Muscles, tendons, cartilage, bones, connective tissue Support & protect organs & help with movement Skin & Sensory Organs Skin is largest organ / protective cover eyes, taste buds, olfactory system are senses 13
Heart & vessels, lungs, nose Transfer food (nutrients) & oxygen to cells Removes toxins from body Chronic conditions include cardiac disease, asthma, allergies, Things to monitor Breathing, runny nose/congestion, coughing, sore throat, allergic reaction, edema, chest pain, symptoms of heart attack, stroke When to call 911 14
Brain, spinal cord, nerves Regulate all other systems Things to monitor (pp 19-22) Seizures (individualized), delirium (confusion), dizziness, fainting, headaches, head injuries, insomnia, level of consciousness, paralysis, tremors 15
Mouth, stomach, intestinal track, pancreas, liver Breaks down food so it can be used by the body Rids body of solid wastes Things to monitor Know the person well Appetite, mouth & teeth, heartburn & gas, nausea & vomiting, abdominal discomfort, stood (feces), constipation, diarrhea (different from loose stool), hemorrhoids, poisoning 16
Urinary = kidneys, ureters, bladder, urethra Genital = testes & ovaries - reproduction Regulates balance of liquids taken in and eliminated Average daily intake and output = 3 quarts Things to monitor Urinary tract infections (UTI), urine, painful urination, discharge (drainage), genital itching, dehydration, sexual organs for males and females 17
Muscles, cartilage, tendons, bones, connective tissue Framework of body, support & protection, mobility Things to monitor Unusual gait, muscle tone, sprains, strains, fractures, pain or swelling in the joints 18
Largest organ of the body Protective covering over entire body Faster a new symptom develops, the more urgent the problem see a doctor Wounds = cuts, scrapes, punctures Abrasion= outer layer of skin worn away Cut= layers separated Laceration=torn or jagged wound Puncture= usually closes high risk of infection 19
Wound infection some populations are at higher risk to develop infection who? Things to monitor: Pain, swelling, redness, warm to touch, pus, elevated temp Human & Animal bites Rarely fatal Check bite characteristics 20
Burns: What are some ways people get burned? Never use ointment unless Dr says so Things to monitor: (pp 32) Red and painful, Blistering Skin charred or crusted What was the cause 21
Chills/Cold Extremities: Caused by rapid muscle contractions & relaxing Way for body to generate lost heat What to monitor (pp 32) Body temp, is shivering involuntary, frequent chills, how long does it last, skin color, what is the outside temp, how is the person dressed, is there an elevated temp, what other symptoms 22
Frostbite: damage to skin & tissues due to cold Who is more susceptible: What to monitor (pp 33) Environment, clothing, condition of skin Heat: Heat cramps, heat exhaustion, heat stroke Body becomes overheated What is our policy? (pp 33) 23
Insect bites & stings Most reactions are not serious What to monitor Itching, swelling, fever, hives, joint/gland pain When should you call 911? Rash Irritated or swollen skin What to monitor (pp 33-34) Redness, itchy, bumpy, scaly, crusty, blistered, color, body part involved, exposure to ? Reaction times vary with type of irritant 24
Fever Normal body temp is 98.6 F So what s different? (pp 34) Skin Color Changes What s normal for this person? (pp 34) Other Skin Changes (pp 34-35) Is it part of the aging process? New growth? Sores heal properly? 25
Ears Tinnitus ringing in the ears Meniere s disease fluid in the inner ear Symptoms? (pp 35-36) Eyes Diabetes is the #1 cause of blindness in US Pain, redness, changes in vision Symptoms? (pp 36) Nose Filters air, warms & moistens it After age 50, taste and smell diminish (pp 37) 26
Life Threatening (pp 44) When should you seek immediate medical help? Reporting Health Threatening Situations Contact supervisor & Use common sense Pay attention to what you see & hear Like what? Pain Threshold Different for everyone Communicating Illness How do people tell others they aren t well 27
Infectious Process: 4 components (parts) Invading organism: virus, bacteria, fungus, parasite Host: provides a place to live and multiply Humans, animals, non-human/non-animal (dirt) Method of Escape: respiratory tract, intestinal, genitourinary tract, blood or body fluids, skin break New vulnerable host: 28
For the invading organism to be infectious depends on: 1. Amount of the invading organism present at exposure time 2. length of time the host is exposed to the organism 3. Person s overall physical and emotional health and the body s ability to fight off the infection 29
Primary goal is to protect others from infectious diseases Second goal is to provide early detection, intervention & referral 30
A. Standard Precautions B. Immunizations C. Early Detection, Intervention & Referral 31
Meant to reduce transmission Protect both DSP s and person infected Used for all persons at all times Protective barriers: gloves, masks, gowns Needed when contact w/ blood or body fluids is likely Hand Hygiene: most important technique is to wash hands Avoid Accidental Cuts Environmental Controls - Usually routine house- cleaning will be enough 1. 2. 3. 4. 32
Contaminated surfaces Cleaning contaminated food surfaces Contaminated laundry 33
Methicillin-resistant Staphylococcus aureus Common bacteria referred to as a Super Bug Spread by: Direct contact with infected person, sharing personal items, touching surfaces with MRSA on it Persons undergoing invasive surgery, weak immune systems Etc. Signs: bump or infected area that s red, swollen, painful, warm to touch, has pus or drains, fever 34
Basically blood or body fluid exposure Eyes, nose, mouth Flush exposed area w/ fresh water 3-5 minutes Needle stick or skin break Wash with soap & water 3-5 minutes Notify supervisor/nurse/ doctor 35
Vaccines: DPT, MMR, Hep B, Polio Vaccine C. Control thru Early Detection, Intervention, & Referral DSP s may be the first to notice changes Report to supervisor / nurse Ongoing tracking/monitoring/ reporting 36