Highlights from Imbrave150 Phase III Clinical Trial in HCC
Explore key findings from the groundbreaking Imbrave150 Phase III clinical trial comparing atezolizumab plus bevacizumab vs. sorafenib in unresectable hepatocellular carcinoma (HCC) patients. Discover exciting results on complete responses and trial design parameters presented in a virtual meeting by Dr. Amit Singal at ASCO 2020.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
MEETING SUMMARY ASCO 2020, VIRTUAL MEETING Dr Amit Singal, MD, MS UT Southwestern Medical Center University Hospital Surgical Oncology Clinic, Dallas, Texas, USA HIGHLIGHTS FROM HCC CONNECT May 2020 2
DISCLAIMER Please note: Views expressed within this presentation are the personal opinions of the author. They do not necessarily represent the views of the author s academic institution or the rest of HCC Connect group. This content is supported by an independent educational grant from Bayer. Disclosures: Dr Amit Singal has received honoraria from the following: Bayer, Eisai, BMS, Exelixis, Genentech, Merck, Roche, Exact Sciences, Glycotest, TARGET Pharmasolutions. 3
COMPLETE RESPONSES (CR) IN PATIENTS RECEIVING ATEZOLIZUMAB (ATEZO) + BEVACIZUMAB (BEV) VERSUS SORAFENIB (SOR) IN IMBRAVE150: A PHASE III CLINICAL TRIAL FOR UNRESECTABLE HEPATOCELLULAR CARCINOMA (HCC) Finn RS, et al. ASCO 2020. Abstract #4596. Poster presentation 4
TRIAL DESIGN IMbrave150 (NCT03434379): Randomized phase 3 trial assessing combination therapy with the PD-L1 inhibitor atezolizumab and the VEGF inhibitor bevacizumab versus standard-of-care sorafenib in first line for advanced HCC Key eligibility criteria Stratification criteria Region: Asia (excluding Japan) or rest of world atezolizumab 1,200 mg IV q3w + bevacizumab 15 mg/kg IV q3w Locally advanced metastatic or unresectable HCC Until loss of clinical benefit or unacceptable toxicity ECOG PS 0 or 1 ECOG PS 0-1 Survival follow-up R 2:1 Presence or absence of macrovascular invasion or extrahepatic spread (Open label) No prior systemic therapy sorafenib 400 mg BID No bleeding or high risk of bleeding Baseline AFP < 400 or 400 ng/mL (n = 501) Co-primary endpoints OS IRF-assessed PFS per RECIST 1.1 Secondary endpoints include IRF-assessed ORR per RECIST 1.1 and HCC mRECIST PROs Exploratory PRO endpoints Time to deterioration of symptoms Patients (%) with clinically meaningful change in QoL and physical and role functioning The abstract covers the description of responders who had a confirmed CR to atezolizumab + bevacizumab AFP, alpha-fetoprotein; BID, twice a day; CR, completer response; ECOG PS; Eastern Cooperative Oncology Group performance status; HCC; hepatocellular carcinoma; IRF, independent review facility; IV, intravenous; (m)RECIST, (modified) Response Evaluation Criteria In Solid Tumours; ORR, objective response rate; OS, overall survival; PD-L1, programmed death-ligand 1; PFS, progression-free survival; PRO, patient-reported outcome; q3w, every 3 weeks; QoL, quality of life; R, randomization; VEGF, vascular endothelial growth factor Finn RS, et al. N Engl J Med 2020;382:1894-905 5
RESULTS: IN THE ITT POPULATION Data cut-off date: 29 August 2019; median survival follow-up: 8.6 months atezolizumab + bevacizumab (n=336) sorafenib (n=165) Median OS (95% CI), months NE 13.2 (10.4-NE) OS, HR (95% CI) 0.58 (0.42-0.79) P value <0.001 Median PFS (95% CI) per IRF RECIST v1.1, months 6.8 4.3 (5.7-8.3) (4.0-5.6) PFS, HR (95% CI) 0.59 (0.47-0.76) P value <0.001 ORR per IRF RECIST v1.1, % 27 12 P value <0.001 CI, confidence interval; HR, hazard ratio; IRF, independent review facility; ITT, intention to treat; NE, not evaluable; ORR, objective response rate; OS, overall survival; PFS, progression-free survival; RECIST, Response Evaluation Criteria in Solid Tumours Cheng A-L, et al. Ann Oncol 2019;30(suppl 9):abstract LBA3; Finn RS, et al. N Engl J Med 2020;382:1894-905; Galle PR, et al. J Clin Oncol 2020;38(suppl 4):abstract 476 6
RESULTS: IN PATIENTS WHO HAD A COMPLETE RESPONSE atezolizumab + bevacizumab IRF RECIST v1.1 (n=18) IRF HCC mRECIST (n=33) Median (range) time to first response (CR or PR), months 2.8 2.8 (1.2-9.7) (1.2-7.2) Median (range) time to CR, months 5.7 4.2 (1.2-11.3) (1.2-11.3) Patients without progression or remaining alive at cut-off date, n (%) 17 (94) 31 (94) Time to progression, months Median (95% CI) NE (NE-NE) NE (NE-NE) Range 1.3+ to 13.0+ 1.3+ to 13.0+ 6-month analysis Patients remaining at risk 10 21 Event-free survival (95% CI), % 94 (83-100) 97 (91-100) CI, confidence interval; CR, complete response; HCC, hepatocellular carcinoma; IRF, independent review facility; (m)RECIST, (modified) Response Evaluation Criteria in Solid Tumours; NE, not estimable; PR, partial response 7
CONCLUSION ATEZOLIZUMAB + BEVACIZUMAB: APPROVED BY US FDA ON 29 MAY 2020 AS FIRST-LINE SYSTEMIC THERAPY FOR ADVANCED HCC IMbrave150 demonstrated a statistically significant improvement in OS and PFS with atezolizumab + bevacizumab versus sorafenib in the first-line setting in patients with advanced HCC Times to response were similar in the combination and sorafenib arms Response rates were significantly higher in the combination arm The trial was conducted in a patient population that had preserved liver function (Child Pugh class A) and a decreased risk of variceal bleeding. The safety of the combination in a broader population warrants further study In most patients who had a confirmed CR to the combination, CR was ongoing at 6 months, and a median CR duration has not yet been reached CR, complete response; FDA, Food and Drug Administration; HCC; hepatocellular carcinoma; OS, overall survival; PFS; progression-free survival Finn RS, et al. N Engl J Med 2020;382:1894-905 8
EFFICACY, TOLERABILITY, AND BIOLOGIC ACTIVITY OF A NOVEL REGIMEN OF TREMELIMUMAB (T) IN COMBINATION WITH DURVALUMAB (D) FOR PATIENTS (PTS) WITH ADVANCED HEPATOCELLULAR CARCINOMA (aHCC) Kelley RK, et al. ASCO 2020. Abstract #4508. Oral presentation 9
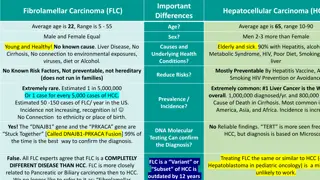
BACKGROUND Anti-PD-(L)1 and anti-CTLA4 antibodies Antitumour activity and durable immune response in subsets of patients with aHCC durvalumab (anti-PD-L1): ORR 10.0%; median OS 13.2 months tremelimumab (anti-CTLA4): ORR 17.6%; median OS 8.2 months Combination of anti-PD-(L)1 + anti-CTLA4 may improve clinical outcomes as shown in the initial cohort of Study 22 (phase 1) Phase 2 randomized expansion cohorts of Study 22 provide the first head-to-head comparison of mono- versus combination therapy in patients with aHCC aHCC, advanced hepatocellular carcinoma; CTLA4, cytotoxic T-lymphocyte-associated protein 4; ORR, objective response rate; OS, overall survival; PD-(L)1, programmed death (ligand) 1 10
TRIAL DESIGN Study 22 (NCT02519348): randomized, open-label, stratified phase 2 study Part 2A Part 3 Randomised Key eligibility criteria D (n=40) T300 + D (n=65) Unresectable HCC T (n=36) Randomized D (n=64) Immunotherapy na ve T75 + D (n=39) T (n=33) Either progressed on, intolerant to, or refused treatment with sorafenib or another approved TKI Part 2B T75 + D (n=45) Safety run-in T300 + D (n=10) Allocated Treatments and regimens T300 + D: tremelimumab300 mg, 1 dose + durvalumab1,500 mg q4w T75 + D: tremelimumab75 mg x 4 doses + durvalumab1,500 mg q4w D: durvalumab1,500 mg q4w T: tremelimumab750 mg q4w, 7 doses; q12w thereafter Primary endpoint: safety Key secondary endpoints: OS, ORR, DoR D, durvalumab; DoR, duration of response; HCC, hepatocellular carcinoma; ORR, objective response rate; OS, overall survival; q4w, every 4 weeks; q12w, every 12 weeks; T, tremelimumab; TKI, tyrosine kinase inhibitor 11
RESULTS: PRIMARY ENDPOINT (SAFETY) T300 + D (n=74) D T T75 + D (n=82) Event, n (%) (n=101) (n=69) TRSAE (including events with outcome of death) 12 (16.2) 11 (10.9) 17 (24.6) 12 (14.6) TRAE with outcome of death* 1 (1.4) 3 (3.0) 0 1 (1.2) TRAE leading to discontinuation of study treatment 8 (10.8) 8 (7.9) 9 (13.0) 5 (6.1) TRAE requiring systemic steroids 18 (24.3) 10 (9.9) 18 (26.1) 20 (24.4) *T300 + D arm: pneumonia; D arm: pneumonia, hepatic failure, abnormal hepatic function; T75 + D arm: hepatic failure Treatments and regimens T300 + D: tremelimumab300 mg, 1 dose + durvalumab1,500 mg q4w T75 + D: tremelimumab75 mg x 4 doses + durvalumab1,500 mg q4w D: durvalumab1,500 mg q4w T: tremelimumab750 mg q4w, 7 doses; q12w thereafter D, durvalumab; q4w, every 4 weeks; q12w, every 12 weeks; T, tremelimumab; TRAE, treatment-related adverse event; TRSAE, treatment-related severe adverse event 12
RESULTS: SECONDARY ENDPOINTS (EFFICACY) T300 + D (n=75) D T T75 + D (n=84) (n=104) (n=69) OS, median (95% CI), months 18.73 13.57 15.11 11.30 (10.78-27.27) (8.74-17.64) (11.33-20.50) (8.38-14.95) Survival rate 60.3 51.2 60.2 49.2 12 months (95% CI), % (47.9-70.6) (40.8-60.8) (47.3-70.9) (37.9-59.6) 52.0 35.3 45.7 34.7 18 months (95% CI), % (38.9-63.6) (25.0-45.8) (32.8-57.7) (24.4-45.2) 24.0 10.6 7.2 9.5 ORR (95% CI), % (14.9-35.3) (5.4-18.1) (2.4-16.1) (4.2-17.9) Median DoR, months NR 11.17 23.95 13.21 PFS, median (95% CI), months 2.17 (1.91-5.42) 2.07 (1.84-2.83) 2.69 (1.87-5.29) 1.87 (1.77-2.43) Treatments and regimens T300 + D: tremelimumab300 mg, 1 dose + durvalumab1,500 mg q4w T75 + D: tremelimumab75 mg x 4 doses + durvalumab1,500 mg q4w D: durvalumab1,500 mg q4w T: tremelimumab750 mg q4w, 7 doses; q12w thereafter CI, confidence interval; D, durvalumab; DoR, duration of response; NR, not reched; ORR; objective response rate; OS, overall survival; PFS, progression-free survival; q4w, every 4 weeks; q12w, every 12 weeks; T, tremelimumab 13
CONCLUSION Safety profile acceptable in all arms T300 + D provides promising clinical activity in a predominantly second-line setting in HCC ORR per RECIST v1.1: 24% in T300 + D arm Median OS (95% CI): 18.73 (10.78-27.27) months T300 + D and D are under evaluation versus sorafenib in the ongoing phase 3 HIMALAYA study (NCT03298451) IF HIMALAYA CONFIRMS THESE RESULTS, THIS COMBINATION COULD BECOME A NEW FIRST-LINE SYSTEMIC THERAPY OPTION FOR PATIENTS WITH ADVANCED HCC Treatments and regimens T300 + D: tremelimumab300 mg, 1 dose + durvalumab1,500 mg q4w D: durvalumab1,500 mg q4w CI, confidence interval; D, durvalumab; HCC, hepatocellular carcinoma; ORR; objective response rate; OS, overall survival; q4w, every 4 weeks; RECIST, Response Evaluation Criteria in Solid Tumours; T, tremelimumab 14
DONAFENIB VERSUS SORAFENIB AS FIRST-LINE THERAPY IN ADVANCED HEPATOCELLULAR CARCINOMA: AN OPEN-LABEL, RANDOMIZED, MULTICENTER PHASE II/III TRIAL Bi F, et al. ASCO 2020, Abstract #4506. Oral presentation 15
BACKGROUND Sorafenib = standard of care in first line for advanced HCC Lenvatinib approved in first-line setting based on non-inferiority to sorafenib No other monotherapy treatment option improves OS vs sorafenib Donafenib = deuterated derivative of sorafenib In a phase 1b study, donafenib 200 mg BID was well tolerated Phase 2-3 trial assessing non-inferiority or superiority of donafenib vs sorafenib Primary endpoint OS Secondary endpoints PFS ORR DCR and Safety donafenib (200 mg BID) Key eligibility criteria Advanced HCC ECOG PS 0 or 1 1 measurable lesion Until intolerable toxicity or PD (RECIST v1.1) 1:1 sorafenib (400 mg BID) (n=668) In 37 sites in China BID, twice a day; DCR, disease control rate; ECOG PS, Eastern Cooperative Oncology Group performance status; HCC, hepatocellular carcinoma; ORR, objective response rate; OS, overall survival; PD, progression of disease; PFS, progression-free survival; RECIST, Response Evaluation Criteria in Solid Tumours 16
RESULTS Baseline characteristics: Most patients were BCLC stage C (87.2% of donafenib and 87.6% of sorafenib group) and had HBV (89.3% of donafenib and 90.9% of sorafenib group) donafenib (n=328) sorafenib (n=331) Efficacy parameters HR (95% CI) P value Median OS (95% CI), months 12.1 10.3 0.831 0.0363 (10.3-13.4) (9.2-12.0) (0.699-0.988) Median PFS (95% CI), months 3.7 3.6 0.909 0.2824 (3.0-3.7) (2.4-3.7) (0.763-1.082) ORR, n (%) (95% CI), % 15 (4.6) (2.6-7.4) 9 (2.7) (1.3-5.1) 0.2448 DCR, n (%) (95% CI), % 101 (30.8) (25.8-36.1) 95 (28.7) (23.9-33.9) 0.5532 donafenib (n=333) sorafenib (n=332) Safety parameters P value AEs grade 3, n (%) 191 (57.4) 224 (67.5) 0.0082 Drug-related 125 (37.5) 165 (49.7) 0.0018 AEs, adverse events; BCLC, Barcelona Clinic Liver Cancer; CI, confidence interval; DCR, disease control rate; HBV, hepatitis B virus; ORR, objective response rate; OS, overall survival; PFS, progression-free survival 17
CONCLUSION DONAFENIB COULD BECOME AN OPTIMAL FIRST-LINE MONOTHERAPY FOR ADVANCED HCC WHERE COMBINATION OPTIONS ARE NOT AVAILABLE Donafenib demonstrated OS superiority versus sorafenib in patients with advanced HCC (12.1 versus 10.3 months) Donafenib versus sorafenib in PFS, ORR, and DCR: no significant differences Safety profile of donafenib, compared with sorafenib, is favourable DCR, disease control rate; HCC, hepatocellular carcinoma; ORR, objective response rate; OS, overall survival; PFS, progression-free survival 18
A PHASE IB STUDY OF LENVATINIB (LEN) PLUS PEMBROLIZUMAB (PEMBRO) IN UNRESECTABLE HEPATOCELLULAR CARCINOMA (uHCC) Zhu AX, et al. ASCO 2020. Abstract #4519. Poster Presentation 19
BACKGROUND Lenvatinib (TKI) is approved for the first-line treatment of advanced HCC Pembrolizumab (anti-PD-1) is approved as second-line therapy after sorafenib for advanced HCC (only in the US) Phase 1b trial of lenvatinib and pembrolizumab in combination in advanced HCC (n=104) Primary endpoints: Safety and tolerability (part 1) ORR and DoR (part 2) Key secondary endpoints: PFS TTP OS Part 1: DLT evaluation (n=6) Patients ineligible for other therapies Tolerability evaluated by DLTs during cycle 1 Key eligibility criteria Advanced HCC BCLC stage B or C ECOG PS 0 or 1 Part 2: expansion (n=98) No prior systemic therapy for advanced HCC Treatment: lenvatinib 12 or 8 mg daily orally + pembrolizumab 200 mg IV on day 1 (21-day cycle) BCLC, Barcelona Clinic Liver Cancer; DLT, dose-limiting toxicity; DoR, duration of response; ECOG PS, Eastern Cooperative Oncology Group performance status; HCC, hepatocellular carcinoma; IV, intravenously; ORR, objective response rate; OS, overall survival; PD-1, programmed death 1; PFS, progression-free survival; TKI, tyrosine kinase inhibitor; TTP, time to progression 20
RESULTS Data cut-off date: 31 October 2019; 100 patients included in the first analysis n (%) Grade 3 Grade 4 Grade 5 Safety TRAE (n=100) 63 (63) 1* (1) 3** (3) * ** TRAE grade 5: acute respiratory failure or acute respiratory distress syndrome (1), abnormal hepatic function (1), and intestinal perforation (1) TRAE grade 4: leukopenia or neutropenia Parameter (for confirmed responders) (n=100) mRECIST per IIR RECIST v1.1 per IIR Efficacy ORR, n (%) / (95% CI) 46 (46) / (36.0-56.3) 36 (36) / (26.6-46.2) Median DoR (95% CI), months 8.6 (6.9-NE) 12.6 (6.9-NE) Median PFS, months / (95% CI) 9.3 / (5.6-9.7) 8.6 / (7.1-9.7) Median TTR (range), months 1.9 (1.2-5.5) 2.8 (1.2-7.7) Disease control rate, n (%) / (95% CI) 88 (88) / (80.0-93.6) 88 (88) / (80.0-93.6) Efficacy analysis set Median OS, months (95% CI) 22.0 (20.4-NE) CI, confidence interval; DoR, duration of response; IIR, independent imaging review; (m)RECIST, (modified) Response Evaluation Criteria in Solid Tumours; NE, not estimable; ORR, objective response rate; OS; overall survival; PFS, progression-free survival; TRAE, treatment-related adverse event; TTR, time to response 21
CONCLUSION IF THE ONGOING PHASE 3 TRIAL (LEAP-002, NCT03713593) OF LENVATINIB + PEMBROLIZUMAB VERSUS LENVATINIB MONOTHERAPY AS FIRST-LINE THERAPY FOR ADVANCED HCC PROVIDES COMPELLING RESULTS, THIS COMBINATION COULD BECOME A NEW COMBINATION TREATMENT OPTION IN THE FIRST-LINE SETTING Lenvatinib + pembrolizumab results in 1. Promising antitumour activity ORR 46% (by mRECIST) and 36% (by RECIST v1.1) Disease control rate 88% (mRECIST and RECIST v1.1) 2. No new or unexpected toxicities HCC, hepatocellular carcinoma; (m)RECIST, (modified) Response Evaluation Criteria in Solid Tumours; ORR, objective response rate 22
FINAL RESULTS OF A RANDOMIZED, OPEN LABEL, PERIOPERATIVE PHASE II STUDY EVALUATING NIVOLUMAB ALONE OR NIVOLUMAB PLUS IPILIMUMAB IN PATIENTS WITH RESECTABLE HCC Kaseb AO, et al. ASCO 2020. Abstract #4599. Poster presentation HCC, hepatocellular carcinoma 23
BACKGROUND In resectable HCC, surgical resection is associated with high recurrence rates No approved neoadjuvant or adjuvant therapies exist, and effects of neoadjuvant immunotherapy have never been reported in this setting in HCC Phase 2 open-label randomized trial to evaluate nivolumab (anti-PD-1) alone (arm A) or with ipilimumab (anti-CTLA4) (arm B) as perioperative treatment for HCC in patients eligible for surgical resection (NCT03222076) Week 0 2 4 6 10 12 14 16 18 20 22 24 Up to 2 years Preoperative nivolumab 240 mg IV q2w ipilimumab 1 mg/kg day 1 Postoperative nivolumab 240 mg IV q2w ipilimumab 1 mg/kg q6w (4 doses) Surveillance every 12 weeks until recurrence Surgery Primary endpoint: safety Secondary endpoints: ORR, pCR, and TTP CTLA4, cytotoxic T-lymphocyte-associated protein 4; HCC, hepatocellular carcinoma; IV, intravenously; ORR, overall response rate; pCR, pathologic complete response; PD-1, programmed death 1; q2w, every 2 weeks; q6w, every 6 weeks; TTP, time to progression 24
RESULTS 27 patients with resectable HCC randomized 21 patients underwent resection as planned Overall n=27 nivolumab (arm A) n=13 nivolumab + ipilimumab (arm B) n=14 pCR, n (%) 5 (19) 2 (15) 3 (21) Major pathologic response (necrosis effect 50 99%), n (%) 3 (11) 1 (8) 2 (14) Adverse events (grade 3)* 6 2 4 *Preoperatively: grade 3 ALT or AST elevation (n=2) in arm B Postoperatively Grade 3: lipase (n=1) or amylase (n=1) elevation in arm A and colitis definite (n=1) in arm B Grade 4: respiratory failure (n=1) in arm B ALT, alanine aminotransferase; AST, aspartate aminotransferase; HCC, hepatocellular carcinoma; pCR, pathologic complete response 25
CONCLUSION IF CONFIRMED, THESE DATA MAY CONTRIBUTE TO A PARADIGM SHIFT IN THE PERIOPERATIVE TREATMENT OF RESECTABLE HCC The phase 2 open-label randomized trial s primary endpoint (safety) is met Secondary objectives including pCR rate and TTP showed interesting results to be further investigated and validated HCC, hepatocellular carcinoma; pCR, pathologic complete response; TTP, time to progression 26
REACH HCC CONNECT VIA TWITTER, LINKEDIN, VIMEO, OR EMAIL OR VISIT THE GROUP S WEBSITE http://www.hccconnect.info A picture containing graphics, drawing A picture containing drawing A picture containing graphics, drawing A close up of a sign Description automatically generated Description automatically generated Description automatically generated Description automatically generated Follow the HCC CONNECT group on LinkedIn Watch us on the Vimeo Channel HCC CONNECT Email Follow us on Twitter @hccconnectinfo froukje.sosef@cor2ed.com 27
HCC CONNECT Bodenackerstrasse 17 4103 Bottmingen SWITZERLAND Dr. Froukje Sosef MD +31 6 2324 3636 froukje.sosef@cor2ed.com Dr. Antoine Lacombe Pharm D, MBA +41 79 529 42 79 antoine.lacombe@cor2ed.com Heading to the heart of Independent Medical Education since 2012